Trinus KF., Claussen C.-F.
Incorporating “Guidelines on Dizziness and space orientation disorders” by Neurootological & Equilibriometric Society Reg. (Bad Kissingen, Germany)
Prepared by International Intercollegiate Dizziness Working Party under the scientific supervision of Neurootological and Equilibriometric Society (Bad Kissingen, Germany).
NEUROOTOLOGICAL AND EQUILIBRIOMETRIC SOCIETY Reg. (NES)
The aims of the Society are: to promote clinical neurootology in practice and in the field of clinical research; inform doctors and paramedical interested in this field in making neurootological diagnosis, paying special attention to tests of functional equilibrium, audiometry, olfactometry and gustometry; standardize clinical methods of research and research equipment in the field of neurootology; create functional anthropometric standards in the field of neurootology; develop provisional principles of occupational medical character for employees recruited for occupations particularly straining the neurootological functioning of the senses; enable participation with the help of neurootological and medical advice in the development of new transport technologies and other technologies, where disorientation strain occurs; develop and advance the various approaches for treatment of the neurootological disorders.
CERTIFICATION IMPLEMENTATION STANDARDIZATION & EDUCATION COMMITTEE (CISEC) of the Neurootological and Equilibriometric Society certify International and National Dizziness Centers, monitor clinical effectiveness and perform expertise in the development of evidence-based guidelines as well as organization and report of multicentre comparative performance data. The work program is collaborative and multiprofessional, involving relevant societies and patient groups. CISEC is self-financing with funding from state budget, charities and other organizations.
Citation of the documents:
- Trinus K.F., Claussen C.-F. Guidelines on dizziness and space orientation disorders. Neurootology Newsletter, 2012, Vol. 9, № 1, 85p. ISSN 1023-6422 Author’s right Ukrainian Certificate #44450 from 25.06.2012
- Trinus KF., Claussen C.-F. International Clinical Protocol on Vestibular Disorders (Dizziness). Neurootology Newsletter, 2016, Vol. 10, № 1, ISSN 1023-6422
Copyright
All rights reserved. No part of this publication may be reproduced in any form (including reprinting, photocopying or storing it in any medium also by electronic means transiently or incidentally to other use of this publication) without written permission of the Authors who are copyright owners. Application for the copyright owners’ written permission to reproduce any part of this publication should be addressed to: trinus.konstantin@gmail.com
Contents
- Intercollegiate Dizziness working party
- Conflicts of interests
- Aim of the Protocol
- Evidence-base for the Protocol
- Search methods
- Assessment of the risk of bias
- Principles of Protocol formation
- Models underlying Protocol development
- Vestibular peripheral sensors
- Space orientation sensory tetrad
- Vestibular brain projections
- Symptoms of vestibular dysfunction
- Vestibulo-cortical projection investigation methods
- Vestibulo-motor projection examination methods
- Vestibulo-vegetative projection testing
- Vestibulo-limbic projection test studies
E. Evaluation of the disease severity
F. Prophylaxis of vestibular disorders
H. Chronic vestibular disorder
- Vertigo versus dizziness differentiation
- Types of vestibulo-sensory disorders
- Management of vestibular dysfunctions
I. Pharmacology of vestibular disorders
2. Therapy dependent from topography of pathology
- Peripheral structures pathology
- Brainstem vestibular nuclei dysfunction
- Midbrain vestibular nuclei dysfunction
- Subcortical vestibular nuclei dysfunction
- Cortical vestibular nuclei dysfunction
- Management of exact types of vestibular disorders
3. Outcome from vestibular lesion
A. Structure of Protocol
1. Intercollegiate Dizziness Working Party
Experts participated personaly or through the Internet communication: Aguilar, L. (Guatemala City, Guatemala); Aoki S., Arai Y. (Tokyo, Japan); Aust G. (Berlin Germany); Bertora G. O., Bergmann J. M. (Buenos Aires, Argentina); Biswas A (Kalkotta, India); Boniver, R. (Verviers, Belgium); Dejonckere P. H., Coryn C., Lebacq J. (Brussels & Louvain, Belgium); Goldstein B., Shulman A. (New York, USA); Hahn A. (Prague, Czech Republic); Kazmierczak H. (Bydgoszcz, Poland); Nagy E., Bencze G., Bencsik B. (Budapest, Hungary); Oliveira C. A., Holdeffer L., Venosa A. (Brasilia, Brazil); Rapponi G. (Milan, Italy); Said J., Izita A. (Mexico City, Mexico); Sakata E., Sakata H., Endo M. (Saitama, Japan); Seabra J. C. R. (Oporto, Portugal); Castillo R. (Lisbon, Portugal); Schneider D. (Würzburg, Germany); Szirmai A. (Budapest, Hungary); Tan U. (Adana, Turkey); Wada M. (Ichikawa, Japan). Cesarany A. (Milan, Italy), Diberardino F. (Milan, Italy), Alpini D. C. (Milan, Italy), Mattei V. (Milan, Italy), Besta C., (Milan, Italy), Matsushima J. (Sapporo, Japan), Tamas L. (Budapest, Hungary), Mavrogeni P. (Limassol, Cyprus), Sachiko Koitabashi (Tokyo, Japan), Őzgirgin N. (Istanbul, Turkey), Schőpfer F. (Hagen, Germany), Rohival R. (Kolkata, India), Bhandari A. (Kolkata, India), Endo M. (Saitama, Japan), Fushiki H. (Saitama, Japan), Kersebaum M. (Bad Kissingen, Germany), Patil N. (Sligo, Ireland).
2. Conflicts of interest
All working party members signed a form to declare any potential conflicts of interest with the Guidelines. Nearly all professionals worked for an organization whose work is related in some way to the guidelines. Details of appointments and affiliations are therefore listed. Financial interest information can be obtained on request from the Neurootological and Equilibriometric Society. The published evidence base and majority opinion (consensus) were deciding factors for the working and content of recommendations.
Commercial companies
All the members had undertaken consultancy, lecturing and research work for companies including IPSEN, HEEL, Hennig Arzneimittel, Berlin-Chemie, Esparma, and other. No members had any personal commercial interest (eg shares) with companies that could benefit from the protocols.
Charities
All the members held posts within different charities.
Developing organizations
Neurootological & Equilibriometric Society Reg. (Bad Kissingen, Germany).
3. Aim of the Protocol
is to provide evidence basis for prophylaxis, diagnosis, management, rehabilitation and long lasing consequences avoidance for vestibular disorders. It has future-oriented recommendative character. It is prepared to show the National Societies, aiming to help the patients with Dizziness, Vertigo, Space Orientation and Related Disorders to create National and local Protocols according to the patient demands specifics and medicare facilities.
4. Evidence-base for the Protocol
Search methods
We have searched the Cochrane Ear, Nose and Throat Disorders Group Trials Register; Cochrane Central Register of Controlled Trials (CENTRAL); Society for Neuroscience; PubMed; EMBASE; CINAHL; Web of Science; BIOSIS Previews; Cambridge Scientific Abstracts; mRCT; LILACS; IndMed; China National Knowledge Infrastructure; CAB Abstracts; Runet; Google.
Protocol is adjusted to subject strategies for databases on the search strategy designed for CENTRAL. As much as possible we have tried to combine our subject strategies with highly sensitive search strategy designed by the Cochrane Collaboration for identification of randomized controlled clinical trials (The Cochrane Handbook for Systematic Reviews of Interventions. 2008, Version 5.0.1, Box 6.4.b.).
Assessment of the risk of bias
in the included studies though it appeared rather high in most studies; we have tried to orient the ideal proposed [119]:
- Certainty of diagnosis (types of participants);
- Adequacy of randomization process and of allocation concealment (A: adequate, B: uncertain, C: inadequate);
- Potential for attrition bias after allocation to study group, i.e., losses of participants to follow up and whether analysis is done intention-to-treat;
- Whether the trial is conducted and outcomes assessed in a double blind manner;
- Adequacy of compliance and its assessment;
- Quality of the assessment (types of outcome measures).
Studies are graded as A, B and C according to their methodological quality.
Principles of Protocol formation
The layout in any specific set of recommendations has to be:
- definition: identification of the problem;
- assessment: identifying or selecting patients for the subsequent recommendations;
- establishment: identifying the exact establishment and doctor for exact patient management;
- action: providing the actions needed;
- identification of patients needing further action;
- further action.
The Protocol use recommendations that have the following structure:
- Identification of the nosology.
- Symptoms of the nosology.
- Epidemiology.
- Etiology.
- Pathogenesis.
- Management and prognosis.
Protocol also supports next identifications:
- Target – identifies which patients, or people, or staff are the subject of the recommendation. It must be as specific as possible.
- Expect – recommendations are just that, indicating what we expect.
- Action – specifies what is expected.
- Qualifiers – additional qualifying comments to specify the particular goal of the action recommended. However, sometimes an alternative structure is used, specifying when a particular intervention is more preferable.
- Grade of the disease severity – establishment of the severity of the exact patient, based at the subjective and objective results.
- Hierarchy – identification requirements for the hospital managing patient of exact grade.
- Qualification – requirements for education and experience of the doctor according to the severity grade levels of patients to be managed.
Models underlying Protocol development
The Protocol uses next models to structure its layout. In summary these are:
- Stages of gravity establishment: criteria;
- Persistency of management: consequence of diagnostic, management and rehabilitation procedures;
- Hierarchy of doctors (from family physician to highly specialized team) and hospitals according to the disease severity grade of patient;
- Time: prevention, acute, subacute (recovery) and long-term;
- Healthcare process: diagnosis/assessment, goal setting, intervention (treatment and support), and re-evaluation;
- World Health Organization’s International Classification of Functioning (WHO ICF) (World Health Organization 2001) model (Wade & Halligan, 2004);
- Donabedian model (Donabedian 1978) for considering healthcare: structure, process, and outcome;
Structure, process, outcome
Protocol is intended to lead to the delivery of the most effective care to individual patients by considering efficiency. Consequently it primarily applies to individual interactions between the healthcare and the patient. The success of the Protocol depends upon influencing the decisions taken and actions performed by clinicians in patient–clinician interactions. These interactions are the mainstream process of healthcare. The fundamental processes in healthcare are similar whether considered as ‘prophylactic’, ‘medical’ or ‘rehabilitation’.
All are problem-solving processes that encompass:
- Data collection and interpretation (i.e. ‘assessment’ or ‘diagnosis’, both of which include drawing conclusions from the data)
- Goal estimating
- Decision – establishment of the severity of disease degree and cut-of whether to manage the patient or send it to higher level hospital
- Intervention (support and treatment; see below)
- Evaluation and reiteration or stop.
In this Protocol, the healthcare process itself is considered from two points of view:
System – characteristics established by medical professionals within particular locality. Protocol encompasses the hierarchy and consequence chain of healthcare management of the patient. This primarily refers to the use of protocols that guide the overall management strategies.
Person–patient interactions – used by individuals treating patients.
In this Protocol interventions are divided into two classes, each subdivided into two:
Support: actions needed to sustain the patient safely. They may have two goals:
- maintaining or sustaining; positively keeping the patient stable,
- preserving or preventing; actions that avoid adverse outcome happening.
Treatment: actions are expected to lead to a sustainable change in outcome. These may have two goals:
- restorative: aiming to reverse to a greater or lesser extent a loss or deficit;
- adaptive: aiming to manage the continuing consequences of a persisting loss or deficit.
Individual patient – team interactions are only possible within a structure, which means buildings, stuff, equipment and the organization needed to proceed them. Structure also encompasses other protocols or systematic approaches used.
In this Protocol three important aspects of structure are considered:
Organization, including hierarchy relationships between different levels of doctors and organizations (including transfer of patient).
Resources (eg who, how many, etc).
Location of delivery of service(s).
The outcome of the healthcare process refers to the actual state of the patient at the end of the process. It should also refer to the intended goals of the process. The imaginable wellbeing is kept in mind; protocol is based at the studies, lasting decades.
In this Protocol it covers:
- Audit of the whole system.
- Evaluation of professional-patient interaction.
- Patient interactions – WHO ICF.
The document uses the WHO ICF model especially as a basis for recommendations that relate to direct patient interactions. Thus, it is considered:
Pathology (disease); (e.g. vestibular lesion or dysfunction).
Impairment (symptoms/signs, e.g. vertigo, dizziness, acrophobia)
activities (disability)
participation (handicap)
context:
- physical
- social
- personal.
The date of the most recent search is May 28, 2016
B. Terminology
1. International Classification of Diseases (ICD) – 10 coding:
F40 Phobic anxiety disorders
F40.0 Agoraphobia
F40.2 Specific (isolated) phobias:
Acrophobia
Claustrophobia
Simple phobia
F41.00 Panic disorder
F4110 Generalized anxiety disorder (GAD)
F43 Reaction to severe stress, and adjustment disorders
F45 Somatoform disorders
F45.3 Somatoform autonomic dysfunction
Cardiac neurosis
Gastric neurosis
F45.4 Persistent somatoform pain disorder
• backache
• headache
H55 Nystagmus and other irregular eye movements
H57.0 Anomalies of pupillary function
H81 Disorders of vestibular function
H81.1 Benign paroxysmal vertigo
H81.3 Other peripheral vertigo:
H81.4 Vertigo of central origin
I95.1 Orthostatic hypotension
R11 Nausea and vomiting
R26 Abnormalities of gait and mobility
R27 Other lack of coordination
R29.3 Abnormal posture
R29.6 Tendency to fall, not elsewhere classified
Excl.:
accidents (X59.-)
difficulty in walking (R26.2)
dizziness and giddiness (R42)
R41 Other symptoms and signs involving cognitive functions and awareness
R41.1 Anterograde amnesia
R41.2 Retrograde amnesia
R41.3 Other amnesia
R42 Dizziness and giddiness
R45 Symptoms and signs involving emotional state
R53 Malaise and fatigue
R54 Senility
R55 Syncope and collapse
Blackout
Fainting
2. Definitions
SOD – space orientation disturbances – disturbance of perception, orientation and interaction with environment in space and time.
Dizziness – belongs to cognitive disorders, disturbance of perception of space, motion and time.
Vertigo – belongs to ear disturbances, illusion of non-existing motion.
Clinical symptoms are divided into vestibulo-sensory, vestibulo-motor, vestibulo-vegetative and vestibulo-limbic.
Delayed consequences of vestibular disorders – appear after few weeks or years after vestibular damage, after the end of the imaginable wellbeing period, and are characterized with irreversibility, organic nature of pathology, polymorphism, resistance to treatment.
Complications of vestibular disorders – often arterial hypertension, metabolic changes, and immune failure: chronic infections, autoimmune diseases and oncopathology, panic disorder, GAD [307, 308].
C. Scope of the problem
Dizziness is met in more then 20% of Global population. It appears to be the third reason of patient admittance to the doctor in USA [67]. According to Cochran reports a nationally representative sample of 4869 adults living in Germany being screened for dizziness, and 1003 individuals with dizziness underwent validated neurootologic interviews to differentiate vertigo from dizziness according to explicit diagnostic criteria.
Dizziness/vertigo has a prevalence of 22.9% in the last 12 months and an incidence (first episode of dizziness/vertigo) of 3.1%. For vertigo, the prevalence is 4.9% and the incidence is 1.4%. 1.8% of unselected adults consulted a physician in the last 12 months for dizziness/vertigo (0.9% for vertigo).
Other authors describe the situation as being even more pessimistic: 36% of females and 29% complaining. After 88-90 y.o. the figures increase to 51-45%, respectively [297]. In some countries they report the prevalence up to 39%, though these data have lack of evidence [132].
Compared with dizziness, vertigo is more frequently followed by medical consultation (70% vs. 54%; P<0.001), sick leave (41% vs. 15%; P<0.001), interruption of daily activities (40% vs. 12%; P<0.001), and avoidance of leaving the house (19% vs. 10%; P=0.001). More than half of the participants with “vestibular vertigo” reported “nonvestibular diagnoses”. Age and sex-adjusted health related quality of life was lower in individuals with dizziness compared with dizziness-free control subjects [153, 176].
1. Objectives
Cochran reviews suggest that the evidence base for dizziness evaluation and management is weak. Meta-analyses and systematic reviews are particularly important for clinicians because these studies design minimize bias and summarize evidence in a manner useful to clinicians. Only few guidelines give consensus support of the clinical utility of vestibular tests. Unique guidelines summarize important measures of diagnostic accuracy (e.g., sensitivity, specificity, and coherence) – the information which is the most useful when making medical decisions [131].
Almost no information exists about the use of this or that method for disease understanding or management strategies [274]. When the sensitivity and specificity of posturography was assessed by a meta-analysis design, both of these operating characteristics were only about 50% for identifying vestibular disorders – indicating that the test results do not influence the probability of the outcome [131].
Imaging studies are increasingly used in dizziness evaluations, but only some experimental results exist indicating their sensitivity as 30-40% [184]. No guidance is proposed to clinicians about who needs an imaging study.
In fact, none of the guidelines were even intended to be a clinical practice guideline for dizziness. Other than BPPV and Ménière’s disease, meta-analyses and systematic reviews were only found on alternative interventions [105]. The main purpose of the guideline on Ménière’s disease was to establish design and reporting criteria for research studies.
The statement on acoustic neuroma stems from a National Institutes of Health Consensus Development Conference – which aim to present useful consensus information to health professionals, but is not intended to be clinical practice guidelines [131].
The guideline on ischemic stroke only briefly addresses dizziness [113].
All this has lead to the next distribution of outcome between groups of patients being monitored dozens of years.
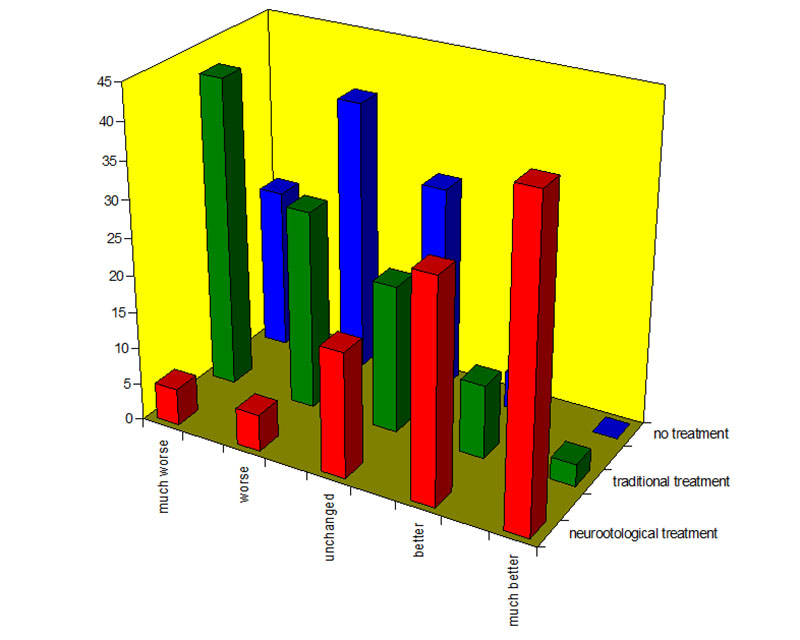
So, it might be seen that unprofessional management (green bars) is much worth, than no treatment (blue bars). Professional neurootologic treatment provides the best results [265].
Research should address questions such as, “Which dizziness patients are likely to benefit from having a brain image, vestibular test, audiogram, or blood analysis?” – Since these tests are expensive, inconvenient and often bothersome to patients, and are generally of very low yield. Evidence for interventions – including re-positioning for BPPV – is insufficient and for medication therapy is absent entirely [105].
Thus, more empirical studies, systematic reviews and meta-analyses on relevant dizziness topics are needed so that evidence is established in a way that will inform clinicians and also research agendas. Guideline statements can then be developed to transform evidence into actual recommendations for clinical care. With these goals as priorities, future work could make an important contribution to the efforts in optimization of patient care and healthcare utilization for one of the most common symptom presentations in the entire medicine [131].
Proposed in 2012 by Neurootological and Equilibriometric Society Consensus Expert Document “Guidelines on dizziness and space orientation disorders” [279] is decided to become the theoretical basis for creation of International Clinical Protocol on Vestibular Disorders (Dizziness).
This Protocol has recommendative and not obligation value and is proposed for development of the National and local protocols according to patient profile and local specifics and facilities.
2. Danger of vestibular disorder
Authors consider dizziness to be the predictor of severe diseases [277]. The course of sickness is the same in the cases of light head trauma [51], ionizing or electromagnetic radiation [266], vibration disease [177] or intoxication [191]. Most cunning feature of all the vestibular disorders is the fact that initial reaction transforms into the imaginable wellbeing. Both patient and doctor are sure that the disease is over – dizziness episodes disappeared.
But, during 25-years monitoring dizziness in Chornobyl clean-uppers, it has been shown that after the period of imaginable wellbeing primary peripheral distortion in two-three years starts to involve higher levels of brain [266], involving motor, vegetative and limbic systems, resulting in organic pathology: neurologic, cardiovascular, psychiatric [275]. When the process reaches brain cortex, the balance of cortical processes is disturbed, causing immune failure [177], which is finished with chronic, autoimmune and oncologic diseases [4].
In the cases of severe damage (severe head trauma, high doses irradiation) this process is running quickly, in moderate – it becomes chronic and long lasting, but its development is the same [263].
3. Concept of vestibular system
Dizziness is considered not to be separate disease, but symptom, which might be met either alone or associated with certain disease or group of nosologies. It accompany seasickness, meteosensitivity, diabetes and other metabolic disorders, hepatic dysfunction, it is met in gynecology: 14-15 years old girls, first trimester of pregnancy, and during climax; in the cases if cardio-vascular diseases, in postoperative period, in oncology, especially during chemotherapy, and as a result of stress, head trauma, intoxication or infection [249]. It may be of occupational origin in the form of vibration or monitor disease, the result of ionizing or electromagnetic fields irradiation [277].
In many cases it has functional and not organic character, among patients with dizziness complaints only in 29% the CT scans and in 40% MRI have shown abnormalities: atrophies, infarctions, demyelization [184]. In general being widely spread dizziness is not enough studied, often resistant to therapy and results in invalidity of patient [294]. Wide scale studies of dizziness, being done from 1974 till today by Neurootological and Equilibriometric Society, as well as knowledge accumulated by Barany Society and Society for Neuroscience, have lead to the concept of vestibular system, which involves the vestibular peripheral sensors, space orientation tetrad, vestibular presentations in the brain cortex and vestibular effectory projections in the brain.
Vestibular peripheral sensors
Each analyzer consists of peripheral sense organ and its pathways to specific cortical zone. Sense organ often consists of more than one sensor, providing high sensitivity to different stimuli of the same modality. For example, in the eye retina coni and baculi are met, which percept accordingly white and color lights, at least four types of sensors are described at the tongue, percepting salty, acidic, sweat and bitter tastes.
The structures, modulating sensitivity of peripheral organs are also present. In the ear – outer hair cells, in the eye – pupilla diameter regulating mechanisms, this provides fine tuning of sensitivity, protection from overexcitement, etc [85].
From this point of view vestibular organ is unique because of several reasons. Its peripheral end organ is a series of closed spaces, in which receptor structures are placed. Maculae with otoliths are located in sacculus, utriculus and lagena, while in the ampoules of semicircular canals – cristae and cupulae. Macula consists of otolith and sensory epithelium.
First is the mass of small crystals (otoconia), conglomerate, connected by otoconial membranes – thin protein ligatures. Cupula differs from macula by presence of only organic components; it resembles the sail, closing most part of canal ampoule. Main principle of vestibular inertial function is in the fact that mass, fixed at vivid spring, deflects proportionally to the acceleration applied.
Mutual position of maculas and cupulas is such that they cover all the possible movement directions, both angular and linear. Signal perceived is coded into pattern of spikes, action potentials, which in its turn is send to CNS [85]. Besides this, the structures named, also evaluate the changes of gravitational field direction, hypo, hypergravitation and weightlessness [216].
Gravitation sensor responds not only to the head position against gravitation field of the Earth changes, but also to microgravitation changes, occurring because of celestial bodies dislocations. These changes are enough to result in the displacements of giant ocean water masses. Many patients feel excitation, sleeplessness, headache spells, and anxiety during full moon days [169].
Microstructure of labyrinths has specific features. Among the others there are macular lacinias (macula neglecta), which have been first found in fishes [198]. They appear to be small macules distributed in sacculus and lagena and differ from ordinary macules by absence of gelatinous substance and otoconia. Hair cell cilia in these structures are most variable in length.
This feature gives the researchers possibility to estimate macula neglecta as being morphological structure for perception of low frequency whole body vibrations. Vibration perception as a separate modality is especially important for fishes and amphibians, for which these stimuli mean the approach of enemy or danger. In nature they are met during earthquake, storm, hurricane and have dangerous meaning.
Today cities are full of technogenic vibrations from underground, lorries, ventilations, etc. Among mammals maculae neglectae are described in cats’ family and in humans [83]. So, all this provide evidence for vestibular perception of low-frequency vibrations [252]. It is also important to note, that the cilia movement frequency being estimated as 7-10 Hz [242], thus explaining this frequency range to be the most horrifiable. In the activity of cilia they have identified Math1 as an essential gene for cilia movement in the hair cells and prestin – essential motor protein. The latter are considered to be serious breakthrough in the approach to management of hearing and vestibular function loss [20; 63].
It is shown that labyrinth is also percepting sounds [230]. In patients with destroyed cochlear it is possible to record flat audiogram proceeding from infrasound to 16 kHz and sensitivity threshold of 30-40 dBA [43]. Saccular hearing is also used now for, so called “vestibular evoked myogenic potentials”. Fine parameters of sound: frequency composition, direction, melody are seemed to be percept by hearing organ, and emotional (especially dangerous meaning of abrupt sounds) – labyrinth.
They discuss the importance of the fact of magnetic particles in fish otoliths [186]. These have been also found in labyrinths [223] and ethmoid sinuses of mammals. So, in the living organisms there are magnetic sensors; magnetic impulse perception system is related to macula as it is dynamic system.
Magnetic particles in ethmoid bones are supposed to have the function of magnetic compass indicating the direction of the magnetic field of the Earth, this system is rigid [10]. It is possible to make up conditioned reflexes to magnetic stimuli and memorize them [186, 298]. Evoked potential in response to electromagnetic field (EMF) stimulus have been recorded, thus proving the presence of pathway from periphery to cortex in the human brain [270]. It appears that moderate magnetic loading impairs coordination in magnetic sensitive patients, the fact indicating close relation of magnetic and vestibular senses [282].
The question arises, why don’t we perceive EMF like visual or auditory stimuli? The answer is possible after analysis of natural, non-technogenic magnetic impulses. These appear when clouds, usually negatively charged, are moving or thunderstorm discharges. In living nature the clouds appear before rain, which is resulting in being wet and energy loss.
During the rain time it is better to hide somewhere – therefore the biological sense of EMF impulse specific sensor is not to provide spectral-phase or amplitude parameters, but storm prediction. This provides explanation of weather change reactions – somnability, fatigue.
Tight connection of magnetic and vestibular sensors might also cause dizziness; disturbances in motor, vegetative, limbic vestibular projections are also possible. In this case becomes understandable the number of accidents in the days of solar storms or in geopathogenic zones. Modern people have changed the Earth, we live today in the condition of “magnetic smog”, which is covering the entire Globe and acting constantly at all the living beings. In the weakest persons it causes not the fatigue, but pathologic reactions – dizziness and imbalance, headaches, palpitations, nausea and vomiting.
Important finding is that animals with enucleated labyrinths stop reacting to emetics [170]. Moreover, analysis of literary data has shown that just vestibular system is mostly sensitive to both inorganic [191], and organic toxins [115]. Many industrial poisons result in vestibular dysfunction in concentrations, which do not influence any other organism function. Chemical reductive agents are increasing the sensitivity, oxidative – reduce it [248].
Mechanism of this phenomenon is disclosed in the studies of vestibular organ of snails. Perfusion of its hair cell cilia with reductive agents increases the cilia rigidity, oxidants – decrease. In both cases the mode of mechano-electric transduction changes [242].
Hair cell sensitivity to reductive oxidizing potential changes is 2-5 orders higher than that of all the other organism tissues [126, 253]! Data presented indicate that vestibular analyzer additionally plays the role of metabolism (condition of oxidative-reductive processes) sensor in the organism. In this context the correlation between vestibular sensitivity and radiation tolerance becomes understandable [90]. Ionizing irradiation cause the accumulation of peroxide products, changing vestibular function.
The more sensitive perceptive structure is, the earlier it switches on the compensatory mechanisms. From the other side it explains the identity of symptoms of kinetosis and intoxication. Penetration of the toxin into the organism excites the sensor in the labyrinth, which initiates the evacuation of toxin from the organism. Kinetosis or motion sickness is also overscale vestibular irritation [98; 115]. It also explains the dizziness, appearing in patients with diabetes, kidney disease, chemotherapy etc.
Resuming the data presented it is possible to estimate that labyrinth consists of set of sensors, for which six modalities of stimuli are adequate [277]:
- Acceleration,
- Gravitation,
- Low frequency whole-body vibration,
- Sound, including infrasound,
- Magnetic impulse,
- Metabolic changes.
Space orientation sensory tetrad
Dizziness belongs to space orientation disorders; therefore it is important to highlight the mechanisms of brain space perception. Role of the analyzers is found out with electrophysiological methods. Even at the level of rhomboid fosse the information inputs have been shown from the other sensory organs.
For example, 28% of vestibular neurons, responding to horizontal canal excitation, also react to hearing and somatosensory stimuli. Reaction is always being the increase of impulsation frequency. For somatosensory information its increase appeared to be greater, than for hearing (62-145% and 20% correspondingly).
Latencies of these responses being in the time frame of from 5 to 40 ms, indicating both oligosynaptic and polysynaptic pathways [34]. Vestibular nuclei neurons respond also to visual stimuli (65% of cells, responding to linear accelerations). This input has the signs of polysynaptic. Cooperative action of visual stimuli and linear accelerations results in phase shift in the direction of maximal accelerations [109].
Moreover, in this zone there are neurons (about 24%), responding to passive eye movements, i.e. from proprioceptors of oculomotor muscles. Latencies for these responses are from 6 to 30 ms, thus indicating several pathways with different amount of synaptic transmissions [8]. 14% of Deiters nucleus neurons react to cornea stimulation with enough short latencies (6-16 ms). It provides the reason to speak about special corneal connections with spinal motor system in the tight contact with vestibular.
Such complex fulfill coordinatory role, being the basis of nociceptive reflex, protecting face and eyes [159]. Studies of many other reflexes show their formation at the structures of rhomboid fosse [118].
Brainstem vestibular nuclei in reptiles are the highest brain level, like cortex in primates. Therefore, the data presented bring evidence that vestibular nuclei are forming the most ancient primary associative area of the brain in the meaning of space perception, orientation and movement coordination. Primary coordinating vestibular associative center of rhomboid fosse is localized at the connection of lateral portion of medial vestibular nucleus, medial portion of lateral vestibular nucleus and descending vestibular nucleus.
Physiological data reveal among other pathways intimate connections of this area with closely located vegetative centers, controlling blood redistribution, heart and breathing rate, during bending, standing up, locomotion and especially moving head up and down [28]. That is why big portion of orthostatic problems are related to the dysfunction of just this brain zone. In the space perception major role is played by upper brain structures: medial longitudinal fasciculus and lamina quadrigemina, where the direction estimation occurs [56].
Next is caudate nucleus and hippocampus, vestibular dysfunction results in their degeneration, which is manifested with spatial memory impairment and cognitive deficit [32; 235]. Subjects recognition, praxis, gnosis, cognition belong to cortical functions [302]. Total spatial disorientation is described, if cortex is the subject of lesion.
Analysis of the influence of different sensory inputs on the rhomboid fosse neuronal function has shown the major input of somatosensory and visual systems and less of hearing. This is depicted in the idea that space perception is formed by three sensory systems (triad): visual, somatosensory and vestibular [213].
The idea of space perception triad is basic for the whole diagnostic branch – posturography [117]. The other proposal is to regard hearing as important part of space orientation [56]. Phonation of patients during dynamic posturography allows revealing the acoustic dysfunction input into topography of dizziness and imbalance. Usually it appears at the level of rhomboid fosse and medial longitudinal fasciculus (MLF). At both locations acoustic and vestibular nuclei are tightly close.
Moreover, lateral longitudinal fasciculus (LLF) is considered to be the very place, where the direction of sound origin is determined. Destruction of either MLF, LLF or lamina quadrigemina results in the fail to determine sound direction. Thus, intersensory interaction might be useful for understanding of dizziness origin, hearing function providing information about sound, vestibular – integrating sound information into space orientation [277]. From the other side, visual-vestibular interaction studies in space microgravity provided much benefit to patients in the Earth conditions [142].
Psychophysical studies of healthy volunteers have revealed significant deficit of visual cortical activity during caloric test [162]. In PET studies optokinetic stimulation in patients with vestibular lesion causes much more active visual cortex response, than in healthy persons [69]. The authors have interpreted the data as competitive interaction between vestibular and visual stimuli, though it might be also regarded from the space orientation process point of view, which is not only competitive [56, 277].
Next question is “non vestibular dizziness” [176], “appearing somewhere in the eyes” [225]. Investigation of dizziness, appearing in the first hour of wearing of ‘improper’ glasses, have shown the excitation of the vestibular nuclei at the level of MLF or lamina quadrigemina, no visual nuclei function impairment is found [277]. These data provide evidence for the idea, that space orientation is formed at the vestibular nuclei as a result of integrative processing, first of all of the information from tetrad – four principal inputs: vestibular, visual, somatosensory and hearing [56].
There is a big bulk of literature proving that dizziness is related to vestibular dysfunction. Minor head trauma starts as a vestibular dysfunction [305]. Tinnitus is related to vestibular disturbances [226]. Low-frequency whole-body vibration cause vestibular damage [150; 260; 262].
In the patients with diabetes polymodal EP reveal peripheral nerves dysfunction, especially pronounced in vestibular peripheral organ [25]. Among arrhythmic patients 15-30% appeared to be vestibular-dependent [24]. Low doses of radiation cause primary vestibular damage which needs vestibular function correction [281]. The latter crucially improves the patient condition [265]. Vestibular dysfunction is present in dizzy patients with neurosis, encephalitis and epilepsy [269].
Early vestibular damage in Chornobyl clean-uppers (miners exposed also to vibrations) leads later to immune deficiency [177]. Monitoring of long-lasting consequences of patients with vestibular lesion has shown that primary peripheral distortion in two-three years spreads to higher levels of brain step-by-step involving motor, vegetative and limbic systems, resulting in organic pathology: neurological, cardiovascular, internal organs damage, including glands of inner secretion, psychiatric disturbances [229].
