Junichi Matsushima and Aiko Matsushima
Sapporo, Japan
Abstract
Autophony and tinnitus accompanied by patulous Eustachian tube (PET) are annoying symptoms. The patients reported here were administered a treatment battery including drip of VB12 and with an autogenic treatment, this was effective for tinnitus relief by improving the blood circulation.
The objective of the study is to establish whether a little-invasive treatment battery as described above is effective for autophony and tinnitus caused by PET. A further object is to identify the factors that play a role in the efficacy of the treatment battery.
The study includes 105 ears in 92 patients (67 females, 25 males) with an average age of 63.1 years, treated from May 2011 to December 2015 for autophony and with positive signs of PET on the sonotubometry. The tinnitus in 78 (74%) of the 105 ears was treated and among these 70 (89%) experienced improvement.
The rate of relief in the tinnitus was similar in the PET related (n=47) and non-related (n=31) tinnitus. There was improvement in the autophony after the treatment in 97 of the 105 ears and among these 62 (59%) experienced complete relief, 35 (33%) experienced some relief, and 8 (8%) experienced no relief.
The duration of the Eustachian tube opening after the treatment (post-time) in the affected ears, 511.2msec (SD: 414.0) was statistically (p<0.0001) shorter, compared with that prior to the treatment (pre-time), 1563.8 msec (SD: 776.1). The middle ear pressure after treatment of the affected ears with negative pressure initially, -64.6daPa (SD: 66.5), was statistically (p<0.0199) improved, compared with that before treatment, -112.6 daPa (SD: 77.1). The presence of ear drum movement and the plateau pattern was positively correlated with the post-time in the affected ears following the treatment.
The treatment battery administered here was able to provide relief of autophony and tinnitus due to PET by improving the tubal function.
Key words: patulous Eustachian tube, autogenic training, Autophony, Tinnitus, duration for opening
Introduction
The Eustachian tube (ET) is a narrow canal that connects the middle ear to the back of the nose and upper throat. The Eustachian tube normally remains closed. In individuals with a patulous Eustachian tube (PET), the tube is abnormally open. Patients with PET experience a form of tinnitus that varies with breathing and autophony (abnormally loud audition of own voice. Autophony, tinnitus and ear fullness are annoying symptoms in patients with PET.
A combination of findings from sonotubometric tests, symptoms like autophony and breathing synchronized tinnitus, and ear drum movement may allow a definite diagnosis of PET (1, 2). Diagnostic criteria for PET using sonotubometry alone however are somewhat confusing and treatment is difficult. For severe PET surgical treatment is a possible treatment, while for less severe PET less invasive treatments can be expected to be effective. However, there are no treatments leading to a cure or little invasive treatments to normalize the tubal function.
A battery of treatments including intravenous drip infusion (IV drip) of VB12 and psychological therapies such as autogenic training, life style intervention, and counseling have been used to treat tinnitus at my clinic. The treatment was shown to improve the blood circulation with autogenic training and also promote rehydration.
The results for tinnitus caused by NVCS (neuro-vascular compression syndrome) have been submitted to the Journal of Otology & Neuro-otology (3). For the treatment of PET, rehydration and lying down are advocated for recovery of the venous tone of the pterygoid venous plexus in less severely affected patients.
The objective of this study is to determine whether a battery of psychological therapies, and including IV drip of VB12 is effective with autophony, tinnitus, and ear fullness based on the findings of sonotubometry. A further object is to investigate statistically what factors are affecting the improvement in the abnormal Eustachian tube function.
Methods
The study includes 105 ears in 92 patients (67 females, 25 males) with an average age of 63.1 years, treated from May 2011 to December 2015 for autophony and with positive signs of PET on the sonotubometry. All participants selected here complained of autophony. In addition to the presence of autophony, positive signs for PET include a duration of ET opening of more than 900 msec upon swallowing (2), that the shape of the sonotubometry shows a so-called “plateau pattern” (1), or that the sound pressure level of the test tone applied to the nostril was less than 105 dB.