When the process reach brain cortex, the balance of cortical processes is disturbed, causing immune failure, this is finished with chronic autoimmune and oncologic diseases [275]. In the cases of severe damage (high doses irradiation) this process is running quickly [148], in moderate – it becomes chronic and long lasting, but its development is the same [263].
Vestibular brain projections
Labyrinth pathways within CNS structures are multiple and rather complicated. They differentiate several groups of them united into projections [147]:
- Vestibulo-cortical (sensory),
- Vestibulo-motor,
- Vestibulo-vegetative,
- Vestibulo-limbic [6].
Vestibulo-cortical projection
According to the physiological findings it is composed of at least three pathways [1; 277]:
- Three neuron shortest pathway to the contralateral hemisphere;
- Five neuron pathway to the ipsilateral hemisphere;
- Multineuron pathway to the contralateral hemisphere.
The first of them is initiated by the thick fibers, innervating big type I hair cells localized in the central part of the peripheral receptor [158]. The first orders neurons are presumably represent the crista-ampoular projections. The first transmission appears at the central part of the superior and partly in lateral vestibular nuclei [228].
Great neurons from this area are sending their axons to the ventral posterior area of thalamus, medial longitudinal fasciculus, Deiters nucleus and interstitial nucleus of Cajal. These second order neurons also send collaterals to the oculo-motor nuclei, being thus important nystagmus producer. Other electrophysiological data have revealed that vestibular responses might be found in the variety of somatic parietal areas (areas 2, 3a and 5). This input originates from great thalamic cells localized in oral portion of ventro-postero-lateral nucleus and ventro-postero-inferior nucleus. These nuclei in turn receive axon terminals from contralateral lateral and medial vestibular nuclei [84]. The latent time of this pathway is 3-5 ms if the vestibular nerve is stimulated directly in the electrophysiological experiment [1].
The second pathway seems to be initiated by mostly thin fibers innervating the II type small hair cells, dispersed at the peripheral parts of all the receptor structures [84]. The first order neurons are dispersed in all the vestibular nuclei of the brainstem. The pathway seems to pass through medial longitudinal fasciculus, Deiters nucleus and interstitial nucleus of Cajal, archicerebellum and striopalidum subcortical system [2; 84]. The latent time of this pathway is about 8 ms if the vestibular nerve is stimulated directly in the electrophysiological experiment [1].
Multineuron pathway or pathways to the contralateral hemisphere has been revealed in the evoked potentials studies. Cortical peak P2 has usual latency of 120-150 ms; the pathway seems to pass through the reticular formation [57]. PET studies have confirmed localization of vestibular cortical representation in parieto-insular zone of primates [91].
This projection represents the analyzer in its general physiologic understanding. In normal conditions the principal manifestations of its function are space perception, motion and time. Quantitative measure of its function is sensitivity threshold of the investigated subject [267]. Subjective sensation studies at the threshold level have revealed three types of sensations: undiscriminated, inverted and discriminated, which appear to be the fundamental feature of movement perception, no matter which the direction of movement is [18, 259].
Quantitative measure of gravitation perception is considered to be vertical estimation, which is to be performed in total darkness [38]. Dizziness, vertigo, being in general space orientation disorders are manifestations of sensory vestibular disorders. Attention has been payed to the fact of dominance of vestibular cortical function in the non-dominant hemisphere (PET studies) [69].
Nystagmus studies in patients during caloric stimulation have shown that vertigo is presumably formed while left labyrinth (right hemisphere) stimulation and dizziness – right labyrinth (left hemisphere) [280]. As vertigo is more strong sensation, it might imitate the vestibular dominance in non-dominant hemisphere in PET studies, cited above. In reality a wide spectrum of symptoms are produced during vestibular stimulation or pathology [272].
Vestibulo-motor projection
It is characterized by vestibulo-spinal and vestibulo-ocular pathways [84]. In norm it provides wonderful coordination we see in sportsmen, dancers, and cascadeurs. In pathology it is manifested with coordination disturbances, distortions of balance, gait (static and dynamic ataxia), nystagmus and saccades [249].
Vestibulo-vegetative projection
This one influences cardio-vascular system and inner organs [28]. In normal conditions provides vegetative reserve for normal function of the whole organism, in special conditions it enhances reconvalescence of postinfarctus patients [79], improve children physical development [134; 202]. Overloading of it causes kinetosis [56].
Vestibulo-vegetative projection in some vital reflexes, i.e. standing up in bipedal living beings, appears to manifest rigid behavior [28]. Its dysfunction may initiate different vegetative disorders: cardiac arrhythmia [24] and even arterial hypertension [278].
Vestibulo-limbic projection
Physiological vestibular stimulation results in improvement of life quality, in pathology it results in limbic disorders [277].
Symptoms of vestibular dysfunction
Taking into consideration the presented material about the projections of the vestibular system, now it is possible to identify the symptoms, which manifest vestibular disorder.
Vestibulo-cortical projection – vestibular analyzer – is the very brain structure, where the movement, space orientation and time perception is formed. In pathology we separate dizziness, vertigo [249], space [56] and time perception disorders [129]. Dizziness means the disturbance of the movement, space orientation and time perception.
The subjects feel themselves unstable or moving, the ground disappears, something is wrong in the head, sometimes it is heavy, sometimes it is somewhere in the glass sphere or it is impossible to explain what happens with this head [86]. Speaking about movement the patient, nevertheless, is unable to indicate the movement direction.
This condition might be accompanied with general inhibition or irritation; excitation is rather rare, but also possible, like the feeling after big dose of coffee. The time might be either dragged out or running too fast [128]. The example of the physiological time perception changes might be in the situation, when the car after driving in the highway at the speed of 140 km/hour is entering the city and the speed is decreased to 30-40 km/hour. It seems to move so slowwwwly!
Claustrophobia, agoraphobia, acrophobia, nyctophobia, orthostatics and optokinesis [49], discomfort while going up and down the staircase, ascendophobia and descendophobia, are also related to vestibular dysfunction, as spatial perception disorders [272].
Vertigo means the illusion of the non-existent movement [249]. In most cases the movement is rotatory like after carouser, less frequent is swinging or linear movement. It might be objective, subjective, giddiness [213] or kinetosis [189]. Usually, it accompanies acute cases of pathology and is combined with excitation or irritation and other additional symptoms: disequilibria, nausea, retching, up to consciousness loss [98].
Vestibular cortical representations
In the electrophysiological experiments the vestibular cortical area has been located in the anterior Sylvian sulcus posterior to the facial somatosensory zone and anterior to auditory cortex [194]. According to Brodmann’s classification this is the area 2V. Neurons in the area 2V respond actively to caloric and electric direct stimulation of labyrinth.
The pathway is bilateral, but contralateral features are strongly exaggerated. A second vestibular cortical projection area in humans is found in area 3 may represent the projection from the somatosensory arm field [35]. These data has been confirmed in 90th of 20 century with PET studies of primates [91] and humans [69].
Therefore, this part of the projection is supposed to represent the somatic afferents, involved into balance. Here, the integration of labyrinthine and somatic proprioceptive signals are providing the subject of awareness of body orientation. It is well known, however, that thalamic neurons transmitting vestibular information to parietal lobe also carry somatosensory signals, usually from proximal joints and muscles [84; 218].
Because many secondary vestibular neurons with canal input also receive visual information from the optokinetic system, this signal is also evaluated in CNS. Thus, the vestibular system is unique among sensory systems, because of its integrative function.
For example, head angular movements are based on information from a variety of sources including the labyrinth, the retina, the joint and the muscle receptors. Vestibular system, starting from rhomboid fosse level, is integrating sensory coordinator to produce effective movement of organism in space [56].
It has been shown that the orientation of visual cortical receptive fields might be changed by otolithic stimulation. In the other experiments the semicircular canals stimulation influences visual cortical background firing rates as well as the size of complex visual cortical receptive field.
Vestibulo-cortical pathway is necessary for spatial orientation and vestibular memory [2]. Humans and animals without labyrinths cannot remember a path through which they have been transported. Such orientation ability seems to be mediated via a pathway through the vestibular nuclei, the magnocellular medial geniculate body and the caudal caudate nucleus [83, 84].
Thus, the specific of the vestibular analyzer means small cortical representation area and presence of the vestibular projections in somatosensory, visual and auditory cortical zones, besides vestibular cortical area itself.
These projections seem to be based at the two parallel systems: type I hair cells-thick fibers-three synaptic pathways and type II hair cells-thin fibers-multisynaptic pathways [228]. They are the very substrate, where the sensations like numbness, black-outs, tinnitus of vestibular origin are formed [281; 285].
Vestibulo-motor projection is responsible for the coordination function and locomotion. In the formation of this function several systems take part, including vestibular, other sensory systems, vestibulo-motor pathways and motor effector system. The general coordination disorder terminology might be further detailed. In locomotion disorder swaying, staggering or stamped walk might dominate [56]. Static ataxia might be characterized by instability, swaying, and spastic disorder [213].
The patient might complain of momentary staggering, walking like drunkard, inability to fix the gaze, numbness, etc [249]. Pathologic eye movements, nystagmus and saccades, belong to the vestibulo-motor disturbances [208]. They are formed at paramedial pontine reticular formation. Such patients are complaining of visual disturbances, inability to concentrate, while reading and writing, poor contrast of the subjects even in normal visual conditions [14].
Different disorders appear in vestibulo-vegetative projection. Most typical are the disorders following motion sickness or kinetosis [98]. They are characterized by intensive nausea, retching and vomiting episodes [256]; usually they are accompanied by blood vessels spasms, palpitations, tachycardia, extrasystols [26; 192], sweating, spasms of esophagus, laryngospasms. Persons are complaining of dyspnoe, pain in epigastrium and bronchi [250].
They depend on the exact vestibular pathway and level of the pathological process location [31]. It might involve this or that internal organ, forming sometimes exotic versions of disease structure. An extraordinary example: patient complains that after about quarter an hour in city traffic the uncontrolled urination happens. The treatment proposed – dimenhydrinate before trip appeared to be successful – thus being the support of vestibulo-vegetative projection existence [277].
Special attention has to be attracted to headache of vestibular origin, which is called vestibular migraine [66]. Sometimes it is considered as a substitute of vertigo, sometimes as an additional symptom [102]. It might be complicated with other symptoms: nausea and vomiting, convulsions and even consciousness losses [250].
According to the WHO statistics 6% of male and 18% of female population of the Globe suffers from migraine attacks [101]. Epidemiological data report that vestibular migraine affects more than 1% of the general population, about 10% of the patients with dizziness and 9% patients with migraine [153; 175].
These data disagree with the previous data of the same authors indicating that 22.3% of German population suffers from dizziness [176], thus providing at least 2.20% of population suffering from migraine. The disagreement might be explained by the fact of subjective diagnosis estimation [237].
This means that the criteria of the vestibular migraine diagnostics have to be based at objective instrumental methods. Vestibular origin of migraine is established with the help of Vestibular EP, ECG and pupillometry with vestibular loading tests. It demonstrates good regression during therapy with the medications, correcting vestibular function, especially histamine blockers. Among the latter special attention attracts betahistine [277].
Vestibulo-limbic connections are least studied and today the data about their disturbances looks like preliminary studies from the point of view of evidence-based medicine. Nevertheless, pioneering physiological studies have attracted the researchers’ attention to this projection [6].
The clinical experience with Chornobyl clean-uppers has shown that up to 40% patients with dizziness are complaining of fears, nightmares and phobia [266]. This experience expands also to the patients with head trauma (including whiplash), poisoning and limbic disturbances triggered by kinetosis (sopit-syndrome, for example).
Sopit-syndrome has been described by American astronauts and is manifested with weakness, somnability, loss of initiative [204]. The correction of the vestibular function crucially influences the limbic symptoms, thus indicating its vestibular origin. Besides phobia and sopit-syndrome, limbic symptoms also include: disturbances of alimentary, drinking, sexual behavior, attacks of irritation, emotional lability, aggressiveness, etc [125].
Sometimes so called asthenization and related signs: chronic fatigue, weakness, loss of initiative, – might be the symptoms, indicating vestibulo-limbic disturbances. In severe cases depression and anxious disorders might develop at the basis of vestibular dysfunction [48].
The experience of aviation and space medicine has shown that being closely related from one side, from the other side the vestibular projections might be enough autonomic. It means that clearly expressed disturbances in one projection, might not be necessarily accompanied by the same expression of the disturbances in the other projections [147].
In the cases of chronic pathology it means that the situations are possible, when we have enough expressed dysfunctions in vegetative or limbic systems, with minor vestibular symptoms. These patients spend years visiting hospitals and ambulances, diagnostic centers, circulating between the doctors – all in wane, they need only the vestibular investigation and correction of the leading trigger of the disease.
The situation might be more pessimistic, because of patient might not relate poisoning, head trauma, visit of radar station several years ago with today palpitation episode or other dysfunctions [273].
D. Diagnostic methods
evaluation criteria proposed: method tolerability, sensitivity, specificity, coherence [131], providing knowledge about the disease, influence on management strategy and cost (proposed by the Authors). Some authors propose to evaluate price of patient management.
For example, in Poland they study benefit of the remedy as optimal relation of effectiveness to the price of medication [309]. In Norway [310] and Netherland [311] taking into consideration price, they nevertheless, mostly accentuate positive effect of the medication.
The authors of the Protocol also put forward the idea if the method provides knowledge about the disease, and how does it influence on management strategy.
Comparison of dizziness study methods are ruled out from the concept of the vestibular system, the most prominent components of which being the idea that the formation of all the dizziness types is related to the vestibular system, which is anatomo-physiologically organized into 4 principal projections: vestibulo-cortical (sensory), vestibulo-motor, vestibulo-vegetative and vestibulo-limbic [279].
According to this, vestibulo-cortical projection is to be investigated with the help of anamnesis, questionnaires and vestibular evoked potentials (vestibular EP, VestEP) (we don’t consider vestibular evoked myogenic potentials, VEMP, because it does not characterize signal propagation in the vestibulo-cortical projection).
1. Vestibulo-cortical projection investigation methods
Though in scientific literature dizziness is described with three-four terms: vertigo, imbalance, faintness and light-headedness [249], in reality it is much more variable [47]. Usually the disease initial phase is missed both by patient and the doctor. Everything starts from the dizziness attacks of little expression.
During several months their duration is increasing and intensity is growing. It starts being accompanied with unbearable headaches, nausea, vomiting episodes, up to conscious losses. At this point the patient admits to doctor, but in the general structure of the disease, dizziness is often ignored both by patient and doctor, because of “more important symptoms”. Only the accentuation of patient attention at the dizziness, he remembers that the sickness started just with it. Dizziness description by patients is full of difficulties in searching appropriate words to characterize their condition.
It is often subjectively percept as space or motion orientation disorders. They describe it as swimming, the ground is moving, the subjects are floating, or something wrong before eyes (eyes of glass, micropsia and macropsia) or in the head. Proposed to detailize clearly the floating direction or other its parameters, patients are not able to do this. Sometimes they describe their sensations as head being placed into glass sphere or helmet. Symptoms are provoked by head movements or during transportation in cars, underground or elevators.
They are usually accompanied by negative emotional perception of situation: patients feel fear of death, they complaint of feeling ill, fear of closed (claustrophobia) or opened (agoraphobia) spaces. Many patients complain of intolerance of certain kinds of traffic (kinetosis). Other patients tell about discomfort at height (acrophobia) insureness in the twilights and darkness (nyctophobia). They cannot track or gaze moving subjects (optokinesis), complain of balance disturbances, difficulties while descending from the hill or staircase (descendophobia), momentary black-outs and pushing aside [272]. Only 4-5% of them can clearly characterize vertigo, establish its direction, velocity and other parameters [176].
Among most popular questionnaires in vestibulology is NOASC. Its use is mostly profitable in statistical studies of wide contingents. There are two different ways of result interpretation. First is the most simple, when they calculate the percentage of patients having this or that complaint [22]. Second is Іe, expression index, which characterize the number of signs from this group (for example, headache types or dizziness parameters) in one patient. Expression index is calculated as ratio of certain group symptoms sum to the number of patients examined [266].
Additionally to NOASC the differentiation of vestibulo-sensory complaints may be quantified with the help of “Types of dizziness” Questionnaire [272].
Vestibular evoked potentials (VestEP)
VestEP mean responses, obtained from EEG with the help of synchronous summation. Industrial issue of the devices for VestEp recording (vestibular sensitivity analyzer – VSA) in 90th has been developed in Kyiv (Ukraine). Mostly the response to chair rotation of about 3° in 400-500 ms time window is recorded. Calculated average acceleration has been in the frame of 1-25°/s2. This acceleration range allows the head to follow the chair movement profile with great accuracy [73].
For long latency VestEP the 1-33 Hz frequency and amplification of 106.appeared to be the optimal recording conditions. 16-20 recordings with 10-15 s intervals appear to be enough for obtaining the expected signal. Literary sources indicate that with the intervals named for long latency evoked potentials habituation and sensibilization phenomena are absent, these conditions are considered to be optimal for cortical evoked potentials recording [182]. Diagnostically significant parameters are considered to be the latencies of principal extremums [215] in the frame of first 250 ms to 1 s from the stimulus initiation.
The results, obtained with this method disclose the topographic level of the disease; therefore these results are important for the management strategy [266]. The shapes of VestEPs are identical both for linear and angular stimuli [261] It is similar to the findings of acoustic evoked potentials [19]. EEG and BAEP sensitivity in the cases of vestibular disorders appeared to be 33% and 18% correspondingly [185], thus showing the high sensitivity and specificity of just vestibular EP in the case of vestibular dysfunction.
Normative data for VestEP: P1 – 20-40 ms, N1 – 60-80 ms, P2 – 120-150 ms, sensitivity threshold level at 4-15 cm/s2 and optimal diagnostic stimulus range – 15-20 cm/s2 [267].
The clinical value of this method is based at a big bulk of clinical studies and inventions being made at the basis of this method use.
One of the first interesting facts being established by Claussen and Schneider is the brain cortex mapping and monitoring the procedure of the cortical processing of the EP generation both in healthy persons and patients [58]. The movement sensation thresholds have been estimated with this method [267]. The other data are discussed in the following review [277].
The method is spread with success to several laboratories. The method is used now in Romodanov Neurosurgery Institute (Kyiv, Ukraine) [305], where they have obtained big amount of data studying the patients with suspicion to acoustic neurinoma and patients with head trauma. In Donetsk (Ukraine) the teams of Profs. Nikolenko and Lastkov have proved that vestibular lesions being the consequence of the professional hazard in miners, because of the combination of whole-body, local vibrations and intoxications [177].
In Kyiv the joint Ukrainian-Polish team with participation of Profs. Kazmierczak and Mierzwinski have studied the interaction of different sensory inputs during caloric stimulation and vestibular habituation [165]. The influence of chronic herpes on the vestibular function has been studied by Kaminskaya TA., et al. [123]. According to evidence-based medicine (EBM) Oxford center recommends the definitions of the information reliability level identification [120]:
- A. High reliability – information is based at the data of several independent clinical tests (CT) with coincidence of the data, summarized in the systematic reviews.
- B. Relative reliability – information is evidenced at the basis of at least several independent investigations, close to CT purposes.
- C. Limited reliability – information about one study results.
- D. The proofs are absent – idea is based at the expert’s opinion.
Method being independently initiated in at least three countries (Ukraine, USA, Germany) [258; 127; 57], passed verification procedure [271; 277] and evaluated by independent NASA experts [NASA Contractor Report 3922, №№ 13 & 23. USSR Space Life Sciences Digest, 1987 & 1988]. The results of coherence ratio are in the frame of 95%, thus making these data highly important from the point of view of evidence-based medicine. Sensitivity of method has been evaluated in comparison to the amount of persons complaining of dizziness (n=912 examinations, 672 patients) – 90.57%, specificity – 98.57% [274].
Anatomic and physiologic basis for establishment of vestibular origin of vertigo, dizziness and space orientation disorders is elaborated with complex of vestibular tests, including VestEP [272; 280]. Light head trauma starts as a vestibular dysfunction [305]. The positive influence of betahistine in the patients with peripheral vestibular disorders has been monitored with the help of vestibular evoked potentials [61].
Long-lasting consequences after Chornobyl accident, monitoring of patients has proved vestibular peripheral origin of dizziness [266]. Tinnitus is related to vestibular disturbances [226]. Low-frequency whole-body vibration cause vestibular damage [260; 262]. In the patients with diabetes polimodal EP reveal peripheral nerves dysfunction, especially pronounced in vestibular peripheral organ [25]. Among arrhythmic patients 15-30% appeared to be vestibular-dependent [24; 264]. Herpes virus infection in military stuff and their family members cause early vestibular damage [123]. Low doses of radiation cause primary vestibular damage, it needs vestibular function correction. The latter crucially improves the patient condition [265]. Early vestibular damage in Chornobyl clean-uppers (miners exposed also to vibrations) lead later to immune deficiency [177].
Evoked potentials (including vestibular) are used for differentiation of neurosis, encephalitis and epilepsy [269]. Vestibular evoked potentials appeared to be the only method for early reveal of vestibular nature of many disorders, especially in patients being at the period of imaginable wellbeing and start of delayed consequences, therefore it has great value from the point of view of the understanding of the nature of the pathologic process and its management [277].
Today, quantitative EEG [52], subjective vertical and PET [69] are also introduced into vestibular research, but yet we do not have any evidence-based information about evaluation of these approaches.
2. Vestibulo-motor projection examination methods
These tests are divided into two groups: vestibulo-spinal and vestibulo-ocular reaction tests.
Vestibulo-spinal reaction methods are based at the tests of Romberg [212], Unterberger-Fukuda and Uemura. Among first methods group most popular has become posturography, which means center of gravity (mass) displacements recording. It is based at the weight evaluation with the help of tensosensors, same to those used in the flour weights. While posturography performing, the patient is proposed to stand at the special platform, and three tensosensors are demonstrating dynamic patient weight redistribution between them [117].
Usually 6 test procedures are performed 20 s each:
- standing with eyes opened at stable platform;
- standing with eyes closed at stable platform;
- standing with eyes opened at stable platform, vision perturbed with moving picture.
Than the platform is descended, it appears to be hanged at the springs and the same test procedures are repeated. Results are reflected as the square of mass center movements, the percentage of increase in the particular test corresponds to the degree of exact disturbed sensory function decrease [174].
It is understandable that square increase while eyes closing corresponds to vestibular dysfunction, while eyes opened – to visual, at hanged platform – somatosensory, during moving picture demonstration – dependence from vision. The more difference between tests results, the more expressed is the disturbance of particular function [23]. The next step, phonation, also being proposed, based at the idea of sensory tetrad (four sense organs forming space orientation: vestibular, hearing, vision and proprioception) [56].
Stereo headphones are put at the patient’s head with melody running from one ear to another and above mentioned procedure being repeated. Patient phonation might either enhance balance performance or impair it [274].
Proposing many positive features posturography does not consider strategy of patient body and extremities movements while balancing, such as bending head, neck or knees, throwing hands forward or stepping.
The unique point is evaluated – mass center displacement. Therefore, the amount of information is limited, thus decreasing its diagnostic value. According to the literary data its sensitivity is between 35 and 54% and specificity up to 90% [70]. Our preliminary data coincide with the opinion of the author: sensitivity related to the amount of patients complaining of dizziness is 37.04% (n=54). The sensitivity of Uemura and Fukuda tests for the same patient group appeared to be 98.15% [274].
Equipment for posturography is enough expensive – prices exceed the amount of 200 thousand $ [67]. Today, scientific progress proposes the possibility to obtain even more information with the help of simple and cheap technical support. To understand the idea let us first analyze cranio-corpo-graphy method. The latter means that markers (light emitting diodes or ultrasound markers) are fixed at the head and shoulders of the patient and then they perform Romberg and Unterberger tests.
The resulting movement patterns of the head and body are recorded and allow the findings to be evaluated directly during or just after the measurement. Unterberger stepping test means marching at a spot with eyes closed (100 steps or 1 min.) [288]. The interpretation is based at the measuring of amplitudes for head and shoulders sways (separately), linear and angular displacement and rotation [50]. Sensitivity of this test is 82.89%, and specificity – 99.78% (n=912) [274].
Prof. Uemura has proposed the test of standing on one foot with eyes closed, as an express-test for vestibular function evaluation [287]. Its sensitivity appeared to be of 98.90% (n=912) [274]. The shortcoming of it is that it is not informative alone in the cases of low extremities diseases. To overcome the obstacle 20-point test battery has been proposed for express-diagnostics of coordination function [284]. According to recent literature postural control during one-legged stance is compromised in elderly adults with osteporosis and osteopenia (Boer et al., Eur J Phys Reahbil Med 2014).
20-point test battery for express-diagnostics of coordination function [after 266].
Complaints quantification. Dizziness attacks are considered to be significant when their duration is more than one minute and frequency is more than once per month. They also take into consideration additional symptoms: headache, black-outs, nightmares, tinnitus, memory problems, depressions and consciousness losses, as well as weakness, fatigue, loss of initiative, time perception changes, etc., related to dizziness attacks. Out of vegetative symptoms nausea, retching, vomiting, diarrhea, sweating, palpitations are most common [48; 287].
Standardized results are described as following:
- 0 points – complaints are absent;
- 1 point – complaints of dizziness (or vertigo) which duration exceeds 1 minute;
- 1 – complaints of dizziness (or vertigo) which frequency exceeds once per month;
- 1 point – complaints of accompanying symptoms. Possible signs combination might be expressed in figures from 0 to 3.
Uemura test is performed in 4 steps:
- standing at two feet with eyes opened;
- standing at two feet with eyes closed;
- standing at one foot with eyes opened;
- standing at one foot with eyes closed.
It is recommended to perform the test at each foot separately, the best performance is taken into account. If the patient is stable at one foot with eyes closed more than 10 s he is considered to be healthy.
Uemura test is evaluated in 5 point score:
- 0 points – patient is stable 10 s with eyes closed at one foot;
- 1 – undulating moderately, but keeping balance;
- 2 – hands are need to keep balance (hand is reaching shoulder level);
- 3 – cannot stand at a spot or stands 3-10 s;
- 4 – cannot stand at one foot even 3 s;
- 5 – cannot stand even at two feet.
Lateralization of displacements and falls are sometimes important.
Stepping (walking) Fukuda test. At the flour three concentric circles are painted with diameters of 0.5 m, 1 m and 1.5 m. In these circles they direct four perpendicular lines. Patient is proposed to stand in the very center and align himself with one of the lines. Then he is asked to make 100 steps at spot with eyes closed [81].
Three principal parameters are considered during test performance:
- displacement distance;
- displacement angle;
- spin (rotation) angle.
Normal is forward linear displacement at the distance of 0.2-1.0 m, angle up to 300 and rotation up to 300. Displacement absence or backward displacement, especially with large sway is regarded as disturbance. Displacement direction might indicate lateralization of the lesion.
Test evaluation is proceeded with three score system:
- 0 – points forward displacement at distance of 0.2-1.0 m, displacement and spin to the angle up to 300;
- 1 – displacement less than 0.2 m or more than 1.0 m;
- 1 – displacement at the angle more than 300;
- 1 – spinning at the angle more than 300.
Note: sometimes it is useful to make correction of normative, according to the height and step length of the patient.
Fukuda writing test. Patient is proposed to write “33” in column with eyes closed [287]. For healthy individuals it is easy going.
Standardization of the results looks as following:
- 0 – column is strait;
- 1 – column is undulating;
- 2 – column decline more than 300;
- 3 points – dismetria.
Tracking means that patient is proposed to track small bright subject, moving horizontally and vertically. Subject is placed at the eyes level.
Quantification of test results is the next:
- 0 – tracking is smooth in all the eyes positions;
- 1 – non-smooth in lateral positions;
- 2 – non-smooth not only in lateral positions;
- 3 points – spontaneous eye movements (nystagmus, saccades).
Note: welders and persons, spending much time at monitors might demonstrate large amplitude spontaneous eye movements, which disappear after several gaze maneuvers to lateral eye positions. Test is better to be performed with nystagmography either electro or video version.
Indicating (past pointing) test – patient is proposed to point with pen or pencil the target with eyes closed at the distance of stretched hand. Results might be fixed at the sheet of paper, monitor screen, etc.
Quantification means:
- 0 point – point in the diameter 25 mm;
- 1 – pointing diameter 50 mm;
- 2 – pointing diameter 75 mm;
- 3 – pointing outside diameter 75 mm.
Direction of mispointing is fixed separately.
According to the result of all the tests vestibular function is evaluated from 0 to 20 points. Figures from 0 to 4 are characterizing norm, 5-9 points indicate small degree of vestibular dysfunction, 10-14 – moderate pathology, and 15-20 – severe lesion, mostly organic.
The sensitivity of such test battery reaches 93.64% (n=912). Time necessary for one patient examination does not exceed 5 minutes. Use of digital camera with video function or even mobile phone provides the possibility to document patient test performance. Adding laser pointer, fixed to the head of the patient, doctor has the possibility to evaluate in figures the sways of patient in all the tests.
Comparing sway amplitudes in Romberg test with eyes opened and closed, at soft support etc., it is de facto possible to obtain all the information same as using of posturographic platform and also additional data with phonation and more sensitive Unterberger-Fukuda and Uemura tests [274].
Among other loadings it is possible to use Romberg, Fukuda stepping and Uemura tests also with acoustic, magnetic, visual, somatosensory and even galvanic loadings [277], though yet these approaches have no evidence base elaborated.
Vestibulo-ocular reflex (VOR) evaluation tests
Examinations are based at two inventions being made by Robert Barany, i.e., both rotation of healthy persons or patients and calorization of labyrinths result in systematic eye movements, nystagmus [13]. Nystagmus eye beatings consist of quick and slow phases, the direction of nystagmus corresponds to the quick phase direction.
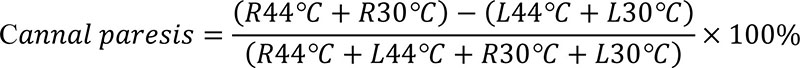
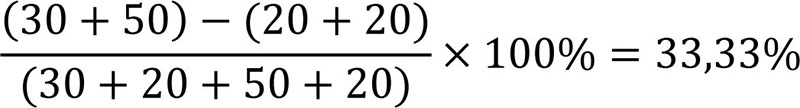
Caloric test is appointed to be “Gold Standard” in the diagnostics of vestibular function and is usually performed according to the protocol of Dix-Hallpike (calorization during 30 s of left and right external acoustic meati with water or air of 30оС and 44оС). Unique feature of the caloric test is the possibility to analyze the result of stimulation of only one labyrinth [97]. They use to study slow phase velocity (SPV) [27] or nystagmus frequency [254]. To establish canal paresis (CP) the difference between right and left labyrinth reactions is estimated [27]:
For example,
Direction preponderance (DP) is also evaluated as difference percentage between left and right labyrinths reactions. DP is manifestation of pathologic asymmetry in the central nervous system, while CP means peripheral lesion. Pathologic changes are considered to start with more than 25% both for CP and DP.
The principal shortcoming of this method is that in the case of very high frequency and low amplitude nystagmus (petit ecriture) it phase is lost for investigator. Today, this rather complicated procedure is sometimes used in USA, but it has mostly historical interest.
In Europe, from the other side, they widely use nystagmus culmination frequency [255], which corresponds to the idea that temporal parameters of physiological reactions have more important diagnostic value, than amplitude ones [215]. Especially convenient and illustrative appears “butterfly diagram”. Data interpretation is performed according to frequency ranges. Increased frequency means hyperreactivity, while decrease lower than the normative values – channel paresis [46].
DP is documented, when they record asymmetric increase of one reaction frequency, for example at 30°С right. Method sensitivity for acoustic neurinom below 15 mm is 70%, and for neurinom of 15-20 mm it is 80-90%, specificity – 90% [19]. Method low sensitivity is somehow compensated by its value in the establishment of hyper or hyporeactivity of the vestibular system, because the latter influences strongly at the management of the disease.
Rotation tests are differentiated into simple rotatory, sinusoidal (pendular), eccentric (otolitic), rotatory tests with head bending (Coriolis forces) and multiaxis tests. Performing simple rotatory test examinator evaluate per-rotatory (evoked during rotation) and post-rotatory (just after stop) nystagmus. Chair with patient is rotated one minute clockwise (CW), one minute pause and after it is rotated one minute counter clockwise (CCW).
Nystagmus is described according to several parameters. Gain – ratio of SPV to chair velocity (American system); ratio of nystagmus frequency to chair motion frequency (European system), normative data – 0.15-0.95. Asymmetry of gain is gain ratio of right to left eye movements in %. Time constant (TC) is time in s, during which gain is decreased to 37% of maximal value (normal 5-25 s) [67]. Test has limited use in clinical practice, because of poor tolerability [249].
Pendular tests (badly tolerated by some patients) are performed with the help of special chairs or with the help of autorotation (active volunteer or passive, with help of investigator hands, head movements). In any case head is performing sinusoidal movements with from 0.01 Hz to 4 Hz frequencies [82]. It has been calculated that biomechanics of human body, in particular neck portion of spine, does not allow to reproduce frequencies higher than 1 Hz, when patient is sitting in the chair, therefore for higher frequencies, they use autorotation test. Healthy persons usually easy going up to frequencies of 3-4 Hz, some well trained ones – even to 8 Hz.
Investigators are examining VOR parameters: gain, asymmetry, phase shift, spectral purity, coherent function, power spectrum and cross-correlation. The normative data for these parameters are considered to be the next (age 15-55 y.o.). Gain: at frequencies 0.01 Hz – 0.25-0.49; 0.02 Hz – 0.37-0.65; 0.04 Hz – 0.44-0.59; 0.08 Hz – 0.49-0.65; 0.16 Hz – 0.50-0.71; 0.32 Hz – 0.50-0.85; 0.64 Hz – 0.50-0.92. Gain asymmetry – normative data do not exceed 14.76%.
Phase shift – difference between phase angles of eye and chair positions (for healthy at frequencies 0.01 Hz – 16.72-58.62; 0.02 Hz – 6.16-33.97; 0.04 Hz – 2.64-22.53; 0.08 Hz – (-3.69)-(+13.02); 0.16 Hz – (-9.51)-(+12.32); 0.32 Hz – (-14.78)-(+8.45); 0.64 Hz – (-14.96)-(+2.64) [67].
Spectral purity means ratio of frequencies filling between input and output, 95% means normative range. Coherent function – is the measure of which part of output is caused by input, 95% means normative range. Spectral analysis shows component frequencies and their harmonics. Cross-correlation – allows to evaluate general interrelationship of two sets of data, in particular, to evaluate temporary relations between vestibular input signal and output eye movement.