Patients here had more than one of the 3 positive signs in the sonotubometry. The presence of ear drum movement was one of the symptoms for a definite diagnosis of PET. The JK-05A Eustachian tube function analyzer (RION, Japan) was used to for the diagnosis.
Figure 1 shows a typical finding of sonotubometry indicating PET. The so-called “plateau pattern” on the recording in the upper left panel disappeared just after the treatment (upper rt. panel). Opening durations of the ET were measured for statistical analysis.
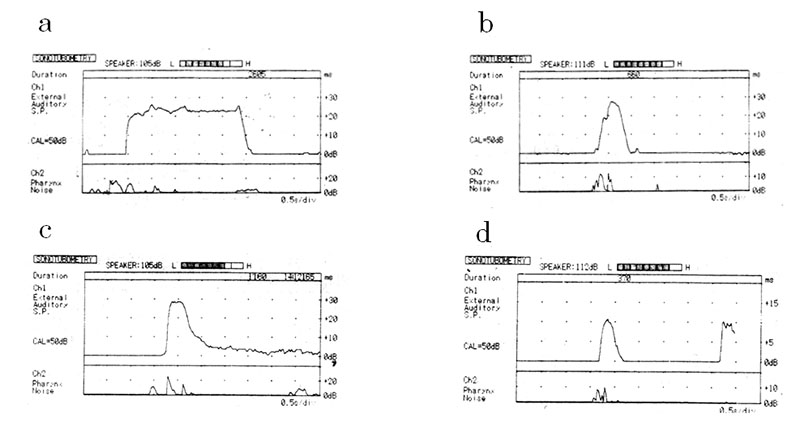
The top panels show recordings of an ear diagnosed with PET before treatment (a) and just after treatment (b). The bottom panels show recordings of the opposite ear unaffected by autophony before treatment (c) and just after treatment (d). The top left panel (a) represents the so-called “plateau pattern” in a recording which is typical to PET. The recording (b) in the top panel represents the nearly normal pattern following the treatment.
Patients were instructed to practice the autogenic training during intravenous drip infusion (IV drip) of VB12 for about one hour. At the weekly examinations a battery of sonotubometry, tympnogram, and audiometric tests were performed before and just after the treatment.
The participants were asked about changes in the symptoms like autophony, tinnitus, and ear fullness after treatment. Treatments were discontinued when positive effects on autophony were reported and/or patients requested treatment to be stopped at the interviews.
Then sonotubometry was undertaken to substantiate the efficacy of the treatment, treatment was generally undertaken once per week.
Statistics
The nonparametric Spearman’s rank correlation coefficient was used to assess the relationships of the various dependent variables. Comparison of the mean values was performed by ANOVA. A logistic regression analysis and the least squares method were used for goodness of fit for some variables. The outcomes of ear fullness, tinnitus, and autophony following treatment was assigned values as follows: relief as 2 points and absence of relief or no change 1 point, for the further study of the relationships.
The software used for the statistics was the JMP 10.0.2 developed by the SAS Institute Inc.
Results
The number of ears where the sound pressure level at the nostril was less than 105 dB, was 33. The number of ears, with a duration of ET opening upon swallowing of more than 900 msec, was 93. The number of the ears displaying the so-called “plateau pattern” on the recording of the sonotubometry was 36 and in 16 ears abnormal movement of ear drum was established.
Evaluations were undertaken when positive effects on autophony were reported. The treatments were then discontinued but continued once a week when patients requested continuation of the treatment at the interviews. The number of treatments administered and evaluated were after one treatment, 60 patients; after the second visit, 22; after three visits, 7; and after 4 treatments, 3. The overall average number of times evaluated was 1.5 times (standard deviation (SD): 0.8). “One treatment” means evaluation just after the first treatment and the 4 is the case of around 3weeks after the first treatment.
The least squares method for goodness of fit showed there was a positive relationship (p=0.0232) between treatment times and the disease duration from the onset of the disease till the first visit (43.8 days, SD: 65.4).