Gain appeared to be most variable parameter, while phase shift being most stable and repeatable [188]. If criterion of vestibular reactivity decrease (VRD) is accepted to be 25% method sensitivity is evaluated as 33.5%, and specificity – 92.5%, accepting VRD 20% authors have obtained sensitivity 41.2% and specificity – 85% [82].
It has been also noted that sensitivity of this test differs at different frequencies (n=54), exactly: 0.01 Hz – 12.96%; 0.02 Hz – 24.07%; 0.04 Hz – 38.89%, 0.08 Hz – 42.59%; 0.16 Hz – 35.19%; 0.32 Hz – 35.19%, 0.64 Hz – 12.96% [274].
Though the test is widely spread its use causes many problems, especially related to the results interpretation. Different sensitivity at different frequencies is not clear; there are no clear-cut topographic relations of exact parameters to certain levels or nuclei in CNS. Significant price of the devices to perform pendular test (exceeds 200.000 $) [67] is limiting its distribution.
Thus, low sensitivity, lack of exact topic diagnostics, low tolerability, limited utility for management and high price resulted in Assurance Quality Commission of American Medical Association Act from September 2004, which restricts pendular test performance, after which American Assurance refuse to reimburse the money for this test. From the other side test might be used for scientific purposes in some huge research centers.
Eccentric (otolithic) rotation tests are mostly limited to scientific research and almost not used in clinical practice.
They are performed with the help of specific chairs, which permit the eccentric patient rotation. The test is considered to reflect otolitic function. The investigators are proceeding the parameters, described for pendular test [183]. Rotation tests with head bending (Coriolis forces) and multiaxis rotational tests are used mostly for the purposes of professional stuff selection in the cases, when the requirements to vestibular function are especially high. They study in these cases not simply vestibular function, but rather vestibular stability (tolerance) [283], operator performance [291], changes of biochemical reaction under vestibular loadings [130].
3. Vestibulo-vegetative projection testing
To the group of objective methods belong electrocardiography (ECG) with neurological loadings [179; 192] and pupillometry (video recording of pupilla diameter during test performance) [277]. Loadings might be the same for both methods [264].
Patient is lying at the functional bed. First control ECG (and/or pupillogram) is recorded.
Then during 20 s one of the next neurological loadings is recorded:
- Takahashi test: 10 head movements with 1 Hz frequency in the 90º sector;
- tracking the bright subject moving at the distance of 30 cm from the patient in the sector of 30º;
- calculation: patient is proposed to subtract ana 7 from 100;
- diadochokinesis, fast pronation-supination of the arms;
- reaction to light and darkness, open and close of goggles placed at the eyes of the patient;
- abrupt clacking sound 60-80 dBA;
- physical loading – in the primitive version 10 knee-bend or better treadmill (veloergometry);
- descending of the functional bed to 15 cm during 10 s [277].
Other loading are possible including visual flashes, magnetic, galvanic and psychological stimuli.
After control record of ECG and pupillogram, they perform test and once more recording, make several minutes interval to allow patient restore pulse rate, again make control recording and one by one proceed test performance. As in the peak parameters, intervals and segments there have not been find visible changes, only pulse rate is proceeded.
The procedure proposed allows not simply document cardioneurosis (F 45.3 – somatoform disturbance), but also to establish topographic level of its initiation in CNS. Pupillometry analysis means anisocoria evaluation and wave-like increases of pupilla diameter during test performance studies. Their appearance indicates presence and type of headache. The tests described are now under development, therefore their sensitivity, specificity and other parameters are the subject of future investigation.
But, even today, the test data influence strongly the management procedure. For example, impairment of the calculation test results mean correction of GABA-ergic mechanisms, etc.
Other vestibular loadings are used for studies of vestibulo-vegetative projection. Moderate electromagnetic field loading results not only in coordination impairment, but it may also increase arterial blood pressure [71; 282].
4. Vestibulo-limbic projection test studies
Studies of all EP parameters have been analyzed: vestibular, visual, acoustic and somatosensory, – from one side, and from the other – data of tonal audiometry: absolute meaning of the thresholds and correlation coefficients, both in the general group and in the group with psycho-emotional disorders have been performed. In the patients with emotional disturbances significant difference between audiometry threshold left and right side has been estimated [6; 277].
Asymmetry of visual P100 is also providing some inspiration for documentation limbic function in future [234]. From the point of view of evidence-based medicine the data, obtained at one laboratory have limited significance. To improve the situation it is necessary to repeat the result in the several establishments and with bigger patient group.
Special attention needs the reference for test method in the dizziness evaluation. The situation seems to be less precise in the case of functional disorder, which is revealed neither by neurovisualization methods [21, 184], nor biochemical, immunologic, bacteriologic alone.
Therefore, the benefit of videophysiology and electrophysiology is evident (evoked potentials, cranio-corpo-graphy, nystagmography). In the best opportunity it is supported with full scale examination of the big hospital.
E. Evaluation of the disease severity
Stages of management must be: continuous, progressive, upgrading. Each new step has to upgrade and not refuse previous management [205]. The process has to be organized according to severity degree of disease [12] which is to be evaluated before management start:
- Mild – everyday activities, both routine and professional are easy going, additional symptoms are absent, instrumental methods: obligatory – Uemura test is 1 point (video obligatory), and desirable – 20-point coordination battery 5 points (protocol and video obligatory), increase of VestEP one peak latency up to 50%.
- Semi-mild – dizziness disturbs routine and/or professional activities, additional symptoms might be present, instrumental methods: obligatory – Uemura test 2 points (video obligatory), and 20-point coordination battery 6-9 points (protocol and video obligatory), desirable – increase of VestEP more then one peak latencies up to 50%, CCG up to 50% increase of pathologic signs.
- Middle – routine and/or professional activities are difficult to be performed, balance is disturbed, vomiting episodes are possible, instrumental methods: obligatory – Uemura test 3 points (video obligatory), and 20-point coordination battery 10-14 points (protocol and video obligatory), VestEP increase more then one peak latencies more then 50%, cranio-corpo-graphy pathological signs 50-100% increase, as well as nystagmography, pupillometry and ECG with neurologic loading. Posturography and rotation tests (might be used if patient condition allows) reveal additional data. Patient might have neurotization signs.
- Intensive – routine and/or professional activities are difficult to be performed, falls and multiple vomiting episodes are present, instrumental methods (as thorough examination as possible is necessary): increase of VestEP one peak latency more then 100%, Uemura test 4 points (video obligatory), and 20-point coordination battery 15-17 points (protocol and video obligatory), cranio-corpo-graphy pathological signs, as well as nystagmography, pupillometry and ECG with neurologic loading. Posturography and rotation tests (might be used if patient condition allows) reveal pathology. Neurovisualisation, biochemistry, virusology, bacteriology and other methods are desirable to be performed as wide as possible.
- Very intensive – routine and/or professional activities are impossible. Patient cannot serve himself. Head movements cause intensive vertigo with falling and vomiting. Instrumental methods (as thorough examination as possible is necessary): increase of VestEP more then one peak latencies more then 100%, Uemura test 5 points (video obligatory), and 20-point coordination battery 18-20 points (protocol and video obligatory), cranio-corpo-graphy pathological signs, as well as nystagmography, pupillometry and ECG with neurologic loading. Posturography and rotation tests are impossible to be performed. Neurovisualisation, biochemistry, virusology, bacteriology and other methods are desirable to be performed as wide as possible.
1. Stages of dizzy patient management
depend on severity degree of the disease.
First line aid doctor during primary or secondary medical examination perform diagnostic Uemura test and estimates the severity degree of the disease. In the cases related to 1 degree the medications of 1 line are prescribed, in 2-5 degree cases, the patient has to be directed or at least consulted by certified specialist to manage dizziness. In the case of non-effective treatment the patient must be transported to higher level hospital not later than one month in the case of stable dynamics and immediately in the case of disease progressing.
- Primary disturbance of the 1 degree may manage doctor of any specialty using first line medications (1 day master-class training). Most important criterion – 1 point according Uemura test.
- Primary disturbance of the 2 degree may manage doctor, who have passed special training in dizziness, know the differential diagnostics of dizziness/vertigo, bedside dizziness documentation and principal therapeutic technologies (1 week training). Criteria: 2 points Uemura test, and 5-9 points according to 20-point test battery.
- Primary disturbance of 3 degree and early delayed consequences may manage the doctor, practicing in certified for dizziness medical establishment, passed special training in dizziness, can operate and interpret methods of vestibular evoked potentials, cranio-corpo-graphy and nystagmography, types of dizziness (vestibular disorders) differentiation and know the therapeutic technologies (1 month training course). Patient needs instrumental investigation with vestibular evoked potentials and cranio-corpo-graphy, ECG and pupillometry with neurological loading.
- Primary disturbance of 4 degree and delayed consequences may manage the doctor (medical team), practicing in certified for dizziness medical establishment, passed special training in dizziness, can operate and interpret methods of vestibular evoked potentials, cranio-corpo-graphy and nystagmography, has access to additional methods of dizziness types differentiation and know the therapeutic technologies (3 months training and 2 years of experience).
- Primary disturbance of 5 degree and delayed consequences may manage medical team headed by specialist with academic degree, obtained for dizziness studies, practicing in certified for dizziness multiprofile medical establishment with stationary and emergency, passed special training in dizziness, can operate and interpret methods of vestibular evoked potentials, cranio-corpo-graphy and nystagmography, has access to МRI, CТ, USI, angiography, additional methods of dizziness types differentiation, know therapeutic technologies (1 year training and 5 years of experience or academic grade in dizziness).
- Delayed consequences may manage the doctor (starting from level 3), practicing in certified for dizziness multiprofile medical establishment, passed special training in dizziness, can operate and interpret methods of vestibular evoked potentials, cranio-corpo-graphy and nystagmography, has access to additional methods of types of dizziness differentiation and know the therapeutic technologies
2. Requirements to doctors’ education
Basic program is proposed for training course “Dizziness in medical practice”. It is destinated for doctors of medical units, certified for Dizziness. Objective is updating of theoretical knowledge in the clinical diagnostics and management of vestibular disturbances, accompanied by dizziness and space orientation disorders 1-3 stage of severity, for doctors of stationary and ambulances.
Duration of the training course – 1 month; Academic hours in total – 156; including: lectures – 56; practices – 64; seminars – 32; examination – 4 hours.
Plan of lectures
| № | Topic | Hours |
| 1 | Concept of vestibular system | 4 |
| 2 | Anatomy and physiology of vestibular system | 4 |
| 3 | Symptoms of vestibular disorders. Degree of lesion severity, delayed consequences | 4 |
| 4 | Methods of examination. General characteristics | 4 |
| 5 | Methods of examination. Sensory projection: anamnesis, questionnaires, vestibular evoked potentials | 4 |
| 6 | Methods of examination. Motor projection: 20-point score battery, cranio-corpo-graphy, video-nystagmography | 4 |
| 7 | Head trauma | 4 |
| 8 | Magnetic sensitivity | 4 |
| 9 | Methods of examination. Vegetative projection: pupillometry, electrocardiography, neurological loadings | 4 |
| 10 | Methods of examination. Limbic projection: questionnaires, audiometry | 4 |
| 11 | Vestibular peripheral lesions | 4 |
| 12 | Vestibular central lesions | 4 |
| 13 | Management of vestibular disorders. First line medications. General principles of therapy | 4 |
| 14 | Management of vestibular disorders. Pharmacotherapy | 4 |
| Total: | 56 |
Plan of practices
| № | Topic | Hours |
| 1 | Anamnesis specifics in the dizzy patient | 4 |
| 2 | Questionnaires NOASC and Types of Dizziness | 4 |
| 3 | Performance, videorecording and interpretation of Uemura test | 4 |
| 4 | Performance, videoregistration and interpretation of 20-point battery results | 8 |
| 5 | Performance, videorecording and interpretation of Takahashi test | 4 |
| 6 | Performance, videorecording and interpretation of cranio-corpo-graphy results | 4 |
| 7 | Performance, videorecording and interpretation of nystagmography results | 4 |
| 8 | Performance, videorecording and interpretation of combination of cranio-corpo-graphy with nystagmography results | 4 |
| 9 | Performance of electrocardiography with neurootological loadings | 4 |
| 10 | Additional tests: phonation, magnetic loading | 4 |
| 11 | First line medications management | 4 |
| 12 | Etiotropic management of dizzy patient | 4 |
| 13 | Management depending from the lesion topography | 4 |
| 14 | Management of certain types of dizziness | 4 |
| 15 | Vestibular rehabilitation | 4 |
| Total: | 64 |
Seminar topics proposed, but may be changed according to local conditions (16 topics, two academic hours each, might be corrected according to the students profile):
- Kinetosis;
- Head trauma;
- Monitor disease;
- Vestibular migraine;
- Magnetic and meteo sensitivity;
- Stress action at vestibular system;
- Delayed consequences of vestibular lesion;
- Types of vestibular lesions;
- Databases formation and analysis;
- Description and variation statistics;
- Correlation statistics;
- Regional situation monitoring;
- Operation research;
- Estimation of vestibular lesion severity;
- Space perception, orientation and interaction;
- Factors of progress.
All the training of certified dizziness doctors is to be based at the training course proposed. It might be shortened to one-day master-class (1 degree), where the general concept of vestibular system, characteristics of vestibular disorders are lectured, Uemura test is proposed to be documented with simple video and interpreted in standard form.
Second step is one week training for the doctors, which mean study differentiation of dizziness from vertigo, disorder documentation with Uemura, Fukuda tests, individual management (2 degree).
Certified for dizziness doctor have to pass one month training course, presented in this paper (3 degree). Next education steps are related to self-education of the doctors (according to Bologna requirements). After one month training the doctor returns to his working place and create databases of patients of his hospital in his area, with their specifics.
After 3-6 months he comes to training center and makes a report about specific features of his patients (4 degree) [62]. Doctor who wants to proceed his education during this visit discuss with experts his further research (must be organized according to WHO Operations Research requirements) [74].
Doctor agrees with experts the management of some critical group of patients, try the new approach to management and after one academic year, make presentation to experts (5 degree).
Authors propose to organize International Dizziness Academy and International Certification Committee to start the process of international standardized certification of Clinics managing dizzy patients, unified education of doctors involved in dizziness management and world-wide monitoring of situation.
Materials for doctor training both free and payable are available: trinus.konstantin@gmail.com.
3. Requirements to the hospitals
Hospitals differ according to the severity degree of patient.
- Stage of severity needs minimum of requirements. This mean, that family physicians and doctors of any specialty pass one-day master-class, know how to perform and video-record Uemura test, know first line medications and know near-by certified Dizziness Center. Doctors know the differentiation criteria for Stages of Severity establishment.
- Stage of severity needs that Doctors know the differentiation criteria for Stages of Severity establishment. Family physicians and doctors of any specialty pass one-week training know how to perform and video-record Uemura test and 20-score test battery, know differentiation of dizziness/vertigo and medications for both cases and know near-by certified Dizziness Center. Hospital of this level creates databases of dizziness patients in its area.
- Hospital is equipped with Vestibular evoked potentials, cranio-corpo-graphy, nystagmography, ECG with neurological loading tests and pupillometry. It has at least one certified Dizziness specialist (one month training). Hospital of this level creates databases of dizziness patients in its area. Hospital supervises lower level medical units.
- Hospital is multiprofile; it has Dizziness Lab, equipped with Vestibular evoked potentials, cranio-corpo-graphy, nystagmography, ECG with neurological loading tests and pupillometry. Emergency is obligatory, as well as MRI, CT, biochemical Lab. It has doctor team with at least one certified Dizziness specialist (one month training). Hospital of this level creates databases of dizziness patients in its region. Scientific research unit is obligatory, monitoring situation with Dizziness in the big region. Dizziness unit accumulate, supervise Dizziness information from nearby smaller Hospitals and ambulances. Publications are obligatory.
- Hospital is multiprofile, it has Dizziness center, equipped with Vestibular evoked potentials, cranio-corpo-graphy, nystagmography, ECG with neurological loading tests and pupillometry. Emergency is obligatory, as well as MRI, CT, biochemical Lab. It has doctor team with at least one certified Dizziness specialist (with academic grade related to Dizziness). Hospital of this level creates databases of dizziness patients in its country or bigger region. Scientific research unit is obligatory, monitoring situation with Dizziness at the international level. Dizziness Center accumulates supervises Dizziness information from Hospitals and ambulances world-wide. Publications, guidelines and clinical protocols are obligatory for the status of the International Center. Meta-analysis, new devices and methods development are important activities. International Conferences and Congresses are important certification criteria. Today facilities like PC tablets give the opportunity for videorecording of the tests and cloud technologies propose the possibility to on-line consultation of every patient at the Dizziness Center even if the patient is at the far-away area.
F. Prophylaxis of vestibular disorders:
- Lifestyle (smoking, alcohol, diet and physical activity),
- Controlling chronic diseases (diabetes, lipidemia, hypertension, uricemia),
- Awareness of occupational hazards (both routine and labor) and correct dosing of them.
First two points are well known and being discussed many times [113]. Therefore we see it to be more reasonable to detailyse the last third point. We should like to structure it according to the concept of vestibular system. Let us start with vestibular peripheral sensors.
Acceleration sensor – in today world there are the next problems, influencing this function: head trauma, hypergravitation in supersound jet flights, spacecraft weightlessness and kinetosis in passengers of different vehicles. Prophylactic of head trauma means escaping conditions leading to it. In occupational, sport, traffic medicine they are precisely reglamented by regulations about safety measures (including helmets, safety belts, etc.), professional selection conditions. In routine head trauma is more rear, but is less predictable.
Anyways, even healthy individuals have to be aware of danger of falling in winter time, when there is ice in the road. Kinetosis becomes real tragedy of today. The speed of running man is approaching 30 km/hour, world champions’ in sprint is about 36 km/hour, while today cars are moving up to 300 km/hour, flights – 700 km/hour. Besides, maneuvers and vibrations are influencing the patient conditions. The duty of medical doctors and nurses is to make patients (especially sensitive to kinetosis) aware that they have to minimize high speed conditions to rational limits.
Pharmacological prophylactic is to be started with menthol, consumed before travel. More potent is vertigoheel. If it appears to be not sufficient transdermal scopolamine may be used. In severe cases they use dimenhydrinate, if necessary combined with cinnarizine or flunarizine [217].
Gravitation changes may be classified as natural and technogenic. The first are caused by moon position, planets’ parade, comets, etc., the second are created in high speed aviation, space and different entertainments, like funny hills, caroseries or so. Hypergravitation in military aircraft has strict restrictions, as well as spacecraft activities; any pilot has to evaluate risk/benefit before starting these types of professional life.
Medical stuff has to explain the public that vestibular tolerance is inborn and its training is equivocal, so it is better to be careful with vestibular overloading. Pharmacological prophylactic is to be started with menthol, consumed before travel. More potent is vertigoheel. In some cases pharmacological doses of coniin or picrotoxin may be applied. If it appears to be not sufficient transdermal scopolamine may be used. In severe cases they use dimenhydrinate, if necessary combined with cinnarizine or flunarizine.
Saccular sound and infrasound perception is related to communication of great animals: elephants, predators – lions, tigers. They accompany natural catastrophes like hurricanes or earthquakes. Technogenic are industrial and routine noises, acoustic explosions and technogenic infrasounds, produced by ventilations, chimneys, engines and sometimes blocks of elevators in skyscrapers.
Concern is growing that children and young adults are developing noise-induced hearing loss as a result of “environmental” overexposure to amplified music, especially through the use of personal music devices such as MP3 players. The reported use of these devices is high in young people — more than 90% in surveys from Europe, and the United States and users often listen for several hours a day at maximum volume.
The devices increasingly use earphones that insert into the ear canal, which produce higher sound levels in the ear than “over the ear earphones” used at the same volume. These sound levels can exceed 120 decibels, similar in intensity to a jet engine.
In 2001, an analysis of national US health survey data found that 12.5% of children aged 6-19 had audiograms suggestive of noise induced hearing loss [209]. Explosive sounds with infrasound components are typical for military activities. But they appear to become the problem among the persons entertaining with firecrackers in civil public [200]. Diabetes, tobacco smoking and chemicals have synergic action with noise, while alcohol – protective [196] Prophylactics depends on the particular type of noise loading.
We can’t stop hurricane, but usually local governments use to evacuate people from the area of its action. For those, who appear to be inside medication prophylactics is necessary. It is to be started with menthol, consumed before the start of hurricane. More potent is vertigoheel. If it appears to be not sufficient transdermal scopolamine may be used. In severe cases they use dimenhydrinate, if necessary combined with cinnarizine or flunarizine.
For those on duty it is important to keep in mind that histaminic and calcium channel blockers can retard the reaction. Industrial noises (including explosive, for example granite excavations) have their regulations, medical stuff has to supervise the exact observation of them. We cannot influence military and terroristic activity, but explain the sides the consequences of the war and call them to peaceful negotiations.
In routine, it is rather difficult to control routine noises, produced by traffic or some teenager idiots, who like to use 140 dB amplifiers in the municipal flats. Soundproof of walls, doors and windows can be the way out sometimes. The role of family physicians is to explain young people the danger of sound overloading and MP3 players.
For persons inhabiting noisy accommodations vitamins, antioxidants are beneficial, sometimes with pharmacological medications, mentioned above [196].
Vibrations (low-frequency whole-body) in nature are typical for earthquake or approach of great animal, which means danger. Therefore, like infrasound, whole-body low-frequency vibration may cause panic in some patients and even healthy persons.
We can not predict earthquakes far in advance to evacuate all the public from the dangerous area today. Besides natural sources of vibration, modern society has created plenty of technogenic ones: industrial – tractors and other moving mechanisms; and routine – buildings, located over metro stations, next to intensive traffic ways, multistore buildings; vibrations are generated by the engines operating in the different constructions – supermarkets, business centers, sound dynamics at conference halls, so on. For industrial noises and vibration they have elaborated protective measures and regulations [244].
For routine – it is necessary to escape the sources of vibration; especially it is important for susceptible persons. As a temporal measure pharmacological prophylactics may be used for reasonable time period. It starts with menthol. More potent is vertigoheel. If it appears to be not sufficient transdermal scopolamine may be used. In severe cases they use dimenhydrinate, if necessary combined with cinnarizine or flunarizine. For those on duty it is important to keep in mind that histaminic and calcium channel blockers can have sedative effects and retard the reaction.
Magnetic sensors in living beings are located at labyrinth, ethmoid bones and eye retina [282]. Labyrinthine magnetic sensor percepts magnetic impulse, ethmoidal – magnetic lines of the Earth magnetic field, function of the retinal magnetic sensor is recalibration from visual to magnetic orientation at sunset.
Labyrinthine magnetic sensor in humans has been shown to change its function even after short-lasting electromagnetic field (EMF) irradiation (5 minutes listening of advertisement from handy phone [277]). Natural magnetic impulses are typical for solar activity (magnetic storms), electric discharges between clouds during thunderstorm, or when negatively charged clouds are moving over the person.
Modern society created also technogenic electromagnetic smog, generated by moving vehicles, radio and TV stations, handy phones, Wi-Fi, Wi-Max and their retranslators. According to WHO experts analysis, both natural and technogenic EMF impair 5% of healthy persons [114]. But, 40% of patients are complaining meteo and EMF-sensitivity [282].
Prophylactic measures mean shielding critical rooms, using compensators, decreasing EMF of nearby generators. Use of most “meteo-protectors”, proposed at the market of medications has no evidence. Medical correction of the vestibular function may give temporary relief.
Metabolic sensor is overloaded by changed chemical environment: washing substances, changes in the structure of alimentary products. Prophylactic means more natural products in the diet, escaping as much as possible to intake industrial and home-use chemical substances.
If not possible, donators of sulfhydril groups are reasonable to be consumed. Dietary products are the first to be started: chicken and duck meat, sweet red pepper, garlic, onion, greenery.
Pharmacological correction of the vestibular function, as well as hepatic and renal functions is beneficial.
Prophylactic of the vestibular disorders of the CNS
Vestibular integrative function provides the space perception, orientation and interaction. It is based at the integrative proceeding of visual, acoustic and proprioceptive inputs to the vestibular nuclei. Therefore, excessive negative information from these inputs may overload them and cause pathologic processes to develop. Prophylactics depend on the particular type of professional activity: hypodynamia – needs active movements, visual tension during monitors use – visual training: gazing close and faraway subjects, relaxation at wild nature conditions. Vestibular function correction with pharmacological medications is beneficial.
Time perception is related to vestibular function [129]. Modern people are travelling a lot, both because of professional activities needs and for leisure purposes. Long-distance travelling is connected with crossing time zones. For aviation stuff there are regulations mostly reglamenting activity and rest conditions. No regulations for passengers can be applied. No regulation includes prophylactic measures and health control criteria, especially regarding vestibular function. Among pharmacological substances, isovaleric acid, menthol and melatonin are recommended [151].
Delayed consequences – prophylactic measures. All the persons with primary vestibular damage have to be informed about the delayed consequences, their signs, danger prognosis and nearby Centers for management. Depending on the severeness of the vestibular damage the imaginable wellbeing period might be from few days to several years. During this time person only seems to be healthy.
In reality, there are the signs, indicating the progressing of the disease. The symptoms are rather different, but general mainstream is rather strictly determinated. Most important is the fact that peripheral dysfunction is involving higher levels of CNS into the pathological process.
Vestibulo-sensory projection pathology starts with short-lasting attacks of dizziness, vertigo, space orientation disorders – acrophobia, agoraphobia, etc., as well as associated disorders: migrainous headaches, nausea, retching, vomiting episodes, tinnitus, black-outs and numbness. During one-two years these attacks become longer, more severe, the amount of accompanying symptoms increases. After couple of years different neurological signs appear, especially in motor sphere. Coordination impairs and drop attacks are possible.
Two-three years later vegetative symptoms appear (palpitations, blood pressure lability), as well as blood formula changes: glucose, lipid spectrum, uric acid, blood proteins. At this period control of blood pressure is necessary, together with vestibular function correction. Five-ten years from the initial vestibular lesion vestibular dysfunction reaches cortical level, causing disruption of GABA-glycin balance.
The latter results in the dysbalance of all mediator systems, fall down of the immunity, disorders in many systems. This leads to chronic infections, autoimmune and oncodiseases. Prophylactics mean awareness of the danger of delayed consequences, understanding their vestibular origin and knowledge of the nearby Center where they are managed in a proper professional way.
G. Acute disorder management
In this period patient complains of severe vertigo, with coordination impairment, retching and vomiting, consciousness may be altered or lost. He needs specialized management depending of the cause of the disease [251].
1. Organization of medicare at prehospital period
includes first aid medical emergency to the patients with vestibular disorder from the moment of admission of the patient or his representative’s application to the moment of patient’s hospitalization.
First aid or emergency medicare at prehospital period is provided by:
- Occasional persons present;
- Any doctors present at the moment;
- Family physicians;
- Emergency.
Acute severe dizziness/vertigo episode means call of the emergency and patient hospitalization, no matter who is present next to the patient at a moment. Today, most of such patients are admitted to stroke departments.
The task of the Emergency is to differentiate stroke from the diseases with similar symptoms. Warning signs and symptoms of stroke [113]:
- Weakness: sudden weakness, numbness or tingling in the face, arm or leg;
- Trouble speaking: sudden temporary loss of speech or trouble understanding speech;
- Vision problems: sudden loss of vision, particularly in one eye or double vision;
- Headache: sudden severe headache and unusual headache;
- Dizziness: sudden loss of balance, especially with any of the above signs.
2. Hospital management
During hospitalization procedure the doctors are to make up the final decision to which type of clinics it is necessary to admit the patient. Typical etiologies causing vestibular dysfunction are listed below.
Head trauma needs visual examination and palpation to establish damages of ear, head and neck. The criteria of the severity are: vomiting and even short consciousness loss, confusion or disorientation [249]. If the patient meets these criteria he has to be transported to neurosurgical stationary. MRI is important to establish brain tissue damage or bleeding and CT – for bone fractures [77].
Acute head trauma is managed in neurosurgery. During first days severe complications may be caused by subarachnoid or brain tissue bleeding. Starting from subacute period full scale vestibular diagnostics is necessary: questionnaire, VestEP [305], cranio-corpo-graphy [15], nystagmography [51], ECG with vestibular loadings and emotional status studies (posttraumatic neurosis) [249].
Vascular catastrophe (TIA, stroke, gastric form of myocardial infactus). For the first two dizziness or pseudovertigo, decrease of conscious level, confusion, SOD also in situation and time, uncontrolled urination and release are possible, weakness of one hand or foot, asymmetric face, emotional, speech disturbances are typical. MRI is the method of choice and the patient is to be brought to the specialized stroke center during the therapeutic time window [304].
Starting from subacute period full scale vestibular diagnostics is recommended: questionnaire, VestEP, cranio-corpo-graphy, nystagmography. Vestibular rehabilitation training is necessary to be started as early as possible [3]. Gastric form of myocardial infactus is rather rare, but dangerous form, disease is mostly characterized by pain in the left epigastrium, dizziness, nausea, vomiting. It must be differentiated from gastritis, esophageal reflux, poisoning and acute ulcer.
Previous infarcts, specific infarctus galloping rhythm (4th heart sound), ECG infarctus signs are important at the prehospital period [160]. At the hospital ECG and EchoCG with special attention to the lower back wall of the left ventriculus are important, MRI and biochemistry for cardiac enzymes presents evidence of the correct diagnosis [249]. For instrumental differentiation of vascular catastrophe from vestibular dysfunction head shaking nystagmus might be usefull, though the doctor has to know the possible side effects, including cervical spine damage.
Any time it is doctor to realize the responsibility and make final decision to do or not to do head shaking test. Head-shaking nystagmus (HSN) is a jerk nystagmus that may follow a prolonged sinusoidal head oscillation. HSN was first described in 1907 by Robert Bárány (1907). Moritz called it “kopfschutteinnystagmus” (1951).
Subsequent studies (Borries 1923; Klestadt 1936; Vogel 1929) described different techniques of eliciting the nystagmus and advanced hypotheses regarding its pathophysiology (Fetter et al. 1990; Hain and Spindler 1993; Halmagyi and Curthoys 1988; Katsarkas et al. 2000; Minagar et al. 2001; Perez et al. 2004).
Transitory ischemic attack (TIA), which differs from stroke by absence of residual signs in the form of paralysis and paresis, is to be differentiated from Vestibular neuronitis. TIA is characterized with temporary blood supply decrease to some brain area, the reasons being thrombosis of brain arteries, damage or spasm of blood vessels in the brain.
Clinical manifestations of TIA are: dizziness, decrease of conscious level, decrease of sensory organs sensitivity, confusion or loss of memory, SO distortion in situation and time, swallowing difficulties, patient does not recognize relatives, uncontrolled urination and release are possible, weakness of one hand or foot, asymmetric face, coordination, emotional, speech disturbances [304].
In the patient with vestibular neuronitis neither consciousness change is met, no paralysis, no paresis. Vomiting is more typical for neuronitis, and head movements cause crucial increase of symptoms intensity [249]. During TIA BP might be increased and pulsing noise might be heard over magistral arteries. Angiography show the narrowing of the arteries, where how much and if it is bleeding. TIA is often accompanied with cholesterol and blood glucose increase.
TIA is to be managed by specially trained medical stuff in stationary, treatment means anticoagulant, spasmolitic therapy, and if necessary microinvasive surgical treatment. Cerebrolysin decreases the dimension of brain infarctus zone by preventing of edema, stabilizes microcirculation, normalizes neurological and cognitive impairments, and increases the survival rates [303].
These effects have been shown in the cases of stroke and vascular dementia in the double-blind placebo-controlled studies at Eurasian, American and Australian continents [107; 201; 304]. In animal experiments cerebrolysin injection in the therapeutic window of 24-48 from the start of ischemia it increases proliferation, migration, maturation and survival rates of neuroblasts [44; 110].
It has been shown in more than 10 years monitoring, that vestibular disorders preceed arterial hypertension (n=530) [266], (n=123) [278]. Dizziness (or pseudovertigo) episode might initiate ischemic attack and therefore in the cases of acute vascular pathology it is necessary to include dizziness specialist into the TIA/stroke team.
Metabolic disorders include hyper and hypoglycemia, hyper or hypothyroidism, electrolyte dysbalance, uricemia. Differential diagnostics mean specific smell and appearance of the patient. Anamnesis is important for diagnosis preestablishment. Final diagnosis is established at the basis of blood biochemistry.
Brain tumors may cause even drop attacks or consciousness loss. MRI provides evidence of tumor, its location, dimensions and metastases, if any.
Idiopathic neuropathy of facial nerve (Bell paralysis) is considered to become because of autoimmune or viral etiology. Pain at retroauricular area may preceed the facial weakness, which develops after several hours.
The involved side is flat and motionless. In severe case the eye can’t be closed. Treatment includes antiviral, dehydrating, hormones, SH-group donators, nucleosides and vitamins. Prognosis is rather beneficial in 90% cases [249; 257].
Coma of different etiology, belong to diffuse disorders of cerebrum. It is identified as unarousable unresponsiveness; even primitive avoidance reflexes may be absent. Physical examination includes measurement of rectal temperature.
Visual examination of skin, scalp and eyes, especially “doll eye response” is important. Respiratory pattern and cardiovascular signs are taken into account. Patient needs immediate hospitalization to reanimation department [249].
Infections of brain and its tunics, local neurologic deficit after epileptic attack (Todd paralysis), syncope, transitory global amnesia and also secondary neurologic and otolaryngologic disturbances at the basis of somatic pathology: pneumonia, cardiac insufficiency, hepatic or renal insufficiency are to be kept in mind to differentiate vestibular disorder in acute case [113].
Intoxications and radiation disease are characterized by severe dizziness (or pseudovertigo), nausea, retching, vomiting, diarrhea, sweating, vascular collapse. Anamnesis is important, if the patient preserves consciousness. Toxin establishment in time preserves the life of patient – it indicates antidote required [17].
In the case of acute radiation disease epidemiological data about nuclear accident are important [5]. All of them start and develop as typical vestibular dysfunction, the dynamics depending on the doses. In the acute period first aid is necessary, in subacute – vestibular testing is important: studies of all the four vestibular projections are required [266].
Vestibular neuritis is characterized with sudden start, severe vertigo with vomiting, one-side falls, in anamnesis some viral infection [121], consciousness is usually intact, muscle tone is not altered [86]. In some cases MRI might show the signs of local inflammation [184]. In subacute phase full scale vestibular testing (cf. above) is necessary.
Ménière’s disease and syndrome are diagnosed because of sudden onset and typical triad: vertigo (often with vomiting and loss of balance), tinnitus and hearing decrease. Its incidence is 4.6% among vertigo patients in Czech population [93]. Diuretics cause quick relief in the case of true Ménière’s disease, they appear to be beneficial both from the diagnostical and symptomatic treatment positions. They seem to be ineffective in the cases of Ménière’s syndrome [39].
Acute and subacute period for patient is better to spend in the stationary under the supervision of specially trained stuff. MRI might be useful for differential diagnostics in the cases of tumors or otitis, CT in the case of osteomalation of labyrinthine bones [106]. Audiometry and BERA are useful to verify Ménière’s disease [122].
VestEP and nystagmography might be important to establish vestibular lesion. In subacute phase vestibular and auditory testing as wide as possible is necessary. Blood biochemistry analysis is important to exclude hyperglucosemia, diabetes, hyperlipidemia, urolithiasis [181].
H. Chronic vestibular disorder
1. Vertigo versus dizziness differentiation
Electrophysiological characteristics of dizziness and vertigo symptoms have been studied [280]. The subjective sensations of them have been carefully recorded during the caloric test. Only 60.0% of the patients have reported vertigo or dizziness, other 40.0% have indicated warmth, wetness and other sensations not related to vestibular system.
Exclusively dizziness is reported by 8.0%, vertigo – 20.0% patients. 28.0% patients have reported that during one procedure the have felt dizziness, but during the other – vertigo. Attention is driven to the fact that some patients have reported dizziness, which is considered to be of “non vestibular origin” [176], during vestibular stimulation. Additional symptoms: headache, nausea have been reported 4.0% each.
Frequency analysis has shown that in the cases related to dizziness it is 0.7±0.2 Hz, vertigo – 1.0±0.4 Hz. (the difference is statistically significant by the Fisher qualitative criterion, р=0.04). Nystagmus might be physiological and pathological. In healthy volunteers caloric nystagmus frequencies have been identified in the range of 0.8-1.4 Hz [165].
Claussen has identified the frequencies of physiological nystagmus in the range of 0.67-1.67 Hz at big amount of patients. Pathological nystagmus of high frequency is related to hyperreflexy, and vice versa, low frequency – hyporeflexy [46].
Evaluation of the lateralization and temperature dependence of vertigo and dizziness has shown the next results. The data being obtained indicates that vertigo is more exaggerated during cold water irrigation. Vertigo sensation is more typical to left labyrinth stimulation. Last fact might indicate the specifics of the interhemispheral relationship. Taking into consideration the existence of several cortical vestibular representatives (at least two) it is easy to suppose the predominance of sensations described formation in the different nervous centers at different hemispheres: in the right one vertigo, and in the left – dizziness [280].
VestEP recording has shown the crucially increased latencies of all the peaks while the EP of the other modalities: i.e., VEP, SEP, AEP are normal – indicates central and peripheral vestibular dysfunction – it is typical for vertigo. Another version is some moderate increase of P1 and N1 of the VestEP indicate maximal dysfunction in the peripheral, brainstem and subcortical parts of the vestibular system. P2, characterizing cortical excitation, might be intact; the other modalities might be in the normal ranges – typical for dizziness (for example Chornobyl clean-uppers, 884 persons examined [266]).
In the patients with diabetes polymodal EP reveal peripheral nerves dysfunction, especially pronounced in vestibular (coefficient of change of P1 of the long latency evoked potential is 110%, in comparison to visual 55%, somatosensory 32.50%, hearing 30% and olfactory 16.43% peripheral sensory nerves [25]. Evoked potentials (including vestibular) being used for differentiation of neurosis, encephalitis and epilepsy, dizziness has prevailed [269].
2. Types of vestibulo-sensory disorders
In 849 patients among other complaints more frequently than 10% appeared to be: dizziness, subjective vertigo, objective vertigo, giddiness (pseudovertigo), disequilibrium, orthostatics, kinetosis, acrophobia, agoraphobia, nyctophobia, claustrophobia, ascendophobia, descendophobia, optokinesis, nausea, vomiting, headache, black-outs, tinnitus and numbness.
The entire ‘phobia’ named being at the level of mild discomfort and not the exaggerated psychiatric signs. No one patient has psychiatric diagnosis. In 35 patients the correlation coefficients (in brackets) of complaints named versus instrumental examination results have been studied. Correlation coefficients more then 0.40 have been estimated as significant. The next data have been obtained [272].
Dizziness – distortion of perception of space, movement and time [48; 129]. Patient, for example, complains of waiting longtime for cars to pass before making left turn during last month. Vestibular evoked potentials: especially increased P1 and N1 peak latencies [266]. Posturography: negative correlation with limit of stability to the left (-0.4172).
Pendular test (vestibulo-ocular reflex, VOR) with visual fixation suppression (VFX) at 0.04 Hz frequency: negative correlation with phase shift (-0.4754), random saccades: negative correlation with accuracy (-0.4016), smooth pursuit: positive correlation with right eye gain at 0.2 Hz (0.4101), pupillometry – positive correlation with anisocoria during Takahashi test (0.5329).
Objective vertigo – sensation the subjects moving around the patient [249]. Vestibular evoked potentials: all peak latencies increased [280]. 20-point scale – negative correlation with the results of tracking test visual evaluation (-0.4039), posturography – negative correlation with stability limit backwards (-0.4661), VFX at 0.04 Hz – exaggerated positive correlation with asymmetry (0.74742) and phase shift (0.8570), rotatory test clockwise (CW) – asymmetrical correlation with time constant (TC) of postrotatory nystagmus (AN) (0.5495). ECG: negative correlation with duration of QRS (-0.4237).
Subjective vertigo – illusion of nonexistent movement, patient feels him moving [249]. Vestibular evoked potentials: all peak latencies increased [280]. VOR: positive correlation with gain at frequencies 0.08 (0.4042) and 0.16 Hz (0.4251), asymmetry of gain at counter clockwise (CCW) rotation (-0.4914).
Giddiness – vertigo which is not similar to subjective or objective ones, sometimes called pseudovertigo: very intensive, difficult to describe, patients often tell that something is rotating inside of the head [213]. Negative correlation with height is reported (-0.4522). Positive correlation with complaints of nausea while headache spell is noted (0.6455). Vestibular evoked potentials: all peak latencies increased [280].
Pendular test with gaze fixation at frequency of 0.04 Hz reveals negative correlation with asymmetry (-0.4760) and phase (-0.6848). Rotation test: positive correlation with time constant of nystagmus at CW rotation (0.5469). ECG: positive correlation with duration of QRS interval (0.5447).
Imbalance (movement coordination disturbance) – sometimes is met alone. Patients are complaining of swaying, staggering, momentary push… [86]. It correlates with complaints of acrophobia (0.4328) and descendophobia (0.4995). Multisensory evoked potentials: all peak latencies might be intact [277]. Positive correlation with the result of 20-point scale is present (0.4311).
During VOR it positively correlates with gain asymmetry at 0.01 Hz (0.5862), and during VFX at 0.04 Hz has highly expressed correlation with gain asymmetry (0.7811) and especially with phase shift (0.9081). ECG: positive correlation with duration of P (0.69561) and negative with QRS complex – (-0.5375).
Orthostatics – discomfort sensations that appear after sudden standing up [100; 290]. It correlates also with complaining of nausea (0.4267). Positive correlation with rotatory nystagmus gain (0.4531) and per-rotatory nystagmus gain (0.5290), negative with gain asymmetry (-0.4536 and -0.6916 correspondingly) and TC during CCW rotation (-0.4697). Positive correlation exists with gain during stepwise rotation both CW (0.4531), and CCW (0.52909).
Kinetosis – a disorder caused by repetitive angular and linear acceleration and deceleration and characterized primarily by nausea and vomiting [98; 256]. It appeared to correlate with weight increase (0.4146) and photophobia in migraine attacks (0.4414).
Posturography: positive correlation with limit of stability to the left test (0.5933). VOR: positive correlation with gain at 0.16 Hz (0.4549), with VFX at 0.04 Hz – positive correlation with gain (0.4474) and asymmetry (0.4028). During rotation test – negative correlation with gain CW (-0.4588) and TC CCW (-0.4893), positive correlation with asymmetry during CCW rotation (0.4221), and negative correlation with postrotational nystagmus gain CW (-0.4588).
Acrophobia (height vertigo, does not belong to true vertigo) – discomfort that appears at height [56; 300]. Has positive correlation with imbalance (0.4328). Posturography – positive correlation with visual perturbed unstable platform test data (0.4109). During rotation test positive correlation with gain CW (0.4304) and gain of post-rotatory nystagmus (0.4304) is recorded. ECG: underlined positive correlation with P interval (0.7258).
Agoraphobia – (αγωρα – Grecian, market) discomfort in open, public places or crowds [249]. Correlates positively with ascendophobia (0.4588) and associated headaches (0.4588). During VOR positive correlation is found with asymmetry at 0.64 Hz (0.4038), and during VFX at 0.04 Hz – negative correlation with asymmetry (-0.7026) and phase shift (-0.5288). During rotation test positive correlation is noted with asymmetry CW (0.4243) and TC for rotatory (0.6366) and post-rotatory nystagmus (0.4736). Pupillometry: positive correlation with anisocoria in diadochokinesis test (0.4385).
Nyctophobia – discomfort, insureness in darkness and twilights [277]. VOR– positive correlation with phase shift at 0.32 Hz (0.5794) is found, during video vestibulo-ocular reflex (VVOR) positive correlation with asymmetry at 0.16 Hz (0.4048) being seen. While CCW rotation is negative correlation with gain it appears (-0.4144).
Smooth pursuit: negative correlation with left eye gain at 0.1 (-0.4034) and 0.4 Hz (-0.4084) is noted and positive correlation with left eye asymmetry at 0.1 (0.4548) and 0.4 Hz (0.4521), and expressed positive correlation with right eye asymmetry at 0.1 (0.6678) and 0.4 Hz (0.5277) is seen. ECG is characterized with exaggerated positive correlation with QRS interval duration (0.8321) and negative correlations with intervals Р (-0.5185), PQ (-0.4623) and ST (-0.4082).
Claustrophobia – discomfort appearing in small, closed spaces [49]. Posturography: negative correlation with body movement velocity at the stable platform with eyes opened is recorded (-0.4581). VOR: positive correlation with asymmetry of nystagmus gain (0.4094) and phase shift (-0.600) is noted at 0.01 Hz frequency, while VFX at 0.04 Hz – underlined positive correlation with asymmetry (0.7474) and phase shift (0.8570) is recorded.
During stepwise velocity rotation test negative correlation with gain CCW (-0.4376), during CW rotation positive correlation with asymmetry (0.5947) and negative correlation with TC (-0.6785) are found. Pupillometry has revealed correlation with anisocoria in Takahashi test (-0.4825). ECG: negative correlation with ST interval duration is marked (-0.4082).
Ascendophobia – discomfort while moving upstairs, patients note the necessity for visual control. Among other complaints correlations with agoraphobia (0.4588) and descendophobia (0.5784) are reported. 20-point scale: positive correlation with writing Fukuda test (0.4071) and general score (0.4678) is found.
VOR: positive correlation with asymmetry at 0.08 Hz (0.4308) is found, as well as positive correlation with TC (0.6320) in CW rotation. ECG: expressed positive correlations with Р (0.7259) and PQ intervals (0.6472) and negative correlation with ST interval duration (-0.4082) are documented [272].
Descendophobia – discomfort during walking down the hill or descending the staircase, patients note the necessity of visual control. Among other signs there is positive correlation with age (0.4037), imbalance (0.5000), ascendophobia (0.5784) and dyspnoe (0.4461).
VOR: positive correlation with asymmetry at 0.01 (0.4638), 0.04 (0.4352) and 0.08 Hz (0.4920) is visible. Step velocity CW rotation test reveals positive correlation with TC (0.7105). Random saccades have shown negative correlation with right eye right side direction movement accuracy (-0.4865). ECG: expressed positive correlation with Р (0.7259) and PQ intervals duration (0.6472), as well as negative correlation with ST complex duration (-0.4082) [272].
Optokinesis – discomfort evoked by optokinetic stimuli, train or cars movement, sunrays blinking through the row of trees etc [249]. It has positive correlation with increase of systolic (0.5202) and diastolic (0.5033) blood pressure. VOR: negative correlation with gain at 0.64 Hz frequency (-0.4002) and positive correlation with asymmetry at 0.04 (0.4223) and 0.08 Hz (0.6080). During rotation test positive correlation is found with TC CW rotation (0.4841).
Nausea is identified as urge to vomit. It has positive correlation with complaints of orthostatics (0.4267), vomiting episodes (0.4148), and dyspnoe attacks (0.4148). VOR: positive correlation with asymmetry at 0.01 Hz (0.4702), and negative at 0.08 Hz (-0.4141), as well as positive correlation with phase shift at 0.64 Hz (0.4115), during VFX test exaggerated negative correlation with asymmetry (-0.8788) and phase shift (-0.6550) at the frequency of 0.04 Hz are revealed.
Rotation test envisages positive correlation with gain both CCW (0.4594), and CW (0.4815), and negative correlation with nystagmus gain asymmetry during CCW rotation (-0.6031). Negative correlation with the increase of systolic blood pressure is reported in these patients (-0.411), also negative correlation with QRS complex duration (-0.6472), in ECG recordings.
Vomiting – is forceful expulsion of gastric contents. It has positive correlation with nausea (0.4148). 20-point coordination scale: positive correlation with Uemura test results (0.4266). Pupillometry: negative correlation with anisocoria during calculation test (-0.5363). ECG: negative correlation with QRS complex duration (-0.6472).
Headache as a substitute of dizziness [66] is positively correlating with agoraphobia (0.4588). Posturography has revealed positive correlation with backward limit of stability test (0.4534). VOR: positive correlation of asymmetry at frequencies of 0.01 (0.4675) and 0.64 Hz (0.4786).
Blackout might appear during sudden movements of head, physical loadings or per se [48]. During random saccades test positive correlation is revealed with velocity of the left eye movements leftward (0.5514). At ECG it has positive correlation with Р (0.5101) and PQ complexes durations (0.62017) and negative with ST duration (-0.5477).
Tinnitus as dizziness substitute has positive correlation with numbness (0.4462). Vestibular evoked potential peaks are increased [226]. During CCW rotation negative correlation is found with nystagmus gain (-0.4397), and positive with asymmetry of this gain (0.5069), as well as with TC of CW rotation (0.4320). Random saccades demonstrate positive correlation with the accuracy of the left eye movements leftward (0.4838).
Numbness is unpleasant sensation of temporary loss of feeling and volunteer control of the parts of the body. Among other complaints it correlates with tinnitus (0.4462). VVOR has revealed positive correlation with phase shift (0.4245), while rotations test – correlation with TC of nystagmus adaptation during CW rotation (0.4502) [277].
Therefore, there are clear-cut defined subjective vestibular function-related complaints, which are recommended to be used in the description of dizziness. The data presented underline the vestibular input into formation of the SOD named above, their different nature (difference between each other), being documented with the help of the world-wide recognized standard test procedures [272].
3. Management of vestibular dysfunctions
Chronic diseases include wide variety of nosologies. Nevertheless, they have some important features in common to benefit the patient management [221]. Their management is to be organized in stages of health care, which means continuous, progressive, step-by-step manner of organization. Each next stage has to progress and not refuse the previous, accumulating the knowledge about patient disease and its specific reactivity to medication.
Prehospital stage is important part of general public understanding of the problem: prophylaxis, responsive approach to the protective measures – individual and corporative, understanding by the relatives of the patient with chronic disease of the problem, understanding of the problem by paramedical stuff. Mostly popular education efforts are necessary [249].
Ambulatory management initiates general medical approach to dizzy patient. In the case of wrong start, patient is during years circulating between the doctors without positive effect, finishing with invalidization, death or psychiatric unit. It is necessary to improve the preliminary diagnostics of all the doctors’ profiles with Uemura test with recommendation to the doctors to use video recording of performance [287].
Types of Dizziness or/and NOASC Questionnaires are important to study the profile of patients at the local area [56]. At least 20-score battery is obligatory for all neurological and ENT units [266]. Their stuff has to differentiate vertigo from dizziness and propose patient specific treatment.
If the patient with dizziness, chronic fatigue, imbalance, space orientation disorders does not feel improvement during one month of ambulatory treatment, no matter of age, he has to be directed to the stationary for examination and profile treatment.
Stationary management starts from investigation. Each big hospital is recommended to have basic level Dizziness Diagnostic (Neurootological) Unit, equipped with: quantitative EEG after Bergmann & Bertora, vestibular (as well as other modalities) evoked potentials [267; 269], cranio-corpo-graphy [50], nystagmography, audiometry, BERA, Electrocochleography [22], ECG and pupillometry with neurological and neurootological loadings [266; 276]. It is recommended to each region to have one at least regional R&D Neurootological center, the function of which must be monitoring of dizziness situation in the area.
Specialized regional centers besides basic level Neurootological Unit are recommended to have extended level Neurootological Department. Besides basic level equipment it must have: posturography, rotating tests facilities, EEG with polymodal evoked potentials (vestibular, acoustic, visual color and white, somatosensory, olfactory) [103]. Neurovisualization: ultrasound with transcranial Doppler, MRI with petrous bone visualization block and CT must be available.
Full scale blood biochemistry, bacteriology, virology, immunology at the international standards level must be available. They must have rehabilitation equipment or supervise patronized rehabilitation centers.
This level centers besides diagnostic and management have also functions of:
- regional data accumulation,
- situation monitoring,
- research & development,
- education,
- public relation,
- coordination with neighbor regional and international centers.
Some regional centers might be organized into National Center or for small countries some National Centers might be organized into International network of Centers.
International research centers have the function of the regional centers. Besides this, they have function of worldwide situation monitoring, testing and implementation new devices, methods, medications and management technologies, issuing Guidelines, Highlights and Expert Consensus documents for the worldwide discussion and implementation.
They organize Foundations for Dizziness studies and coordinate efforts of the regional and National centers in research, development new approaches and industrial devices. They prepare education programs and provide knowledge distribution. They discuss, implement and monitor standards quality control.
They provide spreading important information to Mass-Media to make public opinion aware of the dangers and benefits of the certain branches of progress.
I. Pharmacology of vestibular disorders
In the near past literary sources related to dizziness classification have been presumably based at subjective doctor’s evaluation of patient subjective sensations. This situation results in subjectivism in antivertiginous therapy, when in the medication instruction one might find indications like “dizziness of various origins”.
Physicians Desk Reference lists dizziness related complaints to be side effects for about 1000 medications. “Ironically, many medications used to treat dizziness list dizziness as a common side effect” [cited by 67]. Medications improving dizziness might cause vertigo (for example, dopa-agonists) and vice versa. Therefore, the problem is to highlight the basic principles for drug therapy of dizziness.
The other discussion important is about “first-line” medication. Many candidates are proposed and sometimes it becomes fashionable to prescribe this or that medication to all the kinds of dizziness. The problem arises, what are the criteria of first-line medication.
At list two of them have to be pointed at once:
- usefulness in as much cases as possible;
- least side effects.
From this point of view natural products seem to be most profitable, with minor toxic substances or in the extract form in the low concentrations. Of course, we do not consider acute or severe cases, because vestibular neuronitis and cerebral ischemia have to be treated by specialized stuff and no first-line medication might be proposed. In the chronic medium or mild pathology expression we might discuss the use of some products at all the three periods of vestibular lesion. Among them we can remind concentrated decoctus of Mentha Piperita in the cases of vertigo, nausea and vomiting [249; 257], Ginger root in many cases of dizziness and depression [217], herb of Estragon, which has proved to be effective in mild and middle cases of radiation, vibration disease, head trauma, kinetosis.
Vitamins are effective in many cases [37]. Extract of Conium maculatum is especially effective in cases of arteriosclerosis, followed by cognitive disorders, communication disorders and vertigo of head movements. Anamirta cocculus (picrotoxin) has positive effect in treatment of kinetosis, acrophobia and some other SOD, general discomfort. Ambra is good in cases related to neuroses, dizziness and concentration disorders. Steinoil (Petroleum D) is effective in patients with vertigo, nausea, vomiting, kinetosis and tinnitus. The combination of the last four products in one is named Vertigoheel [217].
In patients with delayed effects of moderate degree radiation disease (n=884 persons) Vertigoheel is decreasing vestibulo-sensory (VestEP), vestibulo-motor (Uemura and Fukuda tests), vegetative (ECG with Takahashi test as loading) and limbic (NOASC Questionnaire) disturbances [266]. Vertigoheel has no contraindications even in pregnant and lactating females, so it might be regarded as strong candidate for first-line medication.
Sedariston, combination of menta and hypericum extracts is shown to be effective in the cases of moderate depression with vertigo [312] Anyways, more evidence-based research is necessary to implement the responsibility of “first-line” medication into world-wide medical practice.
Theoretic background for dizziness therapy is based at the concept of the vestibular system and means the next.
Peripheral organ, labyrinth is composed out of six sensors:
- acceleration,
- gravitation,
- intensive sound and infrasound,
- low-frequency vibration,
- magnetic impulse,
- metabolism.
Central portion of analyzer besides sensory function fulfills also integrative one – it forms space orientation (SO) and effector reactions, interaction with environment. For SO tetrad of sense organs are responsible: vision, hearing, proprioception, vestibular, they discuss also the role of olfaction, magnetic compass and magnetic calibrator in the eye retina. SO starts at the level of vestibular nuclei of the rhomboid fosse, fasciculus longitudinalis medialis plays outstanding role, also lamina quadrigemina, caudal portion of nucleus caudatus.
In the brain cortex besides vestibular projection itself, they differentiate vestibular representations at somatosensory, visual and auditory cortical areas. Vestibular effectory reactions are realized through vestibulo-motor, vestibulo-vegetative and vestibulo-limbic projections.
Vestibular disturbance, no matter which one is passing three phases:
- acute phase,
- period of imaginable well-being,
- delayed consequences.
1. Etiological therapy
This one means providing to the labyrinth sensors the optimal functional conditions. Both deprivation and overloading of certain sensors results in vestibular disorders and necessity for their correction [79; 100].
Peripheral dysfunction
as a subject of classification has lost its absolute value, because of progress in neurovisualization methods for tumor and inflammation estimation.
Moreover, the authors accepting this terminology provide evidence of CNS involvement into the process [69]. Regarding peripheral dysfunction in today diagnostics is important only with identification of the particular character of receptors impaired and pathogenesis.
Establishment of the diagnosis “vestibular peripheral dysfunction” must mean the influence of it at the management process. The use of this diagnosis with only one medication for all the types of peripheral lesions, one side diagnostics (vertigo with instability is indicating peripheral dysfunction) in today world is not acceptable as being not exact.
Not acceptable is to be recognized the diagnosis of “central vestibular dysfunction” without indication of topographic level of disturbance, its character (excitation, inhibition or disihibition) and main features influencing the therapy. Now we come to exact types of dysfunctions and their management.
Excitation versus inhibition is another important problem from the point of view of management strategies. These two entities are cured by different sets of medications.
Excitation is usually accompanying subjective and objective vertigo, kinetosis, nausea, vomiting, exogenous tinnitus, sometimes pseudovertigo, acrophobia, optokinesis, migraine with aura, numbness. Therapy consists of sedation, because no dizziness/vertigo is felt during sleeping, decrease of nerve excitability and nerve regeneration. To sedating antivertiginous belong several medication groups: H1 antihistaminica penetrating blood-brain barrier (dimenhydramine, dimenhydrinate, meclozin), calcium blockers (cinnarizin, flunarizin, cyclandelate), neuroleptica, belladonna alkaloids.
Dimenhydramine causes also sleepiness; meclozin has least of adverse effects, but is least potent. Among neuroleptica sulpirid (benzamin-type drug with dopamine D2 and D3 antagonistic activity) is the most popular.
Also promethazin, triflupromazin and droperidol are used especially in patients who have psychiatric diseases with vertigo and flight illusions as comorbidity. It is necessary to keep in mind that all of them, especially sulpirid may cause hyperprolactinemy.
Calcium channel blockers (cinnarizin, flunarizin, cyclanedelat) of benzhydril type are membrane stabilizing agents with central and peripheral action. Among them cyclandelate is the most potent, but with maximum of adverse effects.
Atropine and scopolamine are belladonna alkaloids, acting as muscarinic blockers, are useful in cases of kinetosis. Side effects mostly limited to dry mouth and eyes [37; 293]. Regulation of nerve excitability include Class IA sodium canal blockers: chinidinsulfat, ajmalin, prajmalin bitartrat, disopyramid; Class IB sodium canal blockers (also have analgesic properties): lidocain, mexiletin, phenytoin; Class IC canal blockers: flecainid, propafenon; Class III potassium canal blockers: solatol, amyodaron.
These medications developed first for cardiologic use have great influence at nervous system, especially at its vestibular portion [171]. Restoration of nerve cell and fiber activity is described in details in the appropriate chapters of the Protocol.
Disinhibition is met in the cases of chronic action of damaging factor. It is related to exhaustion of negative feedback and is described in the chapters, for example, vibration disease. It is mostly related to GABA-ergic system [4].
Inhibition is usually accompanied with dizziness, coordination disturbances without vertigo, endogenous tinnitus, slow brainstem degeneration, migraine without aura, ortostatics, claustrophobia, descendophobia and black-outs. The most popular medications are: betahistin dihydrochloride, betahistine dimesilat, cocculus, ingwer, picrotoxin [277; 293]. Nootropic drugs, vitamins, Crebbs cycle activators are also important [279].
Primary sensors dysfunction
Accelerations. Acceleration sensitive system may be disturbed in the result of being at board of moving vehicles (traffic), to the velocities of which modern human beings are not yet accustomed or other physical factor action: head trauma, vibration [177]. From the other side physiological vestibular loading enhances the reconvalescence of the patient during myocardial infarctus, autistic child, newborn breathing and cardiac distortions [134; 190].
Kinetosis – symptom complex appearing in moving vehicles. The earliest sign is typically epigastric discomfort (stomach awareness), followed by malaise and a feeling of warmth, accompanied with the onset of nausea. The development of pallor, sweating and retching mean the onset of vomiting, which generally produces some temporary relief. If it does not reach the vomiting threshold, manifestations are limited to fatigue and drowsiness, i.e., “sopit syndrome”.
Susceptibility to motion sickness varies with age (with peak between 4 and 12 years). Other risk factors include family history of motion sickness, and Asian heritage. Data on susceptibility to motion sickness being collected on a sample of 535 individuals divided into eight groups.
The prevalence of motion sickness among Tibetans and Northeast Indians (28%) was slightly higher than Northwest Indians (26%). Females (27.3%) are more susceptible than males (16.8%). Among different groups, the highest susceptibility to motion sickness (SMS) is recorded in schizophrenic patients (30%), while the lowest in rowers (zero percent, the data may be incorrect because of professional selection).
Individuals with greater spatial and motor control, reflected in sports like rowing, athletics and professions like armed forces, are less susceptible to motion sickness. The SMS is significantly higher in individuals who suffered from spatial disorientation (35.05%), migraine (26.31%), gastrointestinal disorders (26.82%), those with osmophobia (24.64%) and preferred sweet flavors (24.48%) than their counterparts [231]. It correlates positively with weight increase and migraine associated photophobia.
Opposite to other dizziness related symptoms correlation with vomiting is higher (0.3081), than with nausea (0.2259) [272]. Prophylaxis means diet, necessary for preservation or even decrease of weight if recommended, minimization of smoked products, chocolate, histamine containing products (strawberries, kiwi), beer, red wine and coffee [210]. Training is not always successful [9]. Some positive results are obtained with the use of biofeedback.
During vestibular tests with Coriolis effects the volunteers are presented two tracks of ECG one recorded at rest and momentary one. The volunteer is proposed to use his will to make momentary ECG the same as rest one [152]. Among medications they use for prophylaxis are histamine H1, calcium, muscarinic blockers [156], GABA, nootrops with sedative activity (noophen) and monoamines [9]; for pregnant ladies – Vertigoheel, also estragon, ginger [217].
Treatment of kinetosis is of equivocal effectivity. Sedative agents, vestibular blocking agents with sedative activity, beta-blockers, antiarrhythmic drugs, isovalerianic acid and menthol are used. Aircraft stuff sometimes has to be at the high awareness level, therefore they have used stimulators: phenamine, meridile-centedrine, sydnocarb, sydnophen, trimethylxantines, strichnine, securinine, aralozides, separale [9].
Head trauma is always overscale vestibular irritation. World-wide head trauma is leading cause of death. More than 1,5% of USA population suffers from it, with peak incidences being between ages of 15 and 24 and 30% cases require hospital care [238]. 80% of head trauma patients suffer from injuries of minor, 10% of medium and 10% of pronounced severity [145].
In patients with traumatic brain injury they find long lasting impairment of physical, personality and cognitive performance [203]. Acute period is managed in neurosurgery. In this phase in sensory projection they note giddiness (pseudovertigo), severity of which depends of trauma intensity, SOD in situation and time.
In severe cases the patient loose consciousness. In vestibulo-motor projection they report distortion of movement coordination, falling, nystagmus [53]. Vestibulo-vegetative projection dysfunctions – most important are cardio-vascular, but also described are headaches, vomiting, uncontrolled urination and release [266]. Limbic reactions are characterized with emotions decrease, fears and anorexia [249].
Sedative medications are indicated: histaminic Н1, calcium blockers, GABA, antiemetics [59], menthol [257], in severe cases, cardiac activity stimulators (epinephrine derivatives), trimethylxantines [9], medications restoring neuronal functions: cerebrolysin (has positive effects at neurogenesis, synaptogenesis and neuroplasticity like nerve growth factors: CNTF, GNTF, IGF-1, IGF-2 и NGF) [133; 301], antioxidants (ascorbic acid, coenzyme Q10). Patient is better to stay under professional stuff monitoring, MRI or CT is recommended to evaluate brain and bone tissue destruction [219].
At the period of imaginable well-being patients are complaining of short episodes of slight dizziness, sometimes coordination disturbances during or after physical and emotional loadings, meteosensitivity. The clinical picture is accompanied with kinetosis, SOD, such as: acro, agora and claustrophobia, in more severe cases – descendophobia [266].
At this period nootropic medications are indicated, vestibular rehabilitation, life style correction, it is important to escape overloading of the organ: decrease long lasting traveling, chemical stimuli and electromagnetic fields [277]. At the third phase the disorders are developing step by step at all the effectory vestibular projections. At the initial subphase Vertigoheel has proved to be effective. Later they find organic neurological, cardio-vascular, psychotic lesions. It is necessary to implement into complex treatment, besides “profile therapy”, also the vestibular function correction [55].
If not, in several months or years the disturbance reaches cortical area of the brain. The balance of cortical processes is disrupted (especially GABA-glycine) resulting in the disturbance in mediator systems, metabolism, fall of immunity and therefore, chronic infections, autoimmune and oncodiseases are found in patient [4].
It is necessary to reconstruct the GABA-ergic processes (GABA, NMDA-receptor antagonist memantine, in severe cases gaba-pentine), correct vestibular function depending on the character of disturbance – hypofunction (drugs with nootropic effect) or hyperreflexia (two stages treatment: first decreasing hyperreflexia with vestibular blockers, then – medications for plastic processes activation) [54; 280]. Combination of Amantadine 100 mg in the morning and Cinnarizine 25 mg in the evening also is reported to be effective (Alpini 2013).
Understandable, that at once they also treat the nosology, which appears to be the main one at a moment: hypertension, arrhythmia, arteriosclerosis, diabetes, chronic viral infection or tumor [275]. In some patients from our practice this period is accompanied with insomnia with nightmares the latter is easy going with the help of Vertigoheel and melatonin.
Vibration disease is developing similar to head trauma, but differs with low intensity of traumatic process and its chronic character [116]. It holds second place in occupational pathology involving 21% cases together with noise-induced pathology. First phase of the moderate severity process is seen every day after intensive loading (for example, spring and fall agricultural activities, miners, pilots). Additionally in most vibration-inducing machines and mechanisms local vibration is also present [244].
Cochrane meta-analysis has not revealed exact positive effect of glucocorticoids. From the other side, antioxidants (Vitamins A, C, E in combination with NMDA-receptor blocker magnesium aspartate) and chemical reductive agents are useful for prophylactics. They also discuss new substances: organic molecules containing Selene (SPI-1005, Ebselen) [199]. First phase is recommended to be treated like kinetosis [156]. Imaginable wellbeing usually lasts 5-10 years [154; 177]; its management is the same as posttraumatic and post-irradiation syndromes [266].
After 10-years of professional experience they are already speaking about occupational disease, which is characterized besides vegetative-vestibular syndrome (terminology is not correct, from the causal point of view it is vestibulo-vegetative syndrome), also with radiculitis, angio-dystonic, psycho-emotional and Reynaud syndrome [150; 177]. The latter is documented in the form of “extremities thermoamputation” with the help of infrared thermography.
Specifics of occupational pathology is in exhausting of inhibitory feedback processes, which from one side limits the use of activating nootropic medicaments, from the other – it is characterized with lesion complex, which needs many medications, some of them conflicting with each other (for example, nootropic and histaminic blocking agents or thioct acid with magnesium) [265].
So, in this case might be proposed nootropic drugs with sedative activity (noophen) and combination of nootropic medication with SH-group donating substance – Tiocetam (combination of antioxidant thyotriazolinum with nootropic agent piracetam). Tiocetam is unique neurometabolic stimulator, which improve integrative and cognitive brain activities, activates memory and new skills acquisition. Thyotriazolinum and piracetam have potentiating effect, which improves neuroplasticity and synaptic transmission [257].
In pain syndromes management gaba-pentine is effective. In Reynaud syndrome Tanakan is therapy of choice (medication, which is multicomponent in composition and, therefore, has wide activity spectrum: delatate arterioles, venules and capillars, makes blood more liquid because of antiaggregation of erythrocytes, has antioxidative and scavenging activities, enhances glucose utilization and ATP accumulation in the cells, accumulation of nerve mediators and activates neuroplastic processes, well tolerated during long lasting use) [16].
Tanakan appears to be the only EGB 761 medication, which contain less than 50/00 of toxic ginkgolic acid [146]. Liposomal forms of preparations appeared to have low effect [206]. It is also profitable in combined treatment of dizziness and tinnitus in such patients [54] Hypertension in such patients is frequently accompanied with increased cholesterol, which wants the change of the lifestyle and diet [177] and in severe cases use of statins (atorvastatin, cerivastatin, fluvastatin, lovastatin, mevastatin – in animal experiments, pitavastatin – in the cases of high cholesterol levels, pravastatin, rosuvastatin, simvastatin) [249] in the first case.
Sulfonylurea derivatives (tolinase, butamidum, chlorpropamidum, gliclazide, bucarbanum, glibenclamidum, glipizide, gliquidone, glibutidum, metforminum); biguanides are indicated in the case of high blood glucose levels [257]. Air pollution is frequently results in asthmatic components, which limit the use of beta-blocking agents.
In this group of patients they use calcium blockers, angiotensine converting enzyme inhibitors and sartanes, diuretics, in the cases of individual intolerance to the medicaments named – medications of second line, rauwolfia alkaloids, for example. Limbic disturbances [88] are sometimes similar to Parkinsonism and are easy going under dopamine agonists [30].
Cupulolythiasis, is accompanied with benign paroxysmal positional vertigo (BPPV) attacks lasting seconds or minutes and provoked by certain head positions. It has been first described by Adler in 1887. It might be caused by otitis, sinusitis, meningitis, head trauma or headache, migraine, lythiasis, diabetes mellitus, thyreopathy, allergy and many others. In a population-based survey study, the lifetime prevalence of BPPV is found to be 2.4 percent.
The one-year prevalence of BPPV increases with age and is seven times higher in those older than 60 years old, compared with those aged 18 to 39 years. BPPV is more common in women than men in all age groups [33]. Vertigo is supposed to appear as a result of cupula contact with otoconial particles, which have separated from macula. In some specific head position they are touching cupular receptors, thus causing intensive vertigo (movement illusion).
It is necessary to pay attention to the diseases impairing growth, maturation and resorption of otoconia (special role of carboanhydraze is discussed). Nystagmus accompanying BPPV is characterized by fatigue (beating disappear in few minutes) and habituation (repetition of test cause decrease of nystagmus intensity up to total disappearance). Diagnostically significant is only Hallpike test (changing head positions). It is important to differentiate BPPV from central positional vertigo, which may occur with multiple sclerosis, cerebellar disease and brainstem ischemia. In the case of central positional vertigo there might be no latent period, no fatigability of nystagmus, nystagmus might be not classically rotatory, provocation is not always associated with vertigo and nausea which is usually enough intensive in patients with BPPV [105].
Management is based at the movements directed to repose otoconia from semicircular canal to utriculus, where they are resorbed. Most popular are repositioning maneuvers. For posterior canal it is Epley maneuver, Rahko maneuver – for anterior canal and Semont maneuver for horizontal canal [78]. Patient is proposed to lie at the side of vertigo initiation. Doctor is waiting the nystagmus to stop, and then with an abrupt movement put the patient to the opposite side in the mirror position [111].
Cochrane meta-analysis has included 11 studies with a total of 855 participants. Nine studies are based at post-treatment postural restrictions (using instructions to sleep upright) following the Epley maneuver. There is a statistically significant difference found when these restrictions are compared to a control treatment of the Epley maneuver alone. Although there is a difference between the groups, adding postural restrictions conferred only a small additional benefit since the Epley maneuver is effective alone in just fewer than 80% of patients. Four of the studies reported minor complications such as neck stiffness, horizontal BPPV (a subtype of BPPV which is similar to posterior canal BPPV, but has some distinct differences in terms of the signs and symptoms), dizziness and disequilibrium in some patients.
Application of oscillation to the mastoid during the Epley maneuver (two studies) compared to control intervention produced no difference in outcome. No serious adverse effects are reported in any of the studies in the review [112]. The example of such study might be next one. Thirty-six subjects with confirmed, unilateral benign paroxysmal positioning vertigo have been randomly assigned to receive either Epley’s canalith repositioning procedure or a placebo maneuver. All subjects have completed a daily diary for 1 month to document any dizzy spells and their adherence to the posttreatment instructions.
Follow-up Dix-Hallpike testing has been performed after 1 month by an audiologist who has been blinded to the patient’s treatment group status [105]. The discrepancy of data may be due to small number of randomized double-blind studies. Many cases of BPPV (from 27% [157] to 38% [80]) are resolving by themselves within few weeks, therefore one-month monitoring is not enough to make evidence-based conclusion about effectiveness of this or that management procedure.
Analysis of Dix-Hallpike results confirmed that those who receive the canalith repositioning procedure has significantly more negative responses (88.9%) than does those in the placebo group (26.7%) [157]. Semont liberatory maneuver is also among the most successful therapy for benign paroxysmal positional vertigo and improves patients’ quality of life. Cure rates with Semont maneuver appear to be significantly higher (94.2%) than those obtained with flunarizine (57.7%) and no treatment (36.4%) (P<0.001). Within a 6-month follow-up, relapse rates are lower among patients treated with Semont maneuver (3.8%) than those obtained with flunarizine (5.8%) and no treatment (21.1%).
All patients with resolution of symptoms and negative Dix-Hallpike test results show a great improvement in daily activities and quality of life (p<0.001) [222]. Other Cochrane studies have obtained preliminary evidence of reposition maneuver benefit compared with physical, medical or surgical management of posterior canal BPPV. Regular medications (betahistine, prochlorperazine) are rarely prescribed for the patients with BPPV.
Vestibular suppressants and antihistamines are useful in severe vertigo accompanied with vomiting [105]. Etiotropic therapy is directed to carboanhydraze homeostasis normalization, it includes antibacterial or antiviral medications if necessary, also calcium containing and regulating drugs (ethidronate salts may be tested in the future), antioxidants, vitamins D, E, B1, niacin, B6, biotin, C [249].
Gravitation changes are natural (full moon, planet parade, comet passing by – lunatismus) and technogenic, related to high speed aviation and space flights (space sickness).
Lunatismus means not only sleepwalking, but also other pathologic symptoms caused by full moon and celestial bodies’ positions. Some authors have tried to find correlations of lunar phases with changes of blood pressure, pulse rate and breathing rate. In such periods the symptoms are: insomnia, headache, excitation, including irritation up to aggression, bulimia, sexual excitation, salivation, sometimes palpitations, changes of blood pressure, gastritis, enteritis.
Prophylaxis has to provide optimal regime for vestibular organ, decrease of loadings and escape of overloadings. Treatment – sedative, blockers of vestibular hyperactivity: histaminic Н1 blockers, calcium blockers, potassium and magnesium containing agents, GABA agonists, inhibitors of glycine receptors, muscarinolitics, sometimes beta-blockers or dopaminic receptor blockers [169].
Macro and microgravitation are typical for high speed aviation and space vehicles. Besides changes of usual functional vestibular loading is it also characterized with blood repositions (in the cases of macrogravitation in oversound starfighters in the direction of acceleration gradient, microgravitation – to the upper part of the body and head) [239]. Vestibular disorders in microgravity are described in the papers of Prof.Kornilova [139-141].
They are: vertigo, coordinate orientation illusions, coordination disturbances, nausea, and vomiting, which develop during the initial period of adaptation to microgravity (or readaptation to Earth), they are similar to clinical terrestrial motion sickness. This allows to investigators of microgravity physiological effects to identify this status as space motion sickness (SMS).
The most of astronauts and cosmonauts who spend time in orbit have been subject to a form of motion sickness known as space adaptation syndrome (SAS). Investigators, who consider SMS from the point of view of clinical neuropathology as a real disease, underline the similarity of SMS symptoms to clinical manifestations of various forms of vestibular dysfunction.
Investigators, who accept a general physiological view point, consider the set of abnormal response characteristics during adaptation to microgravity (or readaptation to Earth) as a manifestation of natural responses of the body to external effects, i.e. as a specific SAS.
SMS is a state, when normal physiological adaptation enters the decompensation phase, i. e. sensory disintegration is manifested as vestibular disturbances associated with SAS [137].
Most investigators in the USA, Europe and Russia associate the anomalous reactions observed in microgravity (SAS, SMS) with changes in vestibular system function and in all functions based on vestibular afferent input.
Changes in vestibular system function are variously ascribed to changes in the labyrinth internal environment due to the headward fluid shift (fluid-shift theory), to otolith deafferentation, to canal-otolith conflict, to interlabyrinth asymmetry, or to intersensory mismatch (sensory-conflict theory) [45; 89; 135; 137].
Investigators have developed a questionnaire and tests for the study of vertigo and coordinate spatial illusions, sensory-motor and autonomic reactions occurring during adaptation to weightlessness [136]. 114 cosmonauts have been examined in flight. Practically all of the cosmonauts (98%) have experienced spatial illusions of different kinds, intensity and duration during the first hours of spaceflight.
Illusions have been generally noted in darkness or when eyes were closed (77%) during free floating. In darkness or during free floating with eyes closed, 98% of cosmonauts sometimes experienced a state of partial or complete disorientation. The most frequent type of illusion being filling of upside down (16%), followed by illusions of motion of surrounding objects (15%), and illusions of rotational body movement (9%), illusions of displacement and inclination of objects (8%), and illusions of linear body motion (4%).
The illusions are classified as:
1) Coordinate illusions – 31%. The predominant coordinate illusions are illusions of inclination of the body or surrounding objects (illusion inversion). According to Graybiel, illusions of inversion are caused by responses of the otoliths to weightlessness [89].
2) Kinetic illusions – 28%. According questionnaire data, the following types of kinetic illusions have been observed by Russian cosmonauts:
- Vertigo in the saggital (pitch) plane around the Y-axis (pitch illusion);
- Vertigo around the longitudinal (Z) axis (yaw illusion);
- Vertigo in the frontal plane around the X-axis (roll illusion).
Sometimes it has been combination of yaw, roll and pitch illusions.
3) Mixed illusions – 41% (combination of coordinate and kinetic illusions).
It is necessary to note that illusions of motion are described in clinical literature as objective and subjective vertigo, but the coordinate illusions: inclination and upside down, – are not used in Disease Classifications. Seems, they are worth of special study in clinical practice, especially from the point of view of subjective vertical and horizontal (remark of the Authors).
The majority of cosmonauts (72%) have agreed that illusions and autonomic reactions (hypersalivation, nausea, and vomiting) are triggered during the first few days of flight by increased motor activity, especially abrupt movements of the head and trunk. Some cosmonauts (11%) have associated the development of illusions with the sensation of blood rushing to the head during the acute period of adaptation to weightlessness.
Other cosmonauts (21%) have indicated that optokinetic stimulation is the triggering factor in the development of illusions and autonomic reactions, and also the absence of the accustomed feeling of support and sensation of ‘up and down’. In many cosmonauts tracking moving subjects through the window significantly intensified illusions and autonomic reactions.
According to the cosmonaut reports, illusions could be suppressed by the following simple ways: visual fixation at some subject; rigid fixation of the body trunk on the couch with head or feet pressed against it; or through the use of autogenic feedback training methods.
Special methods being used to correct and ameliorate illusions and autonomic reactions in weightlessness: muscle stress created by elastic cord exercise, contact with a motionless support, physical loading created during bicycleergometer and treadmill exercise, administration of negative pressure to the lower body, wearing pneumatic occlusion cuffs on the legs, wearing neck pneumatic shock absorber to restrain head movement, drugs. According to 82% of the cosmonauts questioned, this has resulted in an improvement of their condition and a decrease of illusions.
In the history of spaceflight all cosmonauts who have experienced vestibular discomfort are without exception ultimately able to adapt to the conditions of weightlessness. Analysis of the inflight data shows that illusions developed virtually instantaneously after transition to weightlessness, while autonomic symptoms either not occur at all or appear significantly later.
The statistical analysis being performed, demonstrate absence of correlation between illusory and autonomic reactions. These findings suggest that the illusions are not primary sensory reactions preceding autonomic disturbance, but have an independent mechanism of development.
Modern approaches to non-pharmacological prevention and therapy of vertigo (dizziness) and balance disorders in space flight and in patients with vestibulopathia.
A new computerized method is proposed for correction and treatment of illusory (vertigo), vestibulo-oculomotor (nystagmus), and vestibulo-postural (balance) which allows teaching the subject to block generalization of an afferent signal to effector mechanisms of the central nervous system by developing a fixation reflex, employing a delayed feedback.
This method has well proved in space flight and in clinic for subjects with peripheral, central and psychogenic vestibulopathia [142].
Acoustic trauma and noise disease (AT and ND) appear as a result of long lasting (occupational, professional or accidental) action of intensive sounds and noises. While occupational noise is tightly regulated by noise protection regulations, leisure noises have been poorly addressed. The aim of the study cited is to estimate prospectively the incidence of blast and explosion trauma due to the use of New Year’s firecrackers in a western industrialized society.
The results are based on 562 centers in Germany, including 31 university hospitals and 87 city hospitals as well as a random sample of specialized otorhinolaryngology private practices (n=444). After extrapolation of the number of reported cases to the number of hospitals and practices on duty, a total of 8.160 cases (95% confidence interval 7.515–8.805) are estimated giving an incidence of 9.9 per 100,000 inhabitants. There are three times as many male affected as female. The incidence for the age group of 6 to 25 years is much higher: 28 per 100,000 with a maximum of 107 per 100,000 for 19-year-old persons.
These incidences suggest that firecrackers may pose a momentous public health risk. Because of the medical and economic importance of incurable sensorineural hearing loss, it is the task of public health services to promote the effective prevention of irreversible damage to the hearing organ [200]. Sacculus percept sounds from infrasound to 16 kHz with threshold of 40-60 dBA. So, both AT and ND besides hearing distortion are accompanied with vestibular ones which have typical three phase disease development [87].
Their manifestation in sensory projection is tinnitus instrumentally documented by audiometry and evoked potentials both acoustic and vestibular [226]. Coordination disturbances are revealed as well as vegetative symptoms: palpitations, blood pressure (BP) changes, changes in blood enzymes composition, sweating, headaches, nausea, retching, vomiting is rare, but often are salivation, or lacrimation, dry mouth syndrome (for one situation muscarinic blockers, for the other – agonists are medications of choice).
Prophylaxis requires escaping noises and explosive sounds, use of protective measures [244]. Pharmacotherapy is directed at the restoration of injured nerves – use of antioxidants, vitamins, especially В (В6) group. Important components in the treatment are nootrops (tanakan, tiocetam), thioct (espa-lipon), succinic and malic acids. Among symptomatic medications antiarrhythmic, hypotensive, histaminic Н1 and muscarinic blockers may be named [249].
Electromagnetic fields effects (EMF). Magnetic impulse sensors are located in the labyrinthine macula [186]. Just they are known to percept weather changes, because clouds movement creates electromagnetic field with Earth surface, as well as a thunderstorm discharge.
In the today world technogenic electromagnetic impulses are irradiated by multiple generators. WHO reports 5% of Global population being hypersensitive to EMF [72]. Their activity results in sensor overloading, and then the process is developing like kinetosis and vibration disease. It has been noted that even moderate loading impair coordination function, especially in sensitive patients [282].
As delayed consequences increased systolic pressure and cancer risks are mentioned among the persons exposed to electromagnetic fields [71; 114; 224; 240; 241]. Prophylaxis: shielded rooms, compensators decreasing EMF. In the case of acute disturbance (overloading) the therapeutic strategies is similar to the one for kinetosis, delayed effects treatment is the same as the one for head trauma and radiation disease [277].
Changes of reduction-oxidation potential in the inner media result in ratio SH- and S-S groups’ changes, thus influencing the rigidity of hair cell cilia in labyrinth [242]. Sensitivity of this system is the highest; it exceeds all the other system sensitivity by 3-5 orders [253]. One of the vestibular peripheral functions is reduction-oxidation potential changes perception and thus the condition of metabolic processes and its impairment when inner media are invaded by toxins or ionizing radiation [170].
Metabolic changes, as it has been shown result in severe impairment of vestibular function, and this means that besides specific treatment of diabetes, thyroiditis, etc, it is obligatory to pay attention at vestibular function, also oxidation processes, lipids and pathologic metabolites [29].
Intoxication from the point of named above is percept just by vestibular system [248]. It has been shown, that it is vestibular analyzer to initiate the reaction chain, directed to homeostasis restoration, starting from blood plasma enzyme composition [130] and ending with evacuation of poisons from gaster and intestines [9].
Thus, in toxicology, besides specific antidotes and correction of mineral and protein blood composition, it is profitable to optimize the vestibular function at all the levels of its formation. At peripheral level hair cell cilia sulfhydril groups suffer. At this basis the complexons, donating sulfhydril groups (unithiol, dimercapthol, succimer and sodium thiosulfate), reductive and chelating agents, intra and extracellular antioxidants are indicated [257]. Among sulfhydril group donator thioct acid has neuroprotective and neurorestorating, antioxidative properties.
Side effects of its different salts are the next:
- Ethylendiamin – contact dermatitis, skin and mucous irritation, allergic reactions. Cross allergy to antihistaminic drugs with ethylendiamin structure.
- Trometamol – local irritation, tissue necrosis. During intravenous injection hyperkaliemia, diarrhea, hypotension may happen.
- Meglumin – headache, fatigue.
Intravenous injection are accompanied with burning sensation in shoulder and arm (non-significant, short-lasting). Crebbs cycle is activated with the help of malic and succinic acids [220]. Inhibition in sensory projection, depending on the level of pathologic process, wants activation of mediator systems: cholinergic, adrenergic, dopaminergic or serotoninergic. Their hyperactivity, on the opposite side, needs the agents, blocking exact mediators [37].
Decrease of tonus in vestibulo-motor projection wants correction of mineral balance [65], vitamins, cholinesterase blockers and adrenaline or dopamine agonists. Respiration inhibition is treated with nicotinic agonists: lobelin, citizin, anabazin or gabazin [36]. Muscle spasms are reduced by myorelaxants (central or peripheral), in the cases complicated with tunnel syndromes they use analgetics, anti-inflammatory, vitamins of B group (B12), sometimes botulinic toxin (Dysport) [217].
Vestibulo-vegetative system distortions are various: untreatable vomiting, intensive headaches, gastric and intestine spasms, palpitations and arrhythmia, blood pressure increase. Patient needs sorbents (activated carbon, skilpin), blood plasma restitution, colloid and rehydrating solutions. Vomiting is treated with antiemetic agents: dopaminic, muscarinic, serotoninergic blockers, menthol.
For example, vomiting resulting during chemotherapy of oncologic patients is used to be stopped with dopaminic blockers: metoclopromide, domperidone, haloperidol, chlorpromazine and alizapride [92]. Strongly expressed antiemetic activities have phenothiazine tranquillizers, which have besides main dopamine blocking effect also less expressed antihistaminic and anticholinolitic action. To this group belong: acepromazine, chlorpromazine, and prochlorperazine. Their possible side effects include hypotension because of also α-adrenoblocking action and lowering of convulsions threshold in epileptics [257].
Extrapyramidal syndromes might appear as interaction with antihistaminic drugs (diphenhydramine). Muscarinolitic antiemetics are: atropine, scopolamine, izopramide and peripheral cholinolitics: glycopirrolate, propanteline, metscopolamine. They are characterized with short lasting activities and are mostly used for kinetosis treatment. Histaminic blockers are characterized with cholinolitic effects: diphenhydramine, dimenhydrinate, promethazine (phenothiazine with Н1 blocking effect), cyclizine, and meclizine (two latter are teratogenic in high dozes) [156]. Metoclopramide has three manifestations of antiemetic activity: in low doses antidopaminic, in high doses – antiserotoninergic, peripheral action is in gastric and duodenal peristaltic activation.
It is used during chemotherapy, in the cases of slow gastric peristaltic, reflux and viral enteritis. The medication is popular also in veterinary as antiemetic for small species. Contraindication is duodenal obstruction or ulcer [214]. In patients with vomiting initiated with cytotoxic drugs, radiation or chemotherapy serotonine antagonists are indicated: ondasetron (not effective in kinetosis), dolasetron, granisetron, tropisetron and alizaprid [292].
ECG is to be monitored, because some medications from this group of are increasing QT, granisetron [40]. In the cases of cisplatin ototoxicity clinical trials (phase II) have approved MRX-1024, D-Methionin and N-acetyl-Cystein (NAC) to be effective [199; 251]. Caspase inhibitors prevent cisplatin-induced hearing loss [295]. Among popular folk remedies menthol is known as concentrated decoctus of Mentha piperita in the case of intractable vomiting [257]. In sub acute phase nucleosides, antioxidants, vitamins В, С, Е, nootrops. In some patients Vertigoheel and espa-lipon appeared to be highly effective. Delayed consequences are treated symptomatically.
Viral toxins in acute form might cause vestibular disturbances: dizziness, coordination impairment, nausea, vomiting and constipations [121]. Detoxication is performed with antacidic, antioxidant, antiallergic medications. If infection is caused with group A flue virus effective appear to be amantadine (it has also expressed antidopaminergic effect in Parkinson disease and medication induced extrapyramidal reactions) and rimantadine. Amantadine potentiates interferons’ activity in complex treatment of C hepatitis [104]. For flue B group viruses most effective appear to be oseltamivir and zamivir [76].
Flue and other viruses, causing acute respiratory sickness, specifically impair statoacoustic nerve [121]. Herpes group is especially characterized with chronic form and low activity with minor clinical manifestations (pathologic fatigue, weakness, loss of initiative, chronic headache, hearing function decrease, tinnitus) and elevated levels of IgG to herpes 1, 2, 3, rubella, cytomegalovirus and Epstein-Barr virus (in the last case the monocytes number is also increased). Positive effect is provided with antiviral drugs: acyclovir, valacyclovir, gancyclovir, panavir (in the case of mixt-virus infection). Neurological management of the patient depends of exact symptom complex and its severity [123; 268].
Vestibular neuronitis (neuritis) might develop either during infection or after it [86]. Type I hair cells and thick fibers are the first to suffer, because they have less optimal ratio of square to volume, then in type II hair cells and thin fibers. Disease is manifested with severe vertigo, horizontal spontaneous nystagmus (with a rotational component) toward the unaffected ear, deviation of the subjective visual vertical toward the affected ear, coordination impairment, postural imbalance with falls toward the affected ear nausea and vomiting.
The head-impulse test and caloric irrigation show an ipsilateral deficit of the vestibuloocular reflex. Sometimes direction preponderance is revealed. Vestibular neuritis is the third most common cause of peripheral vestibular vertigo. It has an annual incidence of 3.5 per 100,000 population and accounts for 7% of the patients at outpatient clinics specializing in the treatment of vertigo.
Treatment: antiviral, histaminic, calcium, muscarinic blockers, nucleosides (cytizine and uridine) [217], antioxidants, vitamins В, С, Е, metabolites. Corticosteroids improve the outcome of vestibular function up to 62% [243]. From the other side meta-analysis of four trials, involving a total of 149 participants compared the effectiveness of oral corticosteroids against placebo.
All the trials were small and of low methodological quality. Although there was an overall significant effect of corticosteroids compared with placebo medication on complete caloric recovery at one month (risk ratio (RR) of 2.81; 95% confidence interval (CI) 1.32 to 6.00, P=0.007), no significant effect was seen on complete caloric recovery at 12 months (RR 1.58; 95% CI 0.45 to 5.62, P=0.48), or on the extent of caloric recovery at either one month (mean difference (MD) 9.60%; 95% CI -20.66 to 39.86, P=0.53) or at 12 months (MD 6.83%; 95% CI -27.69 to 41.36, P=0.70). In addition, there was no significant difference between corticosteroids and placebo medication in the symptomatic recovery of vestibular function following idiopathic acute vestibular dysfunction with respect to vertigo at 24 hours (RR 0.39; 95% CI 0.04 to 3.57, P=0.40) and use of the Dizziness Handicap Inventory score at one, three, six and 12 months [75]. In the cases of residual coordination disorders vestibular rehabilitation is indicated [178].
AIDS is characterized, besides dizziness, also with neurological symptoms like acute or chronic aseptic meningitis, peripheral neuropathy and encephalopathy, focal motor and sensory deficits with progressing dementia (diffuse brain damage). Typical are accompanying infections: toxoplasmosis, tuberculosis, neoplasm, herpes group viruses. Full therapeutic sanation is not possible, but long remission is possible with zidovudine, dideoxinozine. Some relief patients have from inhibition of glioxilation reactions, inhibition of virus protease and immunization of the patients. As prophylaxis they describe positive effects of vaccination against HIV [249].
Bacterial toxins have expressed influence at vestibular system. Additional factor is serious neuro and ototoxicity of some antibiotic classes. It is worth of paying attention at most dangerous groups. Following is the list of antibiotics, sorted by class according to Goodmann and Gillman [37].
- Aminoglycosides: amikacin, gentamicin, kanamycin, neomycin, netilmicin, tobramycin, paromomycin. Common uses: infections caused by Gram-negative bacteria, such as Escherichia coli and Klebsiella particularly Pseudomonas aeruginosa. Aminoglycosides are effective against aerobic bacteria (not obligate/facultative anaerobes) and tularemia. Possible side effects are: а) hearing loss, b) vertigo, kidney damage. Serious effect of GDNF expression on gentamicin-induced vestibular toxicity has been revealed [245].
- Ansamycins: Geldanamycin, Herbimycin. Common uses: experimental, as antitumor antibiotics.
- Carbapenems: ertapenem, doripenem, imipenem/cilastin, meropenem. Common uses: bactericidal for both Gram-positive and Gram-negative organisms and therefore useful for empiric broad-spectrum antibacterial coverage. (Note MRSA resistance to this class). Possible side effects: nausea, headache, seizures, rash and allergic reactions, gastrointestinal upset and diarrhea.
- Cephalosporins (First generation): cefadroxil, cefalotin or cefalothin, cefalexin. Common uses: good coverage against Gram-positive infections. Second generation: cefaclor, cefamandole, cefoxitin, cefprozil, cefuroxime. Common uses: less Gram-positive cover, improved Gram-negative cover. Third generation: cefixime, cefdinir, cefditoren, cefoperazone, cefotaxime, cefpodoxime, ceftazidime, ceftibuten, ceftizoxime, ceftriaxone. Common uses: improved coverage of Gram-negative organisms, except Pseudomonas. There is reduced Gram-positive cover. Fourth generation: cefepime. Common uses: covers pseudomonal infections. Fifth generation: ceftaroline fosamil, ceftobiprole. Common uses: to treat methicillin-resistant Staphylococcus aureus (MRSA). Possible side effects: nausea (if alcohol taken concurrently), allergic reactions, gastrointestinal upset and diarrhea.
- Glycopeptides: teicoplanin, vancomycin, telavancin. Common uses: wide spectrum. Possible side effects: allergic reactions.
- Lincosamides: clindamycin, lincomycin. Common uses: serious staphylo, pneumo, and streptococcal infections in penicillin-allergic patients, also anaerobic infections; clindamycin topically for acne. Possible side effects: pseudomembranous enterocolitis.
- Lipopeptide: daptomycin, Common uses: Gram-positive infections.
- Macrolides: azythromycin, clarithromycin, dirithromycin, erythromycin, roxithromycin, troleandromycin, telithromycin, spectinomycin. Common uses: Streptococcal infections, syphilis, upper respiratory tract infections, lower respiratory tract infections, mycoplasmal infections, Lyme disease, pneumonia, gonorrhea. Possible side effects: nausea, vomiting, and diarrhea (especially at higher doses), Prolonged QT interval (especially erythromycin), visual disturbance, liver toxicity, jamber.
- Monobactam: aztreonam. Common uses: Streptococcal infections, syphilis, upper respiratory tract infections, lower respiratory tract infections, mycoplasmal infections, Lyme disease, pneumonia, gonorrhea.
- Nitrofurans: furazolinone, nitrofurantoin. Common uses: bacterial or protozoal diarrhea or enteritis, urinary tract infections. Possible side effects: general intoxication.
- Penicillins: amoxicillin, ampicillin, azlocillin, carbenicillin, cloxacillin, dicloxacillin, flucloxacillin, mezlocillin, methicillin, nafcillin, oxacillin, penicillin G, penicillin V, piperacillin, temocillin, ticarcillin. Penicillin combinations: amoxicillin/clavunate, ampicillin/sulbactam, piperacillintazobactam, ticarcillin/clavunate. Common uses: the second component prevents bacterial resistance to the first component. Wide range of infections; penicillin used for streptococcal infections, syphilis, and Lyme disease. Possible side effects: allergy with serious anaphylactic reactions, brain and kidney damage, anxiety, gastrointestinal upset and diarrhea.
- Polypeptides: bacitracin, colistin, polymyxin B. Common uses: eye, ear or bladder infections; usually applied directly to the eye or inhaled into the lungs; rarely given by injection. Possible side effects: kidney and nerve damage (when given by injection).
- Quinolones: ciprofloxacin, enoxacin, gatifloxacin, levofloxacin, lomefloxacin, moxifloxacin, nalidixic acid, norfloxacin, ofloxacin, trovafloxacin, grepafloxacin, sparfloxacin, temafloxacin. Common uses: urinary tract infections, bacterial prostatitis, community-acquired pneumonia, bacterial diarrhea, mycoplasmal infections, gonorrhea. Possible side effects: nausea, irreversible damage to central nervous system, tendinosis.
- Sulfonamides: co-trimoxazole, trimexazole, sulfadimethoxine, sulnilamide, mafenide, sulfonamidochrysoidine, sulfacetamide, sulfadiazine, silver sulfadiazine, sulfamethizole, sulfamethoxazole, sulfanilimide, sulfasalazine, sulfisoxazole, trimethoprim, trimethoprim-sulfamethoxazole. Common uses: urinary tract infections (except sulfacetamide, used for eye infections, and mafenide and silver sulfadiazine, used topically for burns). Possible side effects: nausea, vomiting, and diarrhea, sensitivity to sunlight, decrease in white blood cell count, allergy (including skin rashes) and crystals in urine, neurotoxic, kidney failure.
- Tetracyclines: demeclocycline, doxycycline, minocycline, oxytetracycline, tetracycline. Common uses: syphilis, chlamydial infections, Lyme disease, mycoplasmal infections, acne rickettsial infections, malaria. Possible side effects: sensitivity to sunlight, gastrointestinal upset, potential toxicity to mother and fetus during pregnancy, enamel hypoplasia (staining of teeth; potentially permanent), transient depression of bone growth.
- Drugs against mycobacteria: clofazimine, dapsone, capreomycin, cycloserine, ethambutol, ethionamide, isoniazid, pyrazinamide, rifampicin, rifabutin, rifapentine, streptomycin. Common uses: antileprotic, antituberculosis, urinary tract infections, mostly Gram-positive and mycobacteria, Mycobacterium avium complex. Possible side effects: general intoxication symptoms, reddish-orange sweat, tears, and urine, rash, discolored urine, neurotoxicity, ototoxicity.
- Others: arsphenamine, chloramphenicol, fosfomycin, fusidic acid, linezolid, metronidazole, platensimycin, quinupristin/dalfopristin, rifaximin, thiamphenicol, tigecycline, tinidazole. Common uses: spirochaetal infections, meningitis, MRSA, topical use, or for low cost internal treatment. Historic: typhus, cholera. Gram negative, gram positive, anaerobes, VRSA, Infections caused by anaerobic bacteria; also amoebiasis, trichomoniasis, Giardiasis, Traveler’s diarrhea caused by E. coli, protozoan infections. Possible side effects: discolored urine, headache, metallic taste, nausea; alcohol is contraindicated, aplastic anemia, thrombocytopenia, upset stomach, bitter taste, and itchiness.
Therapy with antibiotics named is recommended with protectors: antioxidants, sorbents (activated coal, smecta) reductive agents and sulfhydril group donators. In most cases they have to be separated in time from antibiotic consuming.
Helminthes, proteus and fungi are causing the symptoms of general intoxication and, exactly, vestibular symptoms: dizziness, headache, nausea, retching, vomiting episodes [249]. Anthelmintics or antihelminthics are drugs that expel parasitic worms (helminthes) from the body, by either stunning or killing them. They may also be called vermifuges (stunning) or vermicides (killing). It is understandable that vermicides are more toxic.
Benzimidazoles: Albendazole – effective against threadworms, roundworms, whipworms, tapeworms, hookworms; Mebendazole – effective against pinworms, roundworms and hookworms; Thiabendazole – effective against roundworms, hookworms; Fenbendazole – effective against gastrointestinal parasites; Triclabendazole –against liver flukes; Flubendazole – effective against most intestinal parasites; Abamectin – effective against most common intestinal worms, except tapeworms, for which praziquantel is commonly used in conjunction with abamectin; Diethylcarbamazine –against Wuchereria bancrofti, Brugia malayi, Brugia timori, tropical pulmonary eosinophilia, loiasis; Niclosamide – effective against tapeworms; Ivermectin – against most common intestinal worms (except tapeworms); Suramin; Pyrantel pamoate – effective against most nematode infections; Levamisole; Praziquantel – against cestodes, some trematodes; Octadepsipeptides (e.g.: Emodepside) – is effective against a variety of gastrointestinal helminthes; Aminoacetonitrile derivatives (e.g.: Monepantel): effective against a variety of gastrointestinal helminthes including those resistant to the other drug classes.
There are also some natural antihelmintics: Tobacco (Nicotiana tabacum & Nicotiana rustica), Moringa oleifera (Moringaceae), Neem (Azadirachta indica), Black walnut (Juglans nigra), wormwood (Artemisia absynthium), clove (Syzygium aromaticum), tansy tea (Tanacetum vulgare), Hagenia (Hagenia abyssinica), Garlic (Allium sativum), Diatomaceous Earth (DE), Pineapple (Ananas comosus), kalonji (Nigella sativa) seeds, male fern (Dryopteris filix-mas), Monarda fistulosa (Wild Bergamot), Honey mixed with water and vinegar was also used as a vermifuge, Plumeria (P. acutifolia or P. rubra) in Brazilian folk medicine, Peganum harmala, Banisteriopsis caapi, genistein (from soy and other legumes).
Antiprotozoal agents (ATC code: ATC P01) is a class of pharmaceuticals used in treatment of protozoan infection. Protozoans have little in common with each other (for example, Entamoeba histolytica is less closely related to Naegleria Fowleri than it is to Homo sapiens) and so agents effective against one pathogen may not be effective against another. However, metronidazole is selective for anaerobic organisms, and so it is effective against many (though not all) of these pathogens.
An antifungal medication is a medication used to treat fungal infections such as athlete’s foot, ringworm, candidiasis (thrush), serious systemic infections such as cryptococcal meningitis, and others. Such drugs are usually obtained by a doctor’s prescription. Representatives: Eflornithine, Furazolidone, Melarsoprol, Metronidazole, Ornidazole, Paromomycin sulfate, Pentamidine, Pyrimethamine, Tinidazole. Classes: Polyene antifungals: Natamycin – 33 Carbons, binds well to ergosterol, Rimocidin, Filipin – 35 Carbons, binds to cholesterol (toxic), Nystatin, Amphotericin B, Candicin; Imidazole: Miconazole, Ketoconazole, Clotrimazole, Econazole, Omoconazole, Bifonazole, Butoconazole, Fenticonazole, Isoconazole, Oxiconazole, Sertaconazole, Sulconazole, Tioconazole; Triazoles: Fluconazole, Itraconazole, Isavuconazole, Ravuconazole, Posaconazole, Voriconazole, Terconazole, Albaconazole; Thiazoles: Abafungin; Allylamines: Terbinafine, Naftifine, Butenafine; Echinocandins: Anidulafungin, Caspofungin, Micafungin; Others: Polygodial – strong and fast-acting in-vitro antifungal activity against Candida albicans, Benzoic acid – has antifugal properties but must be combined with a keratolytic agent such as in, Ciclopirox – (ciclopirox olamine), most useful against Tinea versicolour, Tolnaftate, Undecylenic acid – an unsaturated fatty acid derived from natural castor oil; fungistatic as well as anti-bacterial and anti-viral, Flucytosine or 5-fluorocytosine – an antimetabolite, Griseofulvin – binds to polymerized microtubules and inhibits fungal mitosis, Haloprogin – discontinued due to the emergence of more modern antifungals with fewer side effects, Sodium bicarbonate (NaHCO3) – shown effective against green mold on citrus under refrigeration and powdery mildew on rose plants.
Ménière’s disease (MD) and syndrome (MS)
MD is characterized with symptoms triad: hearing function decrease, tinnitus and intensive vertigo attacks. The prevalence is reported to be between 43 and 218.2 cases/100,000; incidence is 4.3-45/100,000 population [143; 299]. In the Framingham study, (Framingham, Mass, USA) 1.48 % of the population claimed to have a history of Ménière’s disease [173]. Acute episodes of disease tend to occur in clusters with a mean frequency of 6-11 clusters per year, though the remission periods may last several months.
Episodes have been observed to increase frequency during first few years after initiation and then decrease in association with progressive sustained hearing and vestibular function deterioration [168]. In most cases vertigo episodes ceases completely by themselves. Principal factor in the disease formation is considered to be the insufficiency of endolymphatic duct. Decompensation appears as a result of viral or bacterial infection, causing endolymphatic hydrops [172], which in severe cases lead to semitendinous labyrinth ruptures.
The latter one results in the paralysis of hearing and vestibular end organs. At the initial stage disease impair one ear and has fluctuating character – patients are complaining of hearing changes at one side, sometimes they note spontaneous hearing improvement during vertigo episode. Hearing decrease before vertigo attack is typical. Vertigo is very intensive, rotational by modality, lasts several hours with vegetative symptoms. Vomiting brings temporary relief.
The American Academy of Otolaryngology – Head and Neck Surgery (AAO-HNS) has produced diagnostic Guidelines, last revision of which being done in 1995 [60].
Though this document is not universally accepted, it provides simple, easy to perform diagnostic criteria for clinical practice:
- at least two spontaneous episodes of severe rotational vertigo lasting minimum 20 minutes;
- audiometric confirmation of sensorineural hearing impairment;
- tinnitus and/or perception of aural fullness.
For diagnosis establishment full-scale clinical picture, vestibular and auditory evoked potentials, as well as caloric test are also useful, though evidence-base is not elaborated. Ideally, the aims of treatment are:
- reduction of the number and severity of vertigo attacks;
- abortion or amelioration of hearing impairment or loss, associated with tinnitus during the attack;
- alleviation of any chronic symptoms (including tinnitus and imbalance);
- prevention of disease progressing (they name hearing and balance functions decrease [39], but we have to underline the other long-lasting consequences of vestibular disorder, including arterial hypertension, cardiac arrhythmia, metabolic disorders) [279].
Treatment: patient needs hospitalization to specialized department. During crisis diuretics, dehydrating agents, histaminic blockers and sometimes antiemetics are used [94].
Among diuretics they have described:
- thiazide derivatives (benzofluazide, hydrothiazide, chlorthalidone, which inhibit Na+/Cl– reabsorption from distal convoluted tubules of the nephrons);
- potassium sparing diuretics (amiloride, spironolactone, triamterene, which inhibit Na+/K+ exchange within collecting ducts);
- loop diuretics (furosemide, which inhibits co-transporter in the medullary thick ascending limb of the Henle loop);
- carbonic anhydraze inhibitors (acetazolamide, inhibitor of H+ secretion, thus promoting Na+ and K+ excretion).
According to Cochrane report therapeutic effect of diuretics is rather unclear, because the authors are ignoring AAO-HNS recommendations; no studies met the inclusion criteria for review [39]. Though small amount of patients studied (22) in a single trial, it has been shown statistically significant positive effect of intratympanic dexamethasone injections after 24 months follow-up study [197].
In the cases of debilitating vertigo, resistant to treatment, it might appear the necessity for surgical interaction, exact character of which depends on the hearing decrease level [95]. Recent Cochrane review has find that neither study has reported any beneficial effect of surgical treatment either in placebo study or grommet incertion [207].
Sometimes gentamicine injection into inner ear is considered to be compromise version for the patient [161; 233]. At intercrisis period they use vestibular rehabilitation training [3]. Effective protectors of hearing and vestibular functions are known to be antioxidants (non-stimulating), Crebbs cycle activators, sulfhydril group donators, potassium salts.
MS there are certain clinical forms, related to Ménière’s triad. MS is related to the next diseases.
Fistula is developing next to lateral semicircular canal as delayed consequence of cholesteatome. It may be suspected with constant puruleous otorhea, positive Tulio phenomenon. Nystagmography reveals non-fatiguing directional fixed nystagmus more prominent when affected ear is in the down position [289]. CT gives the chance to establish final diagnosis. Treatment is surgical [232].
Labyrinthitis is complication of otitis, cholesteathoma or meningococcal meningitis. Treatment: antibiotics, desensibilizing, antifungal, if necessary – surgery [86]. Serous labyrinthitis is characterized with expressed vertigo, tinnitus and hearing loss, accompanied with horizontal nystagmus opposite to the affected labyrinth.
Caloric test shows canal paresis; cranio-corpo-graphy indicates coordination impairment with clear lateralization, MRI with pyramid bone access special function might show changes in the structure of pyramid. Serous labyrinthitis is suspected at the previous or general infection background. Purulent labyrinthitis results in total deafness, because of process spread at cochlear and labyrinth destruction, it needs immediate operation and antibiotic therapy [163].
In some cases MS may be related to chronic otitis, otosclerosis, head trauma, herpes group viruses and syphilis (less typical are hyperinsulinemia, hypothyroidism, Cogan’s syndrome, Mondini dysplasia and psychogenic MS). These diagnoses are established with patient examination using corresponding biochemical, bacteriological and virusological analysis [144].
Psychogenic MS is met in the situation of divorce, loose of big money amounts, employment and similar vital stress conditions. Psychogenic MS is also regarded as syndrome of injustice. In the diagnostics it is necessary to find out possible reasons of patient conflict with social environment. In most cases the doctor cannot influence social events, but the task of medical stuff is to help the patient surviving the crisis with minimal looses, adapt to changes and sometimes – start new life. Treatment is symptomatic. Psychotropic medications are of low effectivity [42].
Allergy. Considerable part of allergies develops with vestibular participation [108]. Worldwide, sensitization (IgE antibodies) to foreign proteins in the environment is present in up to 40% of the population. Worldwide, allergic rhinitis affects between 10% and 30 % of the population. Worldwide, drugs may be responsible for up to 20% of fatalities due to anaphylaxis. Worldwide, adverse drug reactions may affect up to 10% of the world’s population and affect up to 20% of all hospitalized patients [193].
Because of this all the antiallergic drugs influence the vestibular function. It is necessary to start with alimentary products, causing allergy, which contain high concentrations of histamine-like substrates: strawberries, lemons, oranges, tomato, β-lacto-globulins – these ones are better to be excluded from the diet during treatment of allergic and autoimmune diseases [210]. It is necessary to be careful during therapy of patients with some SOD (for example, black-outs), because they have tendency to prolongation of QT intervals at ECG [227], and some of Н1 blockers are just known to increase QT interval.
Therefore, in some cases medications of choice besides histaminic blockers may be desensibilizing agents, such as calcium chloride or gluconate [257]. In patients with dizziness histaminic agonists and nootropic drugs are usually indicated, which might be dangerous for allergic patients [217; 280].
Allergies are accompanied by the content of sulfhydril group changes in the organism tissues, they have to be protected thanks to alimentary products, containing sulfhydril groups: pork, chicken, turkey, eggs, milk and cheese, yogurt and plant products: red pepper, garlic, onion, broccoli, seeds. If protein-containing products are themselves allergenic, containing sulfur as simple (sodium thiosulfate) and complex products (alpha-lipoic acid, unithiol) are indicated [37; 210]. In severe cases glucocorticoid hormones are used. In some patients fasting is very effective.
Pregnancy means change in functional CNS condition, hormonal background and increased loading at the systems releasing metabolites. All the three factors impair vestibular function – early stage toxicosis is vestibular disturbance. Pregnancy put severe limitations at the assortment of medications to be used. Diet is important, among pharmacological substrates ambra, petroleum D, conium, and camphora (vertigoheel).
Migraine in many cases is related to vestibular disorders and is accompanied with vertigo. In migraine without aura prophylaxis is enough effective (up to 80%) appeared to be histaminic agonists (beta-histine, noophen) [276], less effective (50-70%) seems to be beta-blocking drugs [101]. The US Headache Consortium lists five drugs as having medium to high efficacy in migraine treatment: amitriptyline, divalproex, timolol, propranolol and topiramate [124].
In the patients with histaminergic migraine with aura, aura without headache and cluster headache: if the pain is occipital by location most effective is cyclandelate, in the temporal area – Аrlevert (mixture of cinnarizine with dimenhydrinate). During spells – zolmatriptan, nomigraine, ergotamine are the medications of choice. Alprazolame is also reported to have positive effect during spell in the pilot-study [177, 266]. Among new aspects there are reports about positive effect of amantadine both for spell treatment and prophylaxis [236].
Non-steroid anti-inflammatory agent, diclofenac potassium in the form of sachets, prepared according to DBT technology (Cambia, Volfast, Katafast) starts its activity earlier than the other medications and has been reported to be equivalent in effectivity to sumatriptan during spell both in Europe [68] and US [155].
Information loadings (monitor disease) are related to spreading of computers, TV, plasma screens and even neon blinking lights. Practically all the sense organs are overloaded. Of course, the main loading is directed to vision, but the sounds are also changed – they are mostly technogenic [149], we are constantly under electromagnetic smog [296], spectrum of the fragrances and tastes is changed [167] as well as alimentary substrates [11].
Last 50 years our sense organs function in unnatural regime. Signs of monitor disease are: long lasting activities with monitors in anamnesis, dizziness and SO disturbances, headaches, vision dysfunctions, nausea, tinnitus, numbness, black-outs, palpitations, skin symptoms, allergies [277]. Prophylaxis starts with diet containing folic acid: broccoli and other types of cabbage, spinach, caviar, calf liver, eggs and products containing melatonin: blackberries, blueberries, black porridge, plums, products, containing histamine-like substrates: strawberries, lemons, grapefruit and kiwi.
Treatment: nootrops, vitamins of B group, antioxidants, serum containing compounds. If patient has gastric or intestine spasms – muscarinic blockers, palpitations – beta-blockers etc [37].
2. Therapy, dependent from topography of pathology
At the today stage of science development we are only approaching target principle of therapy in neurology in general and dizziness neurootology in particular. Nevertheless, even first news about target brain levels for some medications, even if they are not the only targets, they are extremely important for practical doctor.
Peripheral structures pathology
may be inborn or acquired. The first may be related to the form of labyrinth (for example underdeveloped semicircular canals, wide or narrow endolymphatic duct), otoconia development (megaotolith), hair cells or vestibular nerve degeneration.
They are established clinically in childhood (6-12 years) in the form of dizziness, subjective vertigo, impairment of coordination, hearing accompanied with tinnitus. MRI allows establishing final diagnosis. Treatment is symptomatic [106]. Acquired disturbances might be caused by trauma, toxins of different nature, including endotoxins and metabolites, blood circulation disorders, noises, vibrations, electromagnetic and ionizing radiations [277]. In most cases reduction-oxidative potential shifts to peroxidation side, therefore effective appear to be chemical reductive agents, to which belong monosaccharides (glucose), polysaccharides (lactulose) and alcohols (mannitolum).
Depending on the poison character (heavy metals, diabetes, uricemia and rheumatoid arthritis, hepato-cerebral or hepato-lenticular degeneration) in some cases effective appear to be donators of sulfhydril groups: sodium thiosulfate, alpha-lipoic acid, EDTA derivatives, unithiol, dimercaprole, succimer, penicillamin (cuprenile). Positive effects are reported from intracellular (alpha-tocoferrol) and extracellular (ascorbic acid) antioxidants.
Restoration of distorted peripheral structures is supported by medications with nootropic activity: pyracetam, mexidole, Ginkgo Biloba Extract (tanakan), noophen, sodium oxibutirate, pantogam, picamylone, acephene, bemithil, tiocetam. Improvement is reached by using vitamins D, В1, niacin, В6, biotin [195]. In the case of moderate hypoxemia succinic acid is effective, because the disease of mostly type I hair cells and thick fibers occur. Decrease of potassium cause labyrinthine disorders, its balance is restored by use of potassium salts: bromide, acetate, orotate, chloride, panangine or asparcame [249; 257].
Brainstem vestibular nuclei dysfunctions
manifest with multiple clinical signs: subjective vertigo, dizziness, coordination disturbances, nausea and retching, vomiting, sympathetic or parasympathetic vegetative disorders. Histamine and to some extend acetylcholine are most important neurotransmitters at this level [164].
Overexcitation or asymmetric activity of vestibular nuclei are blocked by Н1 histaminic blockers: ethanolamines (dimenhydrinate, diphenhydramine, clemastine), ethilendiamines (chloropramine), tetrahydrocarbolines (dimebon, mebhydroline), phenothiazines (promethazine), alchilamine derivatives (dimethindene), quinuclidine (quiphenadine, sequiphenadine), phthalazinone (azelastine) and second generation blockers: acrivastine, asthemizol, clemastine, loratadine, terfenadine, cetirizine, ebastine, bicarphen, diprazine, phencarol, ciproheptadine, dimebone, dimethinden, oxathomide, setastine, pheniramine [247].
It is necessary to keep in mind that especially asthemizol and terphenadine might elongate QT. Dizziness of cholinergic origin in the patients who have stopped smoking is effectively decreased with the help of nicotinomimetic drugs: lobeline, citizine, anabazine, gamibazine.
The same groups appear to be effective in patients with hypotension of vestibular origin and orthostatics. In excitations like kinetosis, vibration disease, post stress syndrome, magnetic field overloading effective appear to be muscarinolitics: atropine, belladonna extracts, bellataminal, gioscine, scopolamine, gioscingomatropine, plathiphylline (paluphyne, tepaphylline, solutane) – the latter especially in the cases of increased BP and spasmolitine. In the vertigo cases calcium blockers are profitable: cinnarizine, flunarizine, cyclandelate, nifedipine, nimodipine and alkaloids of Vinca minor, vincapan, vinpocetin, cavinton, instenon [313].
Brainstem is the primary level where nystagmus is formed.
Usually, nystagmus accompanies vertigo and is suppressed by vestibular blocking agents [294]. In some particular cases they use symptomatic treatment for different types of nystagmus. For downbeat nystagmus they prescribe: 3,4-diaminopyridin, 4-aminopyridin, baclofen, clonazepam or gabapentin.
For upbeat nystagmus 4-aminopyridin or baclofen is proposed. In the cases periodic alternating nystagmus baclofen is considered to be the agent of choice. Pendular nystagmus is treated with gabapentin, trihexiphenidyl and memantin or retrobulbar injection of botulinus toxin. In episodic gaze ataxia acetazolamid or 4-aminopyridin may be consumed [293].
Midbrain vestibular nuclei dysfunction
is mostly related to muscarinic, dopaminic and adrenoreceptors and manifested as SODs. Increased dopaminergic activity is characterized with objective and subjective vertigo, psychomotor excitation, delirium and paranoia (in schizophrenia they are accompanied with SOD), sometimes with vomiting episodes, convulsions, tendency to abuse and gambling, sometimes with depression, even season type.
Effective appear to be: clozapine (vertigo), methoclopromide, domperidone, galoperidol, trifluperidol (has also anticonvulsive properties), droperidol (has also anticonvulsive properties), chlorpromazine and alizaprid. Wellbutin is the only effective antidepressant, especially in season depressions [64]. In double-blind, randomized, placebo-controlled study has been shown that similar activity at mild and moderate depressive disorder has Hypericum extract STW 3-VI (Laif®), which alkaloids are blocking synaptosomal reuptake of serotonin, dopamine, and norepinephrine at the presynaptic axon terminal, but differs from synthetic analogs with less adverse effects [286].
From the other side dopaminergic insufficiency is accompanied with coordination disturbances, Parkinsonism, restless legs syndrome (RLS), as well as pituitary tumors (prolactinoma), acromegalia, sexual function decrease [187]. Dopaminic agonists are improving the situation: bromocriptine mezilate, ropinirol, cabergoline (also in cases of anhedonism, alcoholism, it enhances study of new motor skills, increase concentration and memory), pergolide mezilate, apomorphine (also effective in cases of homosexualism, heroin abuse and lack of initiative), lizurid (also anticonvulsant, increase cognitive function and memory, has antimigraine effect), rotigotine, amanthadine (also effective at group A flue, chronic fatigue, multiple sclerosis).
Subcortical vestibular nuclei dysfunction
result, besides the others, in adrenergic and serotoninergic disturbances. They are manifested in the forms of dizziness and vertigo, coordination and SOD, hypertension and limbic distortions. If mostly objective vertigo or pseudovertigo accompany pheochromocytome, migraine, brain blood circulation distortions, end arteriitis, Reynaud disease, acrocyanosis, initial stages of atherosclerotic gangrene, trophic ulcers of extremities, decubiti, hypertension with crisis, – they use alpha-adrenoblockers: terasosine, doxazozine (artezine), omnic or alphazozine.
In the danger of cardiac catastrophe, migraine, arrhythmia, stress consequences they use beta-adrenoblocking agents: atenolol, bisoprolol, betaxolol, methoprolol, nebivolol (influence brainstem vascular center), thalinolol, ethmolol, propranolol [37]. The details are described in specialized guidelines [7]. Dizziness, accompanied with emotional depressive disorders is managed with inhibitors of serotonine reuptake (ISSR): amytriptilline, triavil, imipramine, cephedrine, herfonal, damilene maleinate, clomipramine and especially last generation ISSR: ondasetron, dolasetrone, granisetrone, tropisetrone, alizapride (Vergentan).
In some countries they traditionally use tricyclic (TCAs): amitriptyline, amoxapine, clomipramine, desipramine, doxepin, imipramine, nortriptyline, protriptyline, trimipramine, – and tetracyclic (maprotiline, mirtazapine) antidepressants [37] In subcortical area research the high activity of endorphin, encephalin, dinorphine systems and substance P are found; their role in vestibular dysfunction formation is not established [249].
Cortical vestibular nuclei dysfunction
is leading to dramatic disturbance of GABA-glycine balance and thus excitation-inhibition processes [4]. Decrease of inhibitory GABA activity results in the distortion of all mediator systems activity, which is manifested clinically as neurotization, metabolism is impaired, different sicknesses of inner organs: renal, hepar, thyroid gland, – are revealed [266].
Among severe consequences are falls of the immunity [177], causing chronic infections: viral, bacterial, protozoal, autoimmune and oncologic diseases. Treatment at neurotization stage: GABA, histaminic blockers, in severe pathology – gaba-pentine, pregabalin, in therapy-resistant cases carbamasepin, valproat, lamotrigin [293]. Etifoxine, non-benzodiazepine anxiolytic, causes no dependence and withdrawal effects.
Understandable, that in the case of developed hypertension it is necessary to manage it, but it is obligatory to keep in mind, that in this case, so called “main diagnosis”, is in reality the consequences and not the reason [275]. Managing consequences the doctor does not stop the mainstream process.
Management of exact types of vestibular disorders
General principle: dizziness and vertigo
Dizziness is the disturbance of motion, space and time perception [48; 129]. Vertigo means illusion of non-existent movement most often rotatory, seldom swaying or linear forward-backward, from side to side, up and down. Vertigo is considered to be typical for cupulolythiasis, vestibular neuronitis (neuritis), Ménière’s disease and syndrome [249]. Dizziness is more typical for intoxications and chronic diseases.
From anatomical and physiological point of view vestibular analyzer consists of at least two systems: great type I hair cells, contacting with thick fibers, forming direct 3 neuron pathway to contralateral cortex and small type II hair cells innervated with thin fibers forming polysynaptic pathway. First system is responsible for vertigo sensation, second – for dizziness.
In the cases of vertigo calcium and Н1 histaminic receptor blockers are effective, even combinations of them do exist (for example Arlevert or Migraeflux). In dizzy patients more effective appear to be nootropic drugs [280]. In some patients combinations of dizziness and vertigo episodes and additional symptoms (migraine) are reported, beta-histine is the most effective [138].
Specific Dizziness types, SOD and related symptoms
Dizziness – distortion of space, motion and time perception. The authors do not share the popular viewpoint that “Most causes of dizziness are not serious and either cure themselves quickly or are easily treated”. There is a big bulk of evidence that dizziness predict severe pathology. Therefore, it needs careful examination and treatment.
The latter includes Ginkgo biloba extract (EGB 761, tanakan), piracetam, oxiracetam, cyticholine or nicotinomimetics, neurohomologous phosphlipids (gangliosides, phosphatidylserine, GMI), ACTH, tiocetam, mexidol, GABA-glycine balance regulation and amphetamines [92], dihydroergocristin and codergocorninmesilat, xantinolnicotinat [96]. Symptomatic treatment is indicated, if necessary.
Objective vertigo – feeling the subjects moving around the patient. Treatment: histaminic, calcium and muscarinic blockers, potassium salts, pergolide. Combination of histaminic and calcium blockers has potentiating effect [180]. Etiologic therapy is useful depending of disease characteristics: vestibular neuritis, Ménière’s disease etc.
Subjective vertigo – illusion of non-existent movement, patient feel him moving. Treatment: adrenoblockers, dopaminoblockers, histaminoblockers [249]. Patient needs wide scale examination; sometimes illusions of flying are accompanying chronic diseases, syphilis, tuberculosis, initiation of flue [125].
Giddiness – vertigo which is not similar to subjective or objective ones, sometimes called pseudovertigo: very intensive, difficult to describe, patients often tell that something is rotating inside of the head [213]. It has negative correlation with height (-0.4522). Positive correlation with complaints of nausea while headache spell is reported (0.6455). ECG: positive correlation with duration of QRS interval (0.5447). Treatment: noophen, cholinоlitics, beta-blockers, muscarinic blockers, beta-histin [138]. Histaminic blockers are to be used with ECG control if indicated.
Movement coordination disturbance (imbalance) sometimes is met separately. Patients are complaining of swaying, staggering, momentary loss of motion control… Treatment: nootrops, cholinomimetics mineral balance restoration. In many cases dopamine agonists are among the first medications to be considered [37].
Orthostatic – discomfort sensations appearing at abrupt standing up. Treatment: nicotinomimetic, tanakan, baclophen, estragon (green grass), zintona, serotonin blockers [217].
Kinetosis – symptom complex resulting from being in moving vehicles. Treatment: dimenhydrinate, calcium blockers, muscarinolitics, noophen, monoamines [156].
Acrophobia – discomfort appearing at the height or looking down from the height. Treatment in the case of vestibular dysfunction: calcium blockers, adrenoblockers, muscarinolitics, diuretics. In the case resulting of traumatic event – psychotherapy is indicated [300].
Agoraphobia – discomfort appearing at the opened places, markets, great squares, supermarket syndrome. Treatment: nootrops, adrenolitics, cholinolitics, histamine agonists [49; 52].
Nyctophobia – discomfort appearing at the darkness, twilights. Treatment: adrenergic and dopa agonists, nootrops, melatonin, muscarinolitics, potassium salts. Psychotherapy in psycho traumatic consequences is reported to be profitable [166].
Claustrophobia – discomfort appearing at the small closed places. Treatment: tanakan, beta-histine, monoamines, GABA [56]. Psychotherapy is useful in the case of specific phobia [49].
Ascendophobia – discomfort appearing during climbing up the hill or staircase. Patient note the need of visual control. ECG: expressed positive correlation with Р (0.7259) and PQ (0.6472). Treatment: nicotinomimetica, muscarinolitica, nootrops, potassium salts. Histamine blockers are to be used under control of ECG [277].
Descendophobia – discomfort appearing during descending down the hill or staircase. Patient note the need of visual control. It correlates positively with age (0.4037) and dyspnoe complaints (0.4461). ECG: expressed positive correlation with Р (0.7259) and PQ (0.6472), and negative with ST interval (-0.4082). Treatment: nootrops, adrenoblockers, serotoninoblockers, dopaminoblockers, GABA, muscarinolitics, ganglioblockers and potassium salts. Calcium and histamine blockers are contraindicated [277].
Optokinesis – discomfort appearing during optokinetic stimulation, train or car chain movement, solar rays blinking etc., has positive correlation with systolic (0.5202) and diastolic BP (0.5033). Treatment: calcium blockers, beta-blockers, ganglioblockers, ACE blockers, histaminic blockers, phenibut, GABA, hypotensive [277].
Nausea is defined as urge to vomiting. Treatment: menthol, isovaleric acid, GABA, monoamines, phenibut, ganglioblockers, histamine blockers, muscarinolitica, calcium blockers [249].
Vomiting – forceful evacuation of gastric contents outside. Treatment: menthol, isovaleric acid, muscarinolitics, rehydrating, antiemetics [211].
Headache, as a substitute of dizziness [246] has positive correlation with agoraphobia (0.4588). Treatment: phenibut, beta-histine (without aura), histaminic blockers (aura, cluster headaches), muscarinic blockers, beta-blockers, calcium blockers [101].
Black-out might appear at abrupt head movements, physical loadings or per se. ECG: positive correlation with duration of Р (0.5101) and complex PQ (0.6202). Being met with Brugada syndrome, in this case ajmaline and flecainide are used for treatment). Calcium and histaminic blockers are contraindicated. Therapy: nootrops, ganglioblockers, adrenolitics, GABA, potassium salts.
Tinnitus as substitute of dizziness has positive correlation with numbness (0.4462).
Claussen has identified four types of tinnitus:
- objective (vascular, sounds from muscles and joints, otoacustic emission), among others they differ tinnitus appearing after whiplash injury [306];
- endogenous (mostly characterizing neuro-sensory degeneration);
- exogenic (related to paroxysmal states, like migraine)
- slow brainstem degeneration [52].
ECG: positive correlation with physical loading (-0.4601) sometimes is met in cases of long QT or syndrome Jervell and Lange-Nielsen (rare disease, also accompanied with deafness from childhood, met from 1.6 to 6 per 1 million of population).
Treatment: tanakan, histamine agonists, nootrops, adrenolitics, muscarinolitics, potassium salts [54]. High protein low sugar and restriction of cholesterol intake is suitable for treatment of patients [41]. The treatment depends on the exact type. In the case of tinnitus as auditory psychiatric problem, antihallucination and anticonvulsive medications are effective [99].
Numbness – discomfort sensation of volunteer control loose over parts of body. Treatment: nootrops, GABA, ganglioblockers, adrenoblokers, muscarinolitics, calcium blockers [37].
3. Outcome from vestibular lesion
Basic mechanisms of the human compensation of disequilibrium with respect to the reparation processes within the human self regulation and neuronal plasticity, – in neurootology are discriminated as: restitution, adaptation, suppression, habituation, compensation [56].
Restitution
Restitution can be defined as complete reparation after a temporally limited lesion. For instance, after an inner ear infection with severe vertigo attacks, we observe at later investigations a complete recovery of all the measurable functions, due to a consequent anti-inflammatory and anti-infectious therapy. The patient then is cured and completely free from any further subjective complaints.
Adaptation
Adaptation means that the human equilibrium system can adapt him to physiologically as well as pathologically altered conditions. For instance, during the process of peripheral vestibular lesions of one side we observe that the sensitivity of the opposite vestibular receptor is counter regulated through a feedback-loop so that it nearly suits to the condition of leveled comparisons between both the inner ears. In the follow-ups during a monolateral peripheral vestibular loss we observe an opposite side depression in the caloric butterfly and a spontaneous nystagmus beating towards the lesion (Stenger’s Erholungsnystagmus). Thus, the functional adaptation after a severe peripheral vestibular lesion can precede the process of restitution.
Suppression
As being mentioned, the central regulatory system can alter the sensitivity of the vestibular, the retinal and other receptors for equilibrium regulations. In the case of an adaptation situation, we have also observed an extreme condition of this type of regulation, which we then have called “vestibular suppression”.
In the case of vestibular suppression, one finds that the central regulation suppresses complete lines of, for instance, ocular movement control in favor of the unaltered tracts, as can be proved by the calorization pendulum interference test. The regulation pattern of “suppression” sometimes also appears like a selective switch from one system to another.
Habituation
A compensation phenomenon, which includes a special learning program for movements or spatial situations, is called habituation. The habituation is defined by the reduction of the intensity and duration of the subjective vestibular reactions like vertigo and nausea in case of seasickness, as well as in the correction of days or overreactions of the sensory motor type with a nystagmus or head and body instability. In 1906, Abels related the reduction of seasickness during long time exposure on a boat to the habituation of the vestibular system. Bárány described functional reductions in ballet dancers, especially with respect to the decrease of the postrotatory nystagmus.
This learned reduction or blockage of physiological equilibrium reactions has to be stored in the central nervous system. It can also be forgotten after a while of not using it sufficiently. The habituation is not completely specific for one single vestibular stimulus. It also can be transferred from one type of stimulus to another. Habituation is also possible for optokinetic stimulus modalities. In many vertigo rehabilitation programs, habituation is the goal for a compensatory recovery.
Compensation
The term compensation describes another type of central nervous counter regulation against a functional deterioration through a vestibular or other equilibrium lesion. It utilizes supplementary functions, which are added so that an overlay of additionally activated functions covers the underlying equilibrium lesion by means of its neuronal plasticity.
However, the primary lesion continues to exist and in case of a special conflict it can come to the surface of clinical phenomenology again. By means of an intermediate neuronal plasticity on the level of the vestibular nuclei, a peripheral vestibular lesion, for instance, which is primarily visible in the monolateral caloric inhibition in the butterfly calorigram as well as in the deviation towards the side of the lesion in the step-test cranio-corpo-gram, after a while only can be continuously verified in the calorigram?
However, the cranio-corpo-graphy of the vestibular spinal step-test-movement develops towards a regular normal picture without any further deviation, neither towards the right nor to the left, and without any pathology in the CCG sway patterns.
J. Vestibular rehabilitation
Vestibular rehabilitation has to be performed according to the severity of preliminary disease. Stages 1 to 3 in the cases of satisfactory outcome may pass rehabilitation in non-specialized rehabilitation centers, doctor of 3 level education is obligatory, Uemura test is to be used with videorecording for admittance argumentation, monitoring and documentation of management quality. Stages 4-5, no matter of outcome have to pass rehabilitation at the specialized Dizziness Rehabilitation Centers, corresponding to minimum requirements of stage 3 Dizziness center.
Release from information and vestibular overloading
It means thinking about eternity, self estimation, music, arts, auto training, gazing of natural beauties. Informational relaxation means visiting some kinds of islands, which have no civilization impact: loud music, TV, handies. It predisposes listening natural noises, waterstreams, leaves of the trees and bushes, sounds of the silence. It is directed to gaze the wild nature: rocks and mountains, valleys and forests, flower beds.
It calls the patient to refuse temporary from cheapses, sweet drinks, heavy fats and be involved in simple ‘Mediterranean’ diet with increased proportion of vegetables and seafood. Visiting of art exhibitions and listening relaxing classical music need special indications. If patient has hyperacusia – music therapy is contraindicated. In many cases reestimation of priorities is important. In modern megapolices we forget, that our main purpose is life and not carrier, money, glory, power. Many patients need special autotraining, helping them to control better their body functions and their relations in socium: relatives, colleagues.
Physiotherapy. Modern sanatoriums are full with devises for these procedures. Problem is that they are appointed to be beneficial for the patient, though in reality they are not. Therefore, it is important to regard exactly the strictly established indications and contraindications.
Indications depend on the pathology and procedure type. If phonation improves performance of Uemura test, it is indication to use music therapy. Absence of meteosensitivity means some possibility to use electric and magnetic procedures. Final decision must be taken after Uemura test with electromagnetic loading. It is performed in the next manner.
First, videoregistration of Uemura control is recorded. Then patient has 5 minutes music in the earphones (phonation) or listening of advertisement through mobile phone (electromagnetic field stimulation). At once after loading stop Uemura test performance is recorded. Equivalent or improved result is indication to the procedure.
Contraindications are opposite to indications. Meteosensitivity, intolerance to magnetic fields, susceptibility to sounds are subjective contraindications to sound and electromagnetic based procedures. Uemura test is objective document for contraindication of music, electromagnetic procedures. Contraindication for aroma therapy is impairment of Uemura test performance after inhaling some fragrance (usually citron smell).
Contraindications for physical exercises are derived from ECG with physical and neurological loadings. For example, swimming is dangerous for elder patients with increase of heart rate more then 20 beats per minute at any of the loadings.
Physical training types are classified into: static, dynamic and coordinating training. The latter might be classified into three subtypes:
General – means sport games, depending on age and fitness condition of the patient. Among others, tennis, ping-pong, billiard have shown their beneficial health impact.
Specific individual rehabilitation depends on particular defects of coordination. It considers the outcome from the lesion developed in the course of the disease. For example, young lady after herpetic infection has developed an unusual syndrome. In the study with the help of combination of cranio-corpo-graphy with nystagmography, when she was raising her left foot, her right eye was moving medially. Beneficial for her appeared half hour once per two days beating the ball against the wall with one and then with the other foot.
Biofeedback – today there are plenty of industrial produced posturographic platforms and coordination devices, proposing coordination improvement with the help of visual, acoustic and even tactile and gustatory keys. Their use has to be accompanied with full-scale vestibular function monitoring, including VestEP, CCG-NY, ECG with neurological loadings.
K. State of arts
In the modern world more than 20% population suffer from dizziness, only about 1% of vertigo patients benefit from professional treatment [67; 176]. Cardiologist, endocrinologist, oncologist, etc., space orientation disorders, usually manage dizziness; acrophobia, claustrophobia and others are in better cases are managed by psychiatrist; all of them neglect vestibular components of the disorder.
Dizziness and vertigo diagnostic is concentrated only at one projection: vestibulo-motor. Vestibulo-cortical projection is ignored throughout the whole world. There are not more than 3 centers, which use irregularly vestibular evoked potentials. In most studies vestibular diagnostics is based at Romberg test, the sensitivity of which does not exceed 40% [70]. Only few centers use cranio-corpo-graphy [50], based at Unterberger-Fukuda test, sensitivity of which exceeds 90%. Uemura test is used in unique laboratories irregularly, for scientific and not clinical purposes. Tests for vestibulo-vegetative and vestibulo-limbic projection studies are not used [274], though literature resources are full with articles about “cardioneurosis” (cf. Google search of this item).
Taking into consideration especial spread of the pathology it is obvious that no one, even best organized country healthcare, can manage the situation. It is important also to underline that dizziness is not considered to be mortality risk and, therefore, is neglected by patients and medical stuff, moreover, in many cases it is not managed by professionals. Today scientific progress results in the increase of the amount of people, complaining of dizziness. In most cases dizziness predicts severe pathology: cardiovascular, autoimmune, endocrine diseases, tumors [275].
L. Steps to be started
All this means that we have to organize the problem management, involving wide public involvement in the process. The necessary steps are:
- Spreading knowledge about vestibular system in general public.
- Training of the doctors of all specialties has to include knowledge about dizziness. Uemura test and typical case histories of vestibular disorders has to be familiar to every family doctor.
- All the ENT and neurologists have to know 20-point test battery at least; all the hospitals must have at least cranio-corpo-graphy, better with VestEP.
- It is important to start implementation of the methods with early high (more than 90%) sensitivity and diagnostic significance world-wide (vestibular evoked potentials, cranio-corpo-graphy).
- It is necessary to organize a network of regional Neurootological Centers with full scale complex of methods: VestEP, cranio-corpo-graphy, ECG and pupillometry.
- It is necessary to create International Coordination Centers with WHO patronage to introduce standards for diagnostics and management of dizzy patients.
- Monitoring of the situation word-wide is necessary with full-scale complex of methods or at least established standards.
M. Literature
- Abakarov AT. Vestibular projections to the temporal cortex of cat. Neurophysiology (Kiev). (in Russian). 1983. Vol. 15, № 2, 135-144.
- Abraham L., Potegal M., Miller S. Evidence for caudate nucleus involvement in an egocentric spatial task: return from passive transport. Physiol. Psychol. 1983, №11, 11-17.
- Alpini D. The Italian vestibular rehabilitation protocols. Neurootol. Newsletter. 1994, Vol.1, № 1, 54-67.
- Alvarez MVG. Understanding drug-induced Parkinsonism. Neurology 2008, 70, e32-e34.
- Antipova SI., Korshunov VM., Polyakov SM. Mortality of liquidators in Belarus. 2nd International Conference: Long-term health consequences of the Chernobyl disaster, 1998, 10-11.
- Arnolds D.E.A.T., Lopes da Silva F.H., Boeijinda P., Kamp A., Aitink W. Hippocampal EEG and motor activity in the cat: the role of eye movements and body accelerations. Behav. Brain. Res. 1984, Vol. 12, 121-135.
- Aronow WS., Fleg JL., Pepine CJ. ACCF/AHA 2011 Expert Consensus Document on Hypertension in the Elderly. J American Coll. Cardiol. 2011, Vol. 57, №20, 80 p.
- Ashton J.A., Boddy A., Donaldson I.M.L. Input from proprio-receptors in the extrinsic ocular muscles to the vestibular nuclei in the giant toad, Bufo marinus. Brain Res. 1984, Vol. 53, 409-419.
- Aviation medicine (Guidelines, in Russian). Rudny NM., Vasiliev PV., Gozulov SA. (eds.), Moscow, Medicine. 1986, 579 P.
- Baker R .R., Mather J.G., Kennaugh J.H. Magnetic bones in human sinuses. Nature. 1983, Vol. 301, № 5895, 78-80.
- Balch PA. Prescription for nutritional healing. Penguine Group Inc., NY, Toronto, London, 2006, 896 P.
- Baloh R.W., Kerber K.A. Clinical neurophysiology of vestibular system. Oxford University Press, Oxford, NY. 2010, 456 p.
- Barany R. Untersuchungen über den vom Vestibularapparat des Ohres reflektorisch ausgelösten rhythmischen Nystagmus und seine Begleiterscheinung. Mschr. Ohrenheilk. 1906, 40, 193-297.
- Barber HO., Sharpe JA. Vestibular disorders. Year Book Medical publishers. Chicago. 1988, 282 p.
- Basta D., Clarke A., Ernst A., Todt I. Stance performance under different sensorimotor conditions in patients with post-traumatic otolith disorders. J. Vestib. Res., 2007, 17, 1, 25-31.
- Bauer U. Etude clinique de l’extrait de Ginkgo biloba dans arterite des membre inferieurs. Essai a double insu face au placebo sur 6 mois. Arzneim. Forsch. Drug. Res. 1984, 34, 6, 716-720.
- Bensley EH., Joron G.E. Handbook of treatment of acute poisoning. Williams &Wilkins, Baltimore, 1963, 227 P.
- Benson A.J., Spenser M.B., Stott J.R. Thresholds for the detection of the direction of whole-body linear movement in the horizontal plan. Aviat. Space. Environ. Med. 1986, Vol. 57, 1088-1096.
- Bergenius J., Borg E., Hirsch A. Stapedius reflex test, brainstem audiometry and optovestibular tests in diagnosis of acousticus neurinomas. A comparison of test sensitivity in patients with moderate hearing loss. Scand Audiol. 1983, Vol. 12, P. 3-9.
- Bermingham NA., Hassan BA., Price SD., Vollrath MA., Ben-Arie N., Eatock RA., Bellen HJ., Lysakowski A., Zaghbi HY. Math1 : an essential gene for the generation of inner ear hair cells. Science, 1999, 284, 1837-1841.
- Bertora G., Bergmann J. Doppler sonography in vertigo patients. In: Vertigo, nausea, tinnitus and hearing loss in cardio-vascular diseases. Claussen C.-F., Kirtane M.V (eds.) Excerpta Medica. Amsterdam-New York-Oxford, 1986, 25-30.
- Biswas A. Clinical audio-vestibulometry for otologists and neurologists. 3rd edition. Bhalani Publishing house. Mumbai, 2002, 178 P.
- Black F.O. Vestibular function assessment in patients with Ménière’s disease: the vestibulospinal system. Laryngoscope. 1982, Vol. 92, № 12, 1419-1436.
- Bobrov V., Trinus K., Frolov G., Zalessky V. Vestibulo-dependence tachyarrhythmia: laser biostimulation therapy of the paroxysmal supraventricular tachycardia. XIIIth Ann. Joint Meeting Electroencephalogr. Clin Neurophysiol. Prague, 1990.
- Bodnar P.M., Peshko A.O., Krymovska O.P. Diagnostic importance of long latency multisensory evoked potentials (MEP). Neurootol. Newsletter. 2002, Vol. 6, № 1, P. 117.
- Bodo G. Connection between the vestibular and circulatory systems (a clinical study). In: Vertigo, nausea, tinnitus and hearing loss in cardio-vascular diseases. Claussen C.-F., Kirtane M.V. (eds.) Elsevier Science Publishers BV. Excerpta Medica. Amsterdam-New York-Oxford, 1986, 19-23.
- Bojrab DI., Stockwell CW. Electronystagmography and rotation tests. In: Neurotology. Jackler RK., Brackmann DE. (Eds.). Mosby. St.Louis, Baltimore, Boston. 1994, 219-228.
- Bolton P.S, Kerman I.A, Woodring S.F, Yates B.J. Influences of neck afferents on sympathetic and respiratory nerve activity. Brain Res. Bull. 1998, Vol. 47, № 413, 19.
- Bossnev W., Popova D., Daskalov M., Chalmanov W. Neurovegetative disorders, vertigo and nausea in metabolic diseases. In: Vertigo, nausea, tinnitus and hypoacusia in metabolic disorders. Claussen C.-F., Kirtane MV., Schlitter K (eds.) Elsevier Science Publishers BV. 1988, 235-240.
- Boyd A. Bromocriptine and psychosis: a literature review. Psychiatric Quarterly. 1995, 66, 1, 87–95. doi:10.1007/BF02238717. PMID 7701022. Retrieved 2008-09-06.
- BradleyW. E., Teague C.T. Cerebellar influence on the nicturition reflex. Experimental. Neurol. 1969, Vol. 23, 3, 399-411.
- Brandt T, Schautzer F, Hamilton DA, Bruning R, Markowitsch HJ, Kalla R, Darlington C, Smith P, Strupp M. Vestibular loss causes hippocampal atrophy and impaired spatial memory in humans. Brain. 2005 Nov;128(Pt 11):2732–41. Epub 2005 Sep 1. PMID 16141283
- Brevern von M., Radtke A., Lezius F., et al., Epidemiology of benign paroxysmal positional vertigo: a population based study. J. Neurol Neurosurg Psychiatry, 2007, 78, 710.
- Bricout-Berthout A., Caston J., Reber A. Influence of stimulation of auditory and somatosensory systems on the activity of vestibular nuclear neurons in the frog. Brain Behav. Evol. 1984, Vol. 24, 21-34.
- Brodal A. Anatomy of the vestibular nuclei and their connections. Vestibular system. PI Basic mechanisms. Handbook of sensory physiology. Springer. New York, 1974, Vol. 6, 240-351.
- Bruderman I., Stern S., Braun K. Respiratory effects of intravenous lobeline in normal subjects and in patients with mitral stenosis. Br. Heart J. 1966, 28, 6, 740-745.
- Brunton L., Chabner B., Knollman B. Goodman and Gilman’s The pharmacological basis of therapeutics. Twelfth edition. McGrow Hill Medical. NY. 2006, 1991 p.
- Bryan AS., Bortolami SB., Ventura J., DiZio P., Lackner JR. Influence of gravitoinnertial force level on the subjective vertical during recumbent yaw axis body tilt. Exp. Brain Res. 2007, 183, 3, 389-397.
- Burgess A., Kundu S. Diuretics for Ménière’s disease or syndrome. Cochrane database of systematic reviews. 2006, Issue 3, Art №:CD003599. DOI: 10.1002/14651858.CD003599.pub.2.
- Buyukavci M., Olgun H., Ceviz N. The effects of ondasetron and gravicetron on electrocardiography in children receiving chemotherapy for acute leukemia. Am. J. Clin. Oncol. 2005, 28, 2, 201-204.
- Caovilla HH., Ganança MM., Ganança F., Serafini F. Nutritional diet in the treatment of tinnitus. Neurootol. Newsletter. 2002, Vol. 6, №1, 58-59.
- Casagrande V.C, Kuhn A.M.B. The psychogenic vertigo and its treatment: a case study. Neurootol. Newsletter. 2002, Vol. 6, № 2, 11-13.
- Cazals Y., Aran J.-M., Erre J.-P., Guilhaume A., Aurousseau C. Vestibular acoustic reception in the guinea pig: a saccular function? Acta Otolaryngol. – 1983. – Vol. 95. – P. 211-217.
- Chen H., Tung Y-C., Li B., Iqbal K., Iqbal I-G. Trophic factors counteract elevated FGF-2 induced inhibition of adult neurogenesis. Neurobiology of aging, 2007, 28, 1148-1162.
- Clarke A., Kornilova L., Ocular torsion response to active head-roll movement under one-g and zero-g conditions, J Vestib Res. 2007, 17, 2-3, 99-111.
- Claussen C.-F. Die quantitative Vestibularisprüfung – Eine audiogrammanaloge Auswertung von Nystagmusbefunden (Schmetterlingsschema). Z.Laryng.Rhinol. 1969, 48, 938.
- Claussen C.-F. Statistische Standards besüglich des Symptomes Schwindel in der Bundesrepublik Deutschland aus der Sicht der Neurootologie. In: Differential diagnosis of vertigo. Claussen C.-F. (ed.). Walter de Gruyter & Co., Berlin, New York. 1980, 588-605.
- Claussen C.F. Schwindel, symptomatik, diagnostik, therapie. – Hamburg, Edition m+p. Dr. Werner Rudat und Co, 1983. – 225 p.
- Claussen C.-F. Der Schwindelkranke Patient. Grundlagen der Neurootologie und Äquilibriometrie. Hamburg. medicin+pharmacie. Dr. Werner Rudat & Co. 1992, 143 Z.
- Claussen C.-F. Cranio-Corpo-Graphy (CCG) – 30 years of equilibriometric measurements of spatial and temporal head, neck and trunk movements. In: Equilibrium Research, Clinical Equilibriometry and Modern Treatment. (Eds.) Claussen C.-F., Haid C.T, Hofferberth B., Exerpta Medica, International Congress Series 1201, Elsevier Science B.V., Amsterdam, Netherland. 2000, 245–259.
- Claussen C.F. Neurootologische Aspekte des HWS-Schleudertraumas. Schwindel aus interdisziplinaerer Sicht, (Haid C.-T. editor). Georg Thieme Verlag. Stuttgart, New York, 2003, 187-198.
- Claussen C.F., Bergmann J.M., Bertora G.O. Equilibriometría y Tinnitología Práctica. 4-G-FORSCHUNG E.V. D-97688 Bad Kissingen, Alemania, 2009, 206.
- Claussen C.-F., Claussen E. About the strength of the neck in linking the head to the trunk as measured by the US-CCG. Excerpta Medica, International Congress Series, 1133, Elsevier Publishers, Amsterdam, Lausanne, New York, Oxford, Shannon, Tokyo, 1996, p.9–20.
- Claussen C.-F., Claussen E., Böcking HH., Patil NP. Extractum Ginkgo biloba in the combined treatment of vertigo, nausea and tinnitus. In: Vertigo, nausea, tinnitus and hypoacusia in metabolic disorders. Claussen C.-F., Kirtane MV., Schlitter K (eds.) Elsevier Science Publishers BV. 1988, 583-590.
- Claussen C.-F., Constantinescu L. Late whiplash Injury Syndrome. Claussen C.-F., Constantinescu, L. Equilibriometric Invesstigations. In (Ed.). DeSa-Souza S., Claussen C.-F. Modern Concepts of Neurootology. PRAJAKTA, BOMBAY, 1997, p. 351 -360.
- Claussen CF., Franz B. Contemporary & practical neurootology. Solvay, Hannover, 2006, 410p.
- Claussen C.F., Koltschev, Chr., Bergmann de Bertora J.M., Bertora G.O. Los potenciales evocados equilibriometricos por medio del BEAM y su importancia en el diagnostico y tratamiento de los pacientes von vertigo. From: Sacritan Alonso, T., Bartual, J.: Compenscion vestibular y Vertigos. – XV. Congreso Nacional de la Sociedad Espaniolo de ORL, Cadiz, 1993, 27–45.
- Claussen C.-F., Schneider D., Büky B. Über den Einsatz des Brain Electrical Activity Mapping in der Neurootologie. Wiss.Z.Humboldt-Univ., Reihe Medizin, Neurootologie, 1990, Jg. 39, 322-323.
- Claussen E., Claussen C.F. The combined neurootological pharmacotherapy in old age vertigo. Vertigo, nausea, tinnitus and hearing loss in central and peripheral vestibular diseases. Claussen C.F., Sakata E., Itoh A. (Eds.). Elsevier, Amsterdam-Lausanne-New York, 1995, 149-152.
- Committee on Hearing and Equilibrium. Guidelines for the diagnosis and evaluation of therapy in Ménière’s disease. Otolaryngology – Head and Neck Surgery. 1995, 113, 181-185.
- Constantinescu L., Schneider D., Claussen C.-F. The influence of betahistin on the vestibular evoked potentials in patients with peripheral disorders. Ribari O., Hirschberg A. (Eds.). Proceed. 3rd EUFOS Congress, Budapest 1996, Monduzzi Editore, Bologna. 1996, p. 95 – 98.
- Curaj A., Scott P., Vlasceanu A., Wilson L. European Higher Education at crossroads: between Bologna process and national reforms. Part 1. Springer Science+Business Media. 2012, 1099 p.
- Dallos P., Fakler B. Prestin, a new type of motor protein. Natl. Rev. molecular cell biol., 2002, 3, 104-111.
- David A., Fleminger S., Kopelman M., Lovestone S., Mellers J. Lishman’s organic Psychiatry: a textbook of neuropsychiatry. John Wiley & Sons. Wiley-Blackwell. Singapore 2007.
- DeLucchi E. Tinnitus, hypoacusia and vertigo in hyperuricemia. In: Vertigo, nausea, tinnitus and hypoacusia in metabolic disorders. Claussen C.-F., Kirtane MV., Schlitter K (eds.) Elsevier Science Publishers BV. 1988, 241-248.
- DeLucchi E. Vertigo equivalent migraine. Giddiness & vestibulo-spinal investigations. Combined audio-vestibular investigations. Experimental neurootology. Claussen C.F., Kirtane M.V., Constantinescu L., Schneider D. (Eds.). 1996, 401-406.
- Desmond AL. Vestibular function: evaluation and treatment. Thieme, New York, Stuttgart, 2004, 228p.
- Diener HC., Montagna P., Casc G., Lyczak P., Schumann G., Zöller B., Muldler LJMM., Siegel J., Edson K. Efficacy and tolerability of diclofenac potassium sachets in migraine: a randomized, double-blind, cross-over study in comparison with diclofenac potassium tablets and placebo. Cephalalgia. 2006, 26, 537-547.
- Dietrich M. Funktionelle Bildgebung des vestbulären Systems. In: Hören und Gleichgewicht. Im Blick des Gesellschaftlichen Wandels. 7. Hennig Symposium. Heidelberg. Springer Wien NY. 2010, 95-101.
- Di Fabio R.P. Sensitivity and specificity of platform posturography for identifying patients with vestibular dysfunction. Phys. Ther. 1995, 75, 4, 290-305.
- Easterly C.E. Cardiovascular risk from exposure to static magnetic fields. J. Am. Ind. Hyg. Assoc. 1982, 43, 533-539.
- Electromagnetic fields and public health: Electromagnetic Hypersensitivity, World Health Organization (WHO) 2005, factsheet 296.
- Farfan H.T., Gracovetsky S. The nature of instability. Spine. 1984, Vol. 9, № 7, P. 714-719.
- Fisher A.A., Foreit J.R., with Laing J., Stoeckel J., Townsend J. Designing HIV/AIDS intervention studies. An operation research handbook. The Population Council Inc. 2002, 141 p. ISBN 0-87834-107-2
- Fishman JM., Burgess C., Waddell A. Corticosteroids for the treatment of idiopathic acute vestibular dysfunction (vestibular neuritis). Cochrane Database Syst Rev. 2011 May 11, 5, CD008607. doi: 10.1002/14651858.CD008607.pub2.
- Fleming DM. Zanamivir in the treatment of influenza. Expert Opin. Pharmacother. 2003, 4, 799-805 http://amedeo.com/lit.php?id=7050702
- Foerster BR., Petrou M., Lin D., et al., Neuroimaging evaluation of non-accidental head trauma with correlation to clinical outcomes: a review of 57 cases. J. Pediatr. 2009, 154, 573-577.
- Frank C., Brown S. Practice tips. Treating vertigo in the office. Particle repositioning maneuver. Can Fam Physician. 2000, 46, 2395–2397. PMCID: PMC2145003
- Frisina W. Study of cradle and a pendulum motion for applications to health care. Biomechanics. 1984, Vol. 17, № 8, 573-577.
- Froehling DA., Bowen JM., Mohr DN., Brey RH., Beatty CV., Wollan PC., et al. The canalith repositioning procedure for the treatment of benign paroxysmal positioning vertigo: a randomized controlled trial. Mayo Clinic Proceedings. 2000, 75, 7, 695-700.
- Fukuda T. The stepping test: 2 phases of the labyrinthine reflex. Acta Otolaryng (Stockh.). 1959, 50, 95-108.
- Furman J.M.R., Wall C. III, Kamerer D.B. The simultaneous binaural bithermal caloric test: an evaluation using receiver-operator characteristic methodology. In: Vestibular disorders. Barber H.O., Sharpe J.A (eds.). 1988, 71-86.
- Gacek R.R. The anatomical-physiological basis for vestibular function. In: Nystagmus and vertigo: Clinical approaches to the patient with dizziness. Honrubia V (Ed.). New York: Academic Press. Inc., 1982, 3-23.
- Gacek R.R. Anatomy of the central vestibular system. In: Neurotology. Jackler RK., Brackmann DE. (Eds.). Mosby, St.Luis, Baltimore, Boston. 1994, 41-58.
- Ganong WF. Review of medical physiology. The McGrow Hill Companies Inc., NY. 20th edition, 2001, 766 p.
- Garcia F.V., Garcia C. Vertigo, dizziness and imbalance: the concepts. Basics on vertigo, dizziness and imbalance. Garcia C, Garcia FV, Coelho H, Pimentel J (Eds.). Ass. Portuguesa Otoneurol., 1999, 15-17.
- Gavalas G., Vathilakis I., Dokianakis G., Papazoglou G. Vertigo and otosclerosis. In: Vertigo, nausea, tinnitus and hypoacusia in metabolic disorders. Claussen C.-F., Kirtane MV., Schlitter K (eds.) Elsevier Science Publishers BV. 1988, 259-264.
- Gensemer IB., Smith JL., Walker JC., McMurry F., Indeck M., Brotman S. Psychological consequences of blunt head trauma and relation to other indices of injury. Ann. Emergency Med. 1989, 18, 1, 9-12.
- Graybiel A., Kellogg R.S. Inversion illusion in parabolic flight: its probable dependence on otolith function. Aerospace Medicine, 1967, 38, 1099-1103.
- Grigoriev YuG., Stepanov VS. Relationship between condition of rabbit vestibular analyzer and their individual radioactive sensitivity during irradiation in the dose of 150 Gr. (in Russian) Radiobiology. 1983. Vol. 23, № 4, 549-551.
- Grüsser OJ., Pause M., Schreiter U. Localization and responses of neurons in parieto-insular cortex of awake monkeys (Macaca fascicularis). J. Physiol. (London), 1990, 430, 559-583.
- Guidetti G. La basi razionali della terapia delle vertigini. Ist. Clin. Otolaryngoiatrica Univ. Modena, 1988, 71 p.
- Hahn A. Audiovestibular findings in patients with Ménière’s disease. In: Vertigo, nausea, tinnitus and hypoacusia in metabolic disorders. Claussen C.-F., Kirtane MV., Schlitter K (eds.) Elsevier Science Publishers BV. 1988, 277-281.
- Hahn A., Derzeitige Stand der medikamentösen Therapie der Ménière’schen Erkrankung. In: Der Gleichgewichtsinn. Neues aus Forschung und Klinik. Schere H. (ed.) 6 Hennig Symposium. Springer. Wien, New York., 2008, 159-168.
- Haid T. Surgical treatment of vertigo. In: Vertigo, nausea, tinnitus and hypoacusia due to head and neck trauma. Claussen C.F., Kirtane M.V. (Eds.). Elsevier Science Publishers., 1991, 11-26.
- Halama P. Schwindel – Moderne Diagnostik und Therapie – Presbivertigo. Neurootol. Newsletter. 1995, Vol. 2, №1, 62-66.
- Hallpike C.S. Die Kalorische Prüfung. Pract. Otorrhinolaryng. 1955, 17, 301.
- Hamann K-F. Motion sickness. In: European manual of medicine Arnold W., Ganzer (Series eds.): Otorhinolaryngology, head and neck surgery. Anniko M., Bernal-Sprekelsen M., Bonkowsky V., Iurato S. (Eds.). Springer. 2009, 144-146 P.
- Haralanov S., Claussen C.-F. On the hallucinatory nature of tinnitus sensation: implications for the treatment approach. Neurootol. Newletter. 2002, Vol. 6, №1, 21-26.
- Haralanov H., Sachanska Th., Haralanov S., Popova N. Vegetative dysfunction, vertigo and orthostatic coolapse in sea sickness. In: Vertigo, nausea, tinnitus and hearing loss in cardio-vascular diseases. Claussen C.-F., Kirtane M.V. (eds.) Elsevier Science Publishers BV. Excerpta Medica. Amsterdam-New York-Oxford, 1986, 207-213.
- Harker LA. Migraine. In: Neurootology. Jackler RK & Brackmann DE (Eds.). Mosby. St.Louis, Baltimore, Boston. 1994, 463-469.
- Harker Y.A., Rassekh C. Migraine equivalent as a cause of episodic vertigo. Laringoscope – 1988. – Vol. 98. – P. 160-164.
- Hart CWJ. Medico-legal aspects of balance: US perspective. Neurootol. Newsletter. 1998, Vol. 3, №1, 86-95.
- Helbling B., Stamenic I., Viani F., Gonvers GG., Dufour JF., Reichen J., Cathomas G., Steuerwald M., Borovicka J., Sagmeister M., Renner EL. Interferon and amantadine in naïve chronic hepatitis C: a double-blind, randomized, placebo-controlled trial. Hepatology, 2002, 35, 2, 447-454.
- Hilton MP., Pinder DK. The Epley (canalith repositioning) maneuver for benign paroxysmal positioning vertigo. Cochrane database of systematic reviews. 2004, Issue 2, Art. No.: CD003162. DOI: 10.1002/14651858.CD003162.pub2.
- Hirsch Jr.W.L., Curtin HD., Imaging of the lateral skull base. In: Neurotology Jackler RK & Brackman DE, (eds.), Mosby, St.Louis, Baltimore, Boston, 1994, 303-340.
- Hong Z., Moessler H., Bornstein N., et al., A double-blind, placebo-controlled, randomized trial to evaluate the safety and efficacy of cerebrolysin in patients with acute ischemic stroke in Asla-Casta. Int. J. Stroke. 2009, 4, 406-412.
- Hoover S. Ménière’s migraine and allergy. In: Vertigo, nausea, tinnitus and hypoacusia in metabolic disorders. Claussen C.-F., Kirtane MV., Schlitter K (eds.) Elsevier Science Publishers BV. 1988, 293-300.
- Horn K.M., Miller S.W., Neilson H.C. Visual modulation of neuronal activity within the rat vestibular nuclei. Exp. Brain Res. 1983, Vol. 52, 311-313.
- Howells DW, Donnan GA. Where Will the Next Generation of Stroke Treatments Come From? PLoS Med. 2010, 7, 3. e1000224. doi:10.1371/journal.pmed.1000224.
- Hughes GB., Pensak ML. Clinical otology. Thieme. NY. 2007, 531 P.
- Hunt WT, Zimmermann EF, Hilton MP. Modifications of the Epley manoeuvre for benign paroxysmal positional vertigo (BPPV) Cochrane summaries. Published Online: April 18, 2012.
- Intercollegiate Stroke Working Party. National clinical guideline for stroke, 3rd edition. London: Royal College of Physicians, 2008, 187 p.
- Irvine N. Definition, epidemiology and management of electrical sensitivity. Report for the Radiation Protection Division of the UK Health Protection Agency, 2005, HPA-RPD-010.
- Ishikawa S., Ozawa H., Aoki S., Miyata M. Disturbed balance in chronic organophosphate intoxication. Vestibular and visual control on posture and locomotion equilibrium. 7th Int. Symp. Int. Soc. Postulography. Igarashi M., Black F.O. (Eds.). Karger, Basel, 1985, 295-301.
- Izmerov N. Combined effects of industrial and environmental factors: some effects of methodology and practice. Recent advances in researches on the combined effects of environmental factors. Manninen O. (ed.) ISCEF, Tampere. 1988, 41-50.
- Jackson CA. Dynamic posturography. In: Neurotology. Jackler RK., Brackmann DE. (Eds.). Mosby. St.Louis, Baltimore, Boston. 1994, 241-250.
- Jaju B.P., Wang S.C. Effects of Diphenhydramine and Dimenhydrinate on Vestibular Neuronal Activity of Cat: A Search for the Locus of Their Antimotion Sickness Action. Journ. Pharmakol. Exp. Ther. 1971. 176, 718-724.
- James AL., Burton ML. Betahistine for Ménière’s disease or syndrome. Cochrane Database of Systematic Reviews. 2001, Issue 3. Art No.: CD001873. DOI. 10/1002/14651858.CD001873.
- Jones R. (ed.) Oxford textbook of primary medical Care. Vol.1: Principles and concepts. Oxford University Press., 2005, 631.
- Jonsson I., Hydén D., Ödkvist L., Grandien M., Windström A. Otoneurological disturbances of viral origin. In: Differential diagnosis of vertigo. Claussen C.-F. (ed.). Walter de Gruyter & Co., Berlin, New York. 1980, 152-165.
- Kallinen J., Aantaa E. Intratympanic injection of lidocaine in the therapy of Ménière’s disease. In: Vertigo, nausea, tinnitus and hypoacusia in metabolic disorders. Claussen C.-F., Kirtane MV., Schlitter K (eds.) Elsevier Science Publishers BV. 1988, 539-542.
- Kaminskaya TA., Alexandrova MS., Pavlovsky LP. About the use of complex neurootological examination in the diagnostics of herpes virus infection in military stuff and their family members. In: Modern informational and energy preserving technologies for human vitality (in Russian). FADA Ltd., Kyiv, 2000, Vol. 7, 426-428.
- Kaniecki R, Lucas S. Treatment of primary headache: preventive treatment of migraine. In: Standards of care for headache diagnosis and treatment, National Headache Foundation. 2004, 40-52.
- Kaplan HI., Saddok BJ. Pocket handbook of clinical Psychiatry. Williams & Wilkins a Waverly Company, Baltimore, 1998, 505 p.
- Karlin A. Chemical modification of the active site of the acetylcholine receptor. Gen. Physiol. 1969, Vol. 54, № 1, part 2, 245-254.
- Kast R., Lankford JE. Otolithic evoked potentials: new techniques for vestibular studies. Acta Otolaryngol. 1986, Vol. 102, 175-178.
- Kehaiov AN. Influences vestibulaires sur la fonction auditive de malades atteints de troubles vestibulaires. Revue de Laryngologie. 1977, Vol. 98, № 9-10, 471-480.
- Kehaiov A. Raum, Zeit, Bewegung- Vestibular-, Seh- und Gehör-Wahrnehmungen. Claussen C.-F. Statistische Standards besüglich des Symptomes Schwindel in der Bundesrepublik Deutschland aus der Sicht der Neurootologie. In: Differential diagnosis of vertigo. Claussen C.-F. (ed.). Walter de Gruyter & Co., Berlin, New York. 1980, 481-520.
- Kehaiov A. Changes of the serum parameters under vestibular effect. In: Vertigo, nausea, tinnitus and hearing loss in cardio-vascular diseases. Claussen C.-F., Kirtane M.V (eds.) Excerpta Medica. Amsterdam-New York-Oxford, 1986, 221-226.
- Kevin A., Kerber A., Fendrick M. The Evidence Base for the Evaluation and Management of Dizziness. J Eval Clin Pract. 2010, 16, 1, 186-191.
- Khomaziuk ТА, Yegorov К.Y. General medical practice: dizziness in females with arterial hypertension. Zdorovia Ukraїny, 2010, №3, 1-3.
- König P., Waanders R., Witzmann A., Lanner G., Haffner Z., Haninec P., Gmeinbauer R., Zimmermann-Meinzingen S. Cerebrolysin in Traumatic Brain Injury – a pilot study of a neurotrophic and neurogenic agent in the treatment of acute traumatic brain injury. J. Neurol. Neurochir. Psychiatr. 2006, 7, 3, 12-20.
- Korner A.F., Schneider P., Forrest T. Effects of vestibular proprioceptive stimulation on the neurobihavioral development of preterm infants: a pilot study. Neuropediatrics. 1983, Vol. 14, 170-175.
- Kornilova L.N. Vestibular function and sensory interaction under the condition of altered gravity. Advances in Space Biology and Medicine, JAI PRESS INC. 1997, 6, 12, 275-313.
- Kornilova L.N. The Role of Gravitation-Dependent Systems in Visual Tracking, Neuroscience and Behavior Physiology. 2004, 34, 8, 20-31.
- Kornilova L.N., Grigorova V., Bodo G. Vestibular function and sensory interaction in space flight. Journal of Vestibular Research. 1993, 3, 219-230.
- Kornilova LN., Temnikova VV., Dotsenko VI., Solovieva AD., Akarachkova ES. A computerized method for a complex assessment of vestibular function, intersensory interactions, and the eye pursuit function during treatment of vertigo with betaserc. Neurootol. Newsletter. 2008, Vol. 2, №1, 16-21.
- Kornilova LN., Temnikova VV., Naumov I.A., Solovieva AD. Therapy of patients complaining of vertigo and balance disorders. Journal of neurol. and psychiat. Named after SS Korsakov. (in Russian), 2009, № 10, 21-27.
- Kornilova LN., Temnikova VV., Naumov I.A., Ekimovskiy GA., Solovieva AD. Computer methods of therapy and rehabilitation of patients complaining of vertigo and balance disorders. News in otorhynolaryngol. (in Russian), 2010, № 6, 38-43.
- Kornilova LN., Temnikova VV., Naumov I.A., Ekimovskiy GA., Solovieva AD. Non-pharmacological management of vertigo and balance disorders with the help of hardware-software complex “OCULOSTIM”. Human Physiol. (in Russian), 2010, Vol. 36, № 6, 113-121.
- Kornilova L.N., Temnikova V.V., Naumov I.A., Solovieva A.D. Treatment of Patients with Vertigo and Balance Disorders. Neuroscience and Behavioral Physiology, 2011, № 41, 57-63.
- Kotimaki J, Sorri M, Aantaa E, Nuutinen J. Prevalence of Ménière disease in Finland. Laryngoscope 1999, 109:748-753.
- Kraft JR. Hyperinsulinemia. The differential marker of idiopathic neurootology with diagnostic/therapeutic application. Neurootol. Newsletter. 1996, Vol. 2, №2, 26-30.
- Kraus JV., MacArthur DL. Epidemiologic aspects of brain injury. Neurol. Clinics. 1996, 14, 435-450.
- Kressmann S., Muller WE., Blume HH. Pharmacological quality of different Ginkgo biloba brands. J. of Pharmacy & Pharmacol. 2002, 54, 661-669.
- Krylov YuV., Vorobiev OA., Zaritsky VV. About dissociation of vestibulovegetative and vestibulosensory reactions (in Russian). Kosm. Biol. Aviakosm. Med. 1985. – Vol. 19, № 3. 44-48.
- Kurshakov NA. Radiation disease (in Russian). Handbook of internal diseases. Moscow. Medgiz, 1963, 213-258.
- Kventon JF. Symptoms of vestibular disease. In: Neurotology Jackler RK & Brackman DE, (eds.), Mosby, St.Louis, Baltimore, Boston, 1994, 145-152.
- Lastkov D., Kolganov A., Mukhin V., Dudnik I., Soloviev A. Methodological approaches to assessing the impact of general vibration on coal miners. Proceedings of the 2nd International Workshop “Criteria for the evaluation of effects of whole-body vibration on man”. Moscow. ILO-WHO. 1992, 67-71.
- Lee-Chiong TL. Disorders of the circadian rhythm. In: Sleep medicine. Sateia M., Carskadon MA. (Eds.). Henley & Belfius, Inc., Medical Publishers. Philadelphia. 2002, 254-263.
- Lee CK., Yoo SK. ECG- based biofeedback chair for self-motion management at home. Consumer electronics. 2008, 1-2. ISBN: 978-1-4244-1458-1.
- Lempert T., Neuhauser H., Epidemiology of vertigo, migraine and vestibular migraine. J. Neurol. 2009, 256, 3, 333-338.
- LePage E. Occupational Noise-Induced Hearing Loss: Its Origin, Characterization and Prevention. Acoustics Australia, 1998, 26, 2, 57-61.
- Lipton R., Grosberg B., Singer RP., Pearlman SH., Sorrentino JV., Quiring JN., Saper JR. Efficacy and tolerability of a new powdered formulation of diclofenac potassium for oral solution for acute treatment of migraine: Results from the International Migraine Pain Assessment Clinical Trial. Cephalalgia, 2010, 30, 11, 1336-1345.
- Lukomskaya NY., Nikolskaya MI. Research of medications against kinetosis (in Russian). Nauka, Leningrad, 1971, 227 P.
- Lynn S., Pool A., Rose D., Brey R., Suman V. Randomized trial of the canalith repositioning procedure. OTOLARYNGOL HEAD NECK SURG 1995;113:712-20. http://dx.doi.org/10.1016/S0194-5998(95)70010-2
- Lysakowski A. Further observations on the regional organization of the chinchilla crista ampullaris. Equilibrium Research, Clinical Equilibriometry and Modern Treatment. Claussen C.-F., Haid C.-T., Hofferberth B (eds). Elsevier, Amsterdam, Lausanne, New York, 2000, 39-46.
- Mackert A., Kasper J., Thoden U. Responses to corneal stimulation in vestibulospinal units of nucleus Deiters. Exp. Neurol. 1984, Vol. 83, 24-32.
- Mallinson T. Myocardial infarction. Focus on first aid. 2010, 15, 15.
- Martin E., Perez N. Hearing loss after intratympanic gentamicin therapy for unilateral Ménière’s disease. Otol. Neurotol. 2003, 24, 800-806.
- Mast FW., Merfeld DM., Kosslin SM. Visual mental imagery during caloric vestibular stimulation. Neuropsychologia, 2006, 44, 1, 101-109.
- McMenomey SO., Gubbels SP. Labyrintitis. In: Vertigo and disequilibrium: a practical guide to diagnosis and management. Weber PC. (Ed.). Thieme. NY. 2007, 91-106.
- Mierzwinski J., Kazmierczak H. Vestibular habituation – the effect of cholinergic and adrenergic agents on the process. Neurootol. Newsletter. 1996, Vol. 2, №2, 68-72.
- Mierzwinski J, Trinus K, Kazmierczak H., Piziewicz A. The influence of vestibular habituation on polymodal evoked potentials. Neurootol. Newsletter, 2000. 5, 1, 50-55.
- Mikulas WL. Behavioral bibliotherapy and games for treating fear of the dark. Child & family behavior therapy, 1985, 7, 3, 1-7.
- Miller GT., Spoolman S. Sustaining the Earth: an integrated approach. Brooks/Cole, Centage Learning Inc., Belmont, 2009, 339.
- Moffat DA., Balagh RH. Ménière’s disease. In: Kerr AG., Booth JB. (eds.). Scott Brown’s Otolaryngology. Oxford. Butterworth-Heinemann. 1997, 3-d edition, 1-50.
- Moiseieva NI., Liubitsky RE. Action of heliophysical factors at human organism. In series: Problems of space biology (in Russian). Ugolev AM. (ed.). Leningrad, Nauka. 1986, Vol. 53, 136 p.
- Money K.E., Cheung B.S. Another function of the inner ear: facilitation of the emetic response to poisons. Aviat. Space Environ. Med. 1983, Vol. 54, № 3, 208-211.
- Mönning G. Klinik und Therapie von Herzrhythmusstörungen. Klinik der menschlichen Sinne. Stoll W. (ed.). Springer Wien NY., 2008, 191-198.
- Morita N., Kariya S., Deroee AF., Cureoglu S., Nomiya S., Nomiya R., Harada T., Paparella MM. Membranous Labyrinth Volumes in Normal Ears and Ménière Disease: A Three-Dimensional Reconstruction Study. Laryngoscope, 2009, 119, 11, 2216-2220.
- Moscicki EK, Elkins EF, Baum HM, McNamara PM. Hearing loss in the elderly: an epidemiologic study of the Framingham Heart Study Cohort. Ear and Hearing 1985, 6, 4, 184-90.
- Nashner LM., Black FO., Wall C III. Adaptation to altered support and visual conditions during stance: patients with vestibular deficits. J. Neurosci., 1982, 2, 536-544 p.
- Neuhauser H., Lempert T. Vestibular migraine. Neurol. Clin., 2009, 27, 2, 379-391.
- Neuhauser HK, Radtke A, von Brevern M, Lezius F, Feldmann M, Lempert T. Burden of dizziness and vertigo in the community. Arch Intern Med. 2008, 168, 19, 2118.
- Nikolenko VYu. Diseases of nervous system in miners and immune pathology (in Ukrainian). Donetsk. 1999, 266 P.
- Norré ME. Posture in otoneurology. Acta Oto-Rhino-Laryngologica Belgica. 1990, Vol. 44, №№2,3, pp. I-VI & 55-364.
- Norré ME., Degroote M. Influence of caloric and rotation testing upon bloodpressure and pulse rate. In: Vertigo, nausea, tinnitus and hypoacusia in metabolic disorders. Claussen C.-F., Kirtane MV., Schlitter K (eds.) Elsevier Science Publishers BV. 1988, 139-142.
- Novotný M., Cirek Z. Efficacy and tolerance of a combination preparation Arlevert®. Neurootol. Newsletter. 1996, Vol. 2, №2, 83-84.
- Novotný M., Kladenský J. Ménière’s disease and the urolithiasis. In: Vertigo, nausea, tinnitus and hypoacusia in metabolic disorders. Claussen C.-F., Kirtane MV., Schlitter K (eds.) Elsevier Science Publishers BV. 1988, 305-310.
- Nuwer M.R., Dawson E. Intraoperative evoked potential monitoring of the spinal cord: Enhanced stability of the cortical recordings. Electoencephalogr. Clin. Neurophysiol. 1984, Vol. 9, P. 318-327.
- Ödkvist LM., Noaksson L., Olsson S., Ledin T. Subjective Visual Horizontal Determination During Otolith Stimulation by Eccentric Rotation in Conservatively Treated Ménière’s Disease. Int. Tinnitus J. 1998, 4, 1, 75-77.
- Ojala M., Ketonen L., Palo J. The value of CT and very low field MRI in the etiological diagnosis of dizziness. Acta Neurol. Scand., 1988, 78, 26-29.
- Ojala M., Vaheri E., Larsen TA., Matikainen E., Juntunen J. Diagnostic value of electroencephalography and brainstem auditory evoked potentials in dizziness. Acta Neurol. Scand, 1988, 78, 518-523.
- O’Leary D.P., Vilches-Troya J., Dunn R.F., Campos-Munos A. Magnets in guitarfish vestibular receptors. Experientia 1981, Vol. 37, № 1, 86-87.
- Ollat H. Dopaminergic insufficiency reflecting cerebral ageing: value of dopaminergic agonist, piribedil. J. Neurol. 1992, 239, Suppl. 1, S13-S16.
- Olsson J.E. Rotational testing of the horizontal vestibulo-ocular reflex. In: Vestibular disorders. Barber H.O., Sharpe J.A (eds.). 1988, 97-116.
- Oman CM. Motion sickness: a synthesis and evaluation of the sensory conflict theory. Can. J. Physiol. Pharmacol., 1990, 68, 2, 294-303.
- Ornitz EM., Ritvo ER. The syndrome of autism: a critical review. Am J Psychiatry 1976; 133:609-621.
- Ozawa H., Ishikawa S., Mukuno K. Balance study of methyl mercury poisoning. Vestibular and visual control on posture and locomotor equilibrium: 7th Int. Symp. Int. Soc. Postulography, Igarashi M., Black F.O. (eds.). Karger, Basel, 1985, 302-308.
- Patil NP., Schneider D., Claussen C.-F., Popivanova C. Cardiac reactions in neurootological patients during vestibular stimulation. In: Vertigo, nausea, tinnitus and hypoacusia in metabolic disorders. Claussen C.-F., Kirtane MV., Schlitter K (eds.) Elsevier Science Publishers BV. 1988, 149-154.
- Pawankar R., Canonica GW., Holgate ST., Lockey RF. White Book on Allergy 2011-2012 Executive Summary. World Health Organization.
- Penfield W. Vestibular sensation and cerebral cortex. Ann. Otol. Rhinol. Laryngol., 1957, 66, 691-698.
- Peters TJ., Kotowicz J., Nyka W., Kozubski W., Kuznetsov V., Vanderbist F., De Niet S., Marcereuil D., Coffiner M. Treatment of alcoholic polyneuropathy with vitamin B complex: a randomized controlled trial. Alcohol and alcoholism. 2006, 41, 6, 636-642.
- Pfister M., Presbyakusis – genetische und umweltbedingte Risikofaktoren. In: Hören und Gleichgewicht. Im Blick des Gesellschaftlichen Wandels. 7. Hennig Symposium. Heidelberg. Springer Wien NY. 2010, 9-14.
- Phillips JS., Westerberg B. Intratympanic steroids for Ménière’s disease or syndrome. Cochrane Database of Systematic Reviews. 2011, Issue 7. Art. No.: CD.008514. DOI. 10/1002/14651858.CD.008514.pub.2.
- Platt C. The peripheral vestibular system of fishes. Fish Nerobiol Behav, Northcutt R.G., Davis R.E. (eds.). Ann Arbor: Univ. Michigan Press, 1981, 89-123.
- Plontke SK. Pharmakotherapie bei Hörstörungen – Gegenwärtiger Stantd und aktuelle Entwiklungen. In: Hören und Gleichgewicht. Im Blick des Gesellschaftlichen Wandels. 7. Hennig Symposium. Heidelberg. Springer Wien NY. 2010, 15-24.
- Plontke SK-R., Dietz K., Pfeffer C., Zenner H-P. The incidence of acoustic trauma due to New Year’s firecrackers. European Achives of Oto-Rhino-Laryngology. 2002, 259, 5, 247-252.
- Plosker GL., Gauthier S. Cerebrolysin. A review of its use in dementia. Drugs aging, 2009, 26, 11, 893-915.
- Polatajko HJ., Mandich A. Ergotherapy bei Kindern mit Koordinationsstoerungen – der CO-OPAnsatz. Thieme. Stuttgart, 2008, 147 P.
- Ponsford J., Olver J., Ponsford M., Nelms R. Long-term adjustment of families following traumatic brain injury where comprehensive rehabilitation has been provided. Brain. Inj. 2003, 17, 453-68.
- Pool SL., Nikogosian A. Results of medico-biological research at the experimental flights in the “Space Shuttle” project (in Russian). Kosm. Boil. Aviakosm. Med. 1984, Vol. 18, № 1. 45-57.
- Powell S.K. Case management. A practical guide to success in management care. Lippincott Williams & Wilkins, Baltimore. 2000, 527 p.
- Praetorius M. Gentherapie des Innenohres. In: Hören und Gleichgewicht. Im Blick des Gesellschaftlichen Wandels. 7. Hennig Symposium. Heidelberg. Springer Wien NY. 2010, 25-32.
- Pullens B., Giard JR., Verschuur HP., Benthem PP van. Surgery for Ménière’s disease. Cochrane Database of Systematic Reviews. 2011, Issue 1. Art. No.: CD005395. DOI: 10/1002/14651858. CD005395.pub.2.
- Pyykko I., Henriksson NG., Schalén L., Wenmo C., Novotny M. Velocity of saccades and of the fast phases of vestibular and optokinetic nystagmus. In: Differential diagnosis of vertigo. Claussen C.-F. (ed.). Walter de Gruyter & Co., Berlin, New York. 1980, 75-94.
- Rabinowitz PM. Hearing loss and personal music players BMJ 2010, 340, c1261.
- Reference book in dietology (in Russian). Pokrovsky AA., Samsonov MA. (eds.). Moscow, Medicine. 1981, 701 P.
- Reiss M. Derzeitiger Stand der medikamentösen Therapie von Schwindel. In: Der Gleichgewichtsinn. Neues aus Forschung und Klinik. 6 Hennig Symposium. Springer. Wien, New York. 2008, 149-158.
- Romberg H. Lehrbuch der Nervenkrankheiten. Springer-Verlag, Berlin, 1848, S. 184-191.
- Ropper AH., Brown RH. Adams and Victor’s Principles of Neurology (eighth Edition), NY, Chicago, San Francisco. 2005, 1398p.
- Rossi S. (ed.) Australian medicines handbook. Adelaide 2006. ISBN 0-9557919-2-3.
- Rossi G., Solero P., Cortesina M.F. Brainstem electric response audiometry: Value and significance of ‘latency’ and ‘amplitude’ in absolute sense and in relation to the auditory threshold. Acta Otolaryngol. Suppl. (Stockh). 1979, Vol. 364, P. 1-13.
- Rossini L., Izzo D., Summerer L. Braine-machine interfaces for space applications. In Engineering in medicine and biology society. 2009, 520-523.
- Rote Liste 2010. ECV Aulendorf. 2010, 576 Z.
- Roucoux-Hanus M., Boiusacq-Schepens N. Ascending vestibular projections: further results at cortical and thalamic levels in the cat. Exp. Brain Res., 1977, 29, 283-292.
- Rubin W. MRI use in otolaryngology. In: Vertigo, nausea, tinnitus and hearing loss in cardio-vascular diseases. Claussen C.-F., Kirtane M.V. (eds.) Elsevier Science Publishers BV. Excerpta Medica. Amsterdam-New York-Oxford, 1986, 517-519.
- Saha JC., Dikshit AK., Bandyopahyay M., Saha KC. A review of arsenic poisoning and its effects on human health. Critical reviews in environmental science and technology. 1999, Vol. 29, Issue 3, 281-313.
- Sakata E., Ohsu K. Diagnostic importance of spontaneous pathological eye movement. In (Ed.): Claussen C.-F., Haid C.T, Hofferberth B.: Equilibrium Research, Clinical Equilibriometry and Modern Treatment., Exerpta Medica, International Congress Series 1201, Elsevier Science B.V., Amsterdam, Netherland. 2000, 123-130.
- Salvinelli F., Trivelli M., Casale M., Firrisi L. Peco V.D., D’Ascanio L., Greco F., Miele A. Treatment of Benign Positional Vertigo in the Elderly: A Randomized Trial. The Laryngoscope. 2004, 114, 5, 827–831. DOI: 10.1097/00005537-200405000-00007
- Santos-Sacci J., Marovitz W.F. A ferritin-containing cell type in the stria vascularis of the mouse inner ear. Acta Otolaryngol. 1985, Vol. 100, № 1, 26-32.
- Savitz D. Leukaemia and occupational exposure to electromagnetic fields: review of epidemiological surveys / Savitz D., Calle E.E. – J. Occup. Med. 1987, 29, l, 47-51.
- Schaefer W.D. Okulaere Schwindel. Schwindel aus interdisziplinaerer Sicht, (Haid C.-T. editor). Georg Thieme Verlag. Stuttgart, New York, 2003, 108-115.
- Schneider D., Shulman A., Claussen C.-F., Just E., Schneider L., Koltchev Ch., Kersebaum M., Dehler R., Goldstein B., Claussen E. Recent findings about measurable interactions between tinnitus and vestibular disturbances. In (Ed.): Claussen C.-F., Haid C.T, Hofferberth B.: Equilibrium Research, Clinical Equilibriometry and Modern Treatment. Exerpta Medica, International Congress Series 1201, Elsevier Science B.V., Amsterdam, Netherland. 2000, p. 629 – 634.
- Schwartz PJ. The Long QT Syndrome. Futura Publishing Company, Inc., Armonk, NY. 1997, Vol.7, 427 p.
- Schwarze P. A parallel data processing in the vestibular system, does it exist? In: Vertigo, nausea, tinnitus and hearing loss in cardio-vascular diseases. Claussen C.-F., Kirtane M.V. (eds.) Excerpta Medica. Amsterdam-New York-Oxford, 1986, 235-238.
- Serdiuk AM., Bobyleva OA. Chornobyl and health of Ukraine. Materials of Scientific Conference: “Medical aspects of the accident at Chornobyl NPP” (In Russian). Кyiv, Zdorovia, 1998, 132 P.
- Shall MS. The importance of saccular function to motor development in children with hearing impairments. Int. J. Otolaryngol 2009, 972565.
- Sharma AK. Prevalence and correlates of susceptibility to motion sickness. Acta Genet Med Gemellol (Roma), 1997, 46, 2, 105-121.
- Silverstein H., Wanamaker HH., Rosenberg SI. Vestibular neurectomy. In: Neurootology. Jackler RK & Brackmann DE (Eds.). Mosby. St.Louis, Baltimore, Boston. 1994, 945-966.
- Silverstein H., Wazen J., Ess MJ van., Daugherty J., Alameda YA. Intratympanic gentamicin treatment of patients with Ménière’s disease with normal hearing. Otolaryngol Head Neck Surg. 2010, vol. 142 № 4, 570-575.
- Small M. Visual evoked potentials in a patient with prosopagnosia. Electroencephalography and Clinical Neurophysiology/Evoked Potentials Section. 1988, V. 71, Issue 1, 10-16.
- Smith PF, Zheng Y, Horii A, Darlington CL. Does vestibular damage cause cognitive dysfunction in humans? J Vestib Res. 2005, 15, 1, 1–9. PMID 15908735
- Snow V., Weiss K., Wall EM., Mottur-Pilson C. American Academy of family physicians; American College of Physicians – American Society of internal medicine. Pharmacologic management of acute attacks of migraine and prevention of migraine headache. Annals of internal medicine 2002, 137, 10, 840-849.
- Solomon S., Lipton RB. Criteria for diagnosis of migraine in clinical practice. Headache. 1991. 31, 6, 384-387.
- Sosin DM., Sniezek JE., Thurman DJ. Incidence of mild and moderate brain injury in the United States, 1991. Brain. Inj. 1996, 10, 47-54.
- Space biology and medicine (in Russian). Gazenko OG (ed.). Moscow, Nauka, 1987, 317 p.
- Speers M.A.Occupational exposures and brain cancer mortality. Speers M.A., Dobbins J.G., Miller V.S. American J. of Ind. Med. 1988, 13, 629-638.
- Stevens R.G. Electric power, pineal function and the risk of breast cancer. Stevens R.G., Davis S., Thomas D.B, Anderson L.E., Wilson B.W. FASEB. 1992, 6, 853-860.
- Stommel F.W., Stephens R.E., Alkon D.L. Motile statocyst cilia transmit rather than directly transduce mechanical stimuli. Cell. Biol. 1980, Vol. 87, 652-662.
- Strupp M., Brandt T. Vestibular neuritis. Semin. Neurol. 2009, 29, 5, 509-519. doi: 10.1055/s-0029-1241040. Epub 2009 Oct 15.
- Suvorov GA., Shkarinov LN., Denisov EI. Hygienic norming of industrial noises and vibrations (in Russian). Мoscow. Medicine. 1984, 240 P.
- Suzuki M., Yagi M., Brown JN., et al. Effect of transgenic GDNF expression on gentamicin-induced cochlear and vestibular ototoxicity. Gen. Ther. 2000, 7, 1046-1054.
- Szirmai A., Ribári O., Répássy G. Migraine related vestibular disorders in childhood and adolescents. Neurootol. Newsletter. 2002, Vol. 6, №2, 56-59.
- Tasaka K., Chung YH., Sawada K., Mio M. Excitatory effect of histamine on the arousal system and its inhibition by H1 blockers. Brain Res. Bull. 1989, Vol. 22, Issue 2, 271-275.
- Tham R., Bunnfors I., Eriksson B. Vestibulo-ocular disturbances in rats exposed to organic solvets. Acta Pharmacol. Toxicol. 1984, Vol. 54, 58-63.
- The Merk Manuel of Diagnosis and Therapy. Berkow R. (Ed.-in-Chief). – New York: Merk & Co. Inc. Rahway, 1992, 2844 p.
- Tibbling L., Hyden D. Vestibulo-vagal activity in the gastroesophagal region. Vertigo, nausea, tinnitus and hearing loss in cardio-vascular diseases. Claussen C.F., Kirtane M.V. (eds.). New York-Oxford-Amsterdam: Excerpta Medica, 1986, 201-205.
- Timmerman H. Pharmatherapy of vertigo: Any news to be expected? Acta Otolaryngol (Stockh). 1994, Suppl. 513, 28-32.
- Todd NPMcAgnus, Rosengren SM., Golebatch JG. Tuning and sensitivity of the human vestibular system to low frequency vibration. Neurosci. Letters, 2008, 444, 1, p. 36-41.
- Torchinski Yu.M. Serum in proteins. Moscow, Nauka. (in Russian). 1977. 302 P.
- Torok N. Significance of the Frequency in Caloric Nystagmus. Acta Otolaryng (Stockh.), 1948, 36, 38.
- Torok N. The Culmination Phenomenon and Frequency Pattern of Thermic Nystagmus. Acta Otolaryng. (Stockh.), 1957, 48, 530.
- Toupet M., Codognola S. Dictionnaire du vertige. – Paris: Lab. Janssen Ed., 1988. – 115 p.
- Trinus F.P. Pharmaco-Therapeutical reference book. Eighth edition (in Russian). Kyiv, Zdorovia, 1998, 880 p.
- Trinus K.F. About bioelectrical activity of human brain recorded in response to adequate vestibular stimulus. Physicians’ Affairs 1984. – №3. – P. 83-84 (In Russian).
- Trinus KF. Thresholds of long latency evoked potentials and movement sensations perceived during the linear acceleration action on human. Kosm. Biol. Aviakosm. Med (in Russian). 1986. – Vol. 20, № 6, 62-66. NASA Contractor Report 3922, №№ 13 & 23. USSR Space Life Sciences Digest, 1987 & 1988.
- Trinus K.F. Vestibular analyzer: criteria of its state evaluation. 2nd workshop on criteria for the evaluation of effects of whole-body vibration on man. Moscow, 1988, 92.
- Trinus K.F. Vestibular evoked potentials in response to angular acceleration. Abstracts of the twelfth midwinter meeting of the Association for research in Otolaryngology. – St. Petersburg Beach, Florida. Febr.5-9, 1989, 245-246.
- Trinus K.F. Action of the occupational hazards on the vestibular system. 20 Ann. Meeting Soc. for Neurosci. St.Levis, Missouri, 1990, 969.
- Trinus K.F. Chornobyl Vertigo: the comparison of the acute and chronic forms. Soc for Neurosci 22 Ann. Meeting. Anaheim, California, 1992, Vol. 18, part 2, 1048.
- Trinus K.F. Chornobyl vertigo, vestibulocardiac syndrome. Vertigo, nausea, tinnitus and hypoacusia due to central disequilibrium. Visual mechanisms in balance control. Proc. of the NES, Claussen C.F., Kirtane M.V., Schneider D. eds., 1994, Vol. 20, 121-126.
- Trinus K.F. Chornobyl vertigo: therapy. Vertigo, nausea, tinnitus and hearing loss in central and peripheral vestibular diseases. Claussen C.F., Sakata E., Itoh A. eds., Elsevier Sci. BV, 1995, 227-230.
- Trinus K.F. Chornobyl vertigo. 10 years of monitoring. Neurootology Newsletter, 1996, Suppl. 1, 140 p.
- Trinus K.F. Vestibular evoked potentials. Adv. Otolaryngol., Alford B.R., Jerger J., Jenkins H.A. (eds.): Electrophysiologic Evaluation in Otolaryngology. Basel, Karger, 1997, Vol. 53, 155-181.
- Trinus K. Chronic viral encephalitis, diagnostics with multisensory long latency evoked potentials. Neurootology Newsletter, 1999, Suppl. 2, 22-25.
- Trinus K. Multisensory evoked potentials (MEP) in differentiation of neurosis, encephalitis and epilepsy. Soc for Neurosci 29 Ann. Meeting. Miami Beach, 1999, Vol. 25, part 2, 1417.
- Trinus K. Evoked potentials recorded in response to magnetic stimulation. Przeglad Wojskowo-Medyczny, 2001, Suppl. 1, Vol. 43, 66.
- Trinus K. Vestibular potentials evoked by rotatory stimulus – parameters and data interpretation (in Polish). Biblioteczki Prospera Ménière´a. – Kwartalnik Rok, – Warszawa, 2003. – Vol.7. – P. 31-35.
- Trinus KF. Types of dizziness, evidence-based approach. ASN, 2010, 11p. http://neurootology.com
- Trinus K. Dizziness: etiology, pathogenesis, manifestations. 2010, 250 P. Internet edition http://books.google.com.ua/books?id=gd3tVHSaXbcC&lpg=PA43&ots=5-5cMMKTTS&dq=trinus%20dizziness&hl=en&pg=PA27#v=onepage&q&f=false
- Trinus K.F. Dizziness study test comparison. Archives of sensology and neurootology in science and practice ASN, 2011, Vol. 6. ISSN 1612 3352 http://neurootology.org
- Trinus K. Delayed neurological consequences of Chornobyl catastrophe (in Ukrainian). Materials of All-Ukrainian scientific practical conference with international participation «Actual problems of ambulatoric neurology» Kyiv, 18-19 May 2011, 149-163.
- Trinus KF. Migraine – vestibular disturbance: evidence-based approach (in Ukrainian). International Neurological J. 2011, №2, 40.
- Trinus K. Vestibular system: morpho-physiology and pathology. Lambert Academic Publishing. 2012, 544 p. ISBN 978-3-659-11350-5
- Trinus KF. Pathogenetic role of vestibular dysfunction in formation of arterial hypertension. Materials of All-Ukrainian scientific theoretical conference “Innovative technologies for prophylactic and management of arterial hypertension in ambulatory practice”, Kyїv, 20-30 November 2012, 96-101.
- Trinus K.F., Claussen C.-F. Guidelines on dizziness and space orientation disorders. Neurootology Newsletter, 2012, Vol. 9, № 1, 85p. ISSN 1023-6422 Author’s right Ukrainian Certificate #44450 from 25.06.2012
- Trinus KF., Claussen CF., Barasii SM. Vertigo and dizziness: differential diagnostics and individual treatment procedures. Neurootology Newsletter, 2008, Vol. 8, №2, 6-15.
- Trinus K.F., Claussen C.F., Schneider D., Demidenko N.V. Studies of vestibular disorders after Chornobyl – a specific vestibular syndrome. Neurootology Newsletter, 1995, Vol. 2, № 1, 46-53.
- Trinus KF., Kwasnitska OM. Human sensitivity to impulse magnetic fields (in Ukrainian). Ukrainian Med. Almanach. 2011, 14, 4 (Suppl.), 105-108.
- Trinus K.F., Oleinik V.I., Cherniuk V.I., Lastovchenko V.B., Meshcheriakov G.V., Nikolenko V.Y. Vestibular traumatic action of the different loadings. Vertigo, nausea, tinnitus and hypoacusia due to head and neck trauma. Claussen C.-F., Kirtane M.V. eds., Elsevier Science Publishers, 1991, 171-174.
- Trinus KF., Poskrypko YuA. Role of vestibular analyzer in the ergonomical support of flight safety. Sci.Recueill Kyiv. KIIGA, 1987, 92-97.
- Trinus K., Toupet M. L’Atteinte de la fonction vestibulaire chez les decontaminateurs de Tchernobyl. La Revue d’ONO, 1993, Vol. 19, Suppl. 1, № 20, 152-156.
- Uebelhack R., Gruenwald J., Graubaum H.-J., Busch R. Efficacy and tolerability of Hypericum extract STW 3-VI in patients with moderate depression: a double-blind, randomized, placebo-controlled clinical trial. Advances of Therapy. 2004, 21,4, 265-275.
- Uemura T., Suzuki J.-I., Hozawa J., Highstein S.M. Neurootological examination with special reference to equilibrium function tests. Tokyo, Igaku Shoin Ltd., 1977, 178 p.
- Unterberger S. Neue objektive registrierbare Vestibularis-körperdrehreaktionen, erhalten durch Treten auf der Stelle. Der Tretversuch. Arch.Ohr., – Nas.-,Kehlk.Heilk. 1938, 145, 273-282.
- Van der Laan FL. The ENG diagnosis of perilymph fistulae. Neurootol. Newsletter. 1999, Vol. 4, №1, 117-119.
- Vicini C., Ghilardi P.L. Dizziness and orthostatic hypotentsion: a clinical study. In: Vertigo, nausea, tinnitus and hearing loss in cardio-vascular diseases. Claussen C.-F., Kirtane M.V. (eds.) Elsevier Science Publishers BV. Excerpta Medica. Amsterdam-New York-Oxford, 1986, 87-94.
- Vorobiev OA., Migachev CD., Potkin AV. Effectivity of training activities use at visual, vestibular and motor systems to increase the resistance to kinetosis. Space Biol. & Aviaspace Med. Abstracts of IX All-Union Conference. Moscow-Kaluga, 1990, 36-38.
- Vrabel M. Is ondasetron more effective than granisetron for chemotherapy-induced nausea and vomiting? A review of comparative trials. Clin. J. Oncol. Nurs. 2007, 11, 6, 809-813.
- Waldfahrer F. Pharmacotherapie vestibulärer Erkrankungen. In: Hören und Gleichgewicht. Im Blick des Gesellschaftlichen Wandels. 7. Hennig Symposium. Heidelberg. Springer Wien NY. 2010, 103-113.
- Waldfahrer F., Iro H. Medikamentoese Therapie bei Schwindel. Schwindel aus interdisziplinaerer Sicht. Haid C.-T. (ed.). New York-Stuttgart: Georg Thieme Verlag, 2003, 206-216.
- Wang J., Ladrech S., Pujol R., et al. Caspase inhibitors, but not c-Jun NH2-terminal kinase inhibitor treatment, prevents cisplatin-induced hearing loss. Cancer Res.2004, 64, 9217-9224.
- Wertheimer N., Leeper E. Electric wiring configurations and childhood cancer. American Journal of Epidemiology. 1979, 109, 273-284.
- Westhofen M. Schwindel im Alter. In: Hören und Gleichgewicht. Im Blick des Gesellschaftlichen Wandels. 7. Hennig Symposium. Heidelberg. Springer Wien NY. 2010, 161-172.
- Wiltschko R., Wiltschko W. Pigeon homing: Effect of various wavelengths of light during displacement. Naturwissenschaften. 1998, 85, 164-167.
- Wladislavosky-Waserman P, Facer G, et al. Ménière’s disease: a 30-year epidemiologic and clinical study in Rochester, MN, 1951-1980. Laryngoscope 1984, 94, 1098-1102.
- Whitney SL, Rolf JG, Sparto BG. “Acrophobia and pathological height vertigo: indications for vestibular physical therapy?” Physical Therapy 2005, 85, 5: 443–458. ISSN 15842192. PMID 15842192.
- Wong GK., Zhu XL., Poon WS. Beneficial effect of cerebrolysin on moderate and severe head injury patients: result of cohort study. Acta Neurochir. Suppl. 2005, 95, 59-60.
- Zakharov VV., Yakhno NN. Syndromes of higher psychic functions disturbance. In: Diseases of nervous system (in Russian). Vol 1. Yakhno NN, Shtulman DR. (eds.) Moscow. Medicine. 2001, 170-190.
- Zhang C., Chopp M., Cui Y., Wang L., Zhang R., Zhang L., Lu M., Szalad A., Doppler E., Hitzl M., Zhang ZG. Cerebrolysin enhances neurogenesis in the ischemic brain and improves functional outcome after stroke. J. Neurosci. Res. 2010, 88, 3275-3281.
- Zozulia I.S., Golovchenko J.I., Onoprienko O.P. Stroke. (in Ukrainian) Svit uspikhu. Kyiv, 2010, 320 P.
- Zubkova OV. Investigation of long latency brain evoked potentials in response to rotatory stimulus in patients with light head trauma. Neurootol. Newsletter, 2008, Vol. 8, 2, 89-91.
- Boniver R. Temporomandibular joint dysfunction in whiplash injuries. Int. Tinnitus J. 2002, 8, 2, 129-131. http://www.scribd.com/doc/71429570
- Szirmai Á., Kisely M., Nagy G., Nedeczky Z.,. Szabados É.M., Tóth Á. Panic disorder in otoneurogical experience. International Tinnitus Journal, 2005, Vol 11, No I, 77-80.
- Szirmai Á. Anxiety in vestibular disorders. In Anxiety and related disorders. (Szirmai A. editor). Intech, Rijeka, 2011, ISBN 978-953-307-254-8, 191-210.
- Orliewska E., Mierzejewski P. Guidelines for conducting pharmacoeconomic evaluations. Farm. Econ. 2000, Suppl. 1
- Norwegian Medicines Control Authority. The Norwegian guidelines for pharmacoeconomical analysis in connection with application for reimbursement. Norwegian Medicines Control Authority Department of Pharmacoeconomics. Oslo, 1999.
- Riteco JA., de Heij IJM., van Luijn JCF. Dutch guidelines for pharmacoeconomic research. Amstelveen: College voor Zorgverzekeringen. 1999
- Panijel M. Die Behandlung mittelschwerer Angstzustände. Randomisierte Doppelblindstudie zum Klinischen Wirksamkeitvergleich eines Phytotherapeutikums mit Diasepam. Therapiewoche, 1985, 35, Heft 1, 4659-4668
- Alternative Medicine Review 7 (3): 240–3. 2002.
- Jacobson GP, Newman CW The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1990 Apr;116(4):424-7.