Table 1 shows the outcomes of the autophony, tinnitus, and ear fullness. There was improvement in the autophony in 97 (92.4%) of the 105 ears and among these 62 (59.1%) experienced complete relief, 35 (33.3%) experienced some relief, and 8 (7.6%) experienced no relief. For tinnitus, the outcomes were similar.
| Table 1 Diagnosis of affected ears vs. degree of relief in symptoms following treatment | |||||
| Degree of relief | Autophony | Tinnitus | Tinnitus based on origin | Ear fullness | |
| PET origin | Others | ||||
| Completely | 62 ears (59.1%) | 32 (41.0%) | 28 (87.5%) | 4(12.5) | 49 (47.1%) |
| Partly | 35 (33.3%) | 38 (48.7%) | 16 (42.1) | 22 (57.9) | 34 (32.7%) |
| Unchanged | 8 (7.6%) | 8 (10.2%) | 3 (37.5) | 5 (62.5) | 10 (9.6%) |
| n (ears) | 105 | 78 | 47 | 31 | 93 |
The tinnitus in 78 (74.3%) of the 105 ears were treated and among these 70 (89.7%) experienced improvement. No difference from the relief rate between PET related (n=47) and non-related (n=31) tinnitus was observed. There were ear fullness in 93 ears (89.5%) among 105 ears as reported to the first author. The ear fullness disappeared in 49 (47.1%) ears, was relieved in 34 (32.7%) ears and was unchanged in 10 (9.6%) ears.
The outcomes of autophony were positively correlated with the outcomes of tinnitus (γ=0.6331, p<0.0001) and the ear fullness (γ=0.7601, p<0.0001) using the nonparametric Spearman’s rank correlation coefficient.
There was also a positive relationship between outcomes of tinnitus and ear fullness, (γ=0.3986, p=0.0006). This shows that ear fullness and tinnitus were relieved when autophony improved. So relief of autophony was essential for treatment of PET.
The duration of opening of the ET after the treatment (post-time) in the affected ears, 511.2 msec (SD: 414.0), was significantly (p<0.0001) shorter, compared with that before treatment (pre-time), 1563.8 msec (SD: 776.1), as shown in Table 2.
| Table 2 Overall durations of opened Eustachian tubes and the pressures in the affected and unaffected ears | ||||||
| Parameters | Affected ears | Unaffected ears | ||||
| Pre-time | Post-time | n=105 | Pre-time | Post-time | n=79 | |
| Duration (msec) | 1563.8(776.1) | 511.2(414.0) | P<0.0001 | 689.4(515.5) | 407.2(342.4) | ns |
| Pre-pressure | Post-pressure | n=26 | Pre-pressure | Post-pressure | n=16 | |
| Pressure (daPa) | -112.6(77.1) | -64.6(66.5) | P<0.0199 | -34.1(62.7) | -14.8(29.2) | ns |
| ns: not significant. daPa: dalton pascal. | ||||||
The pre-time opening duration in the unaffected ears was significantly (p<0.0001) shorter than that of the pre-time in the affected ears. In the unaffected ears, the post-time opening duration, 407.2 msec (SD: 342.4) was not statistically shorter than that of the pre-time, 689.4 msec (SD: 515.5).
There was a positive correlation between the post-time in the affected ears vs. pre- and post-time durations in the unaffected ears, γ=0.347, p=0.0017 and γ=0.6821, p<0.0001 respectively. There also was a positive correlation between pre- and post-time values in the unaffected ears, γ=0.5426, p<0.0001. These findings suggest that the treatment improved the tubal function in the affected side and that the tubal functions in the affected ears would recover more when a rather good function in the opposite ears was maintained.
The treatment led to recovery in the negative pressure toward the normal level. Figure 2 presents a recording of a tympanogram. The peak of the negative pressure (-133 daPa) before treatment in the ear diagnosed with PET, as shown with a thin black line in the upper panel (a) recovered to the nearly normal level (-53 daPa) after one treatment, as shown with a thin black line in the lower panel (b).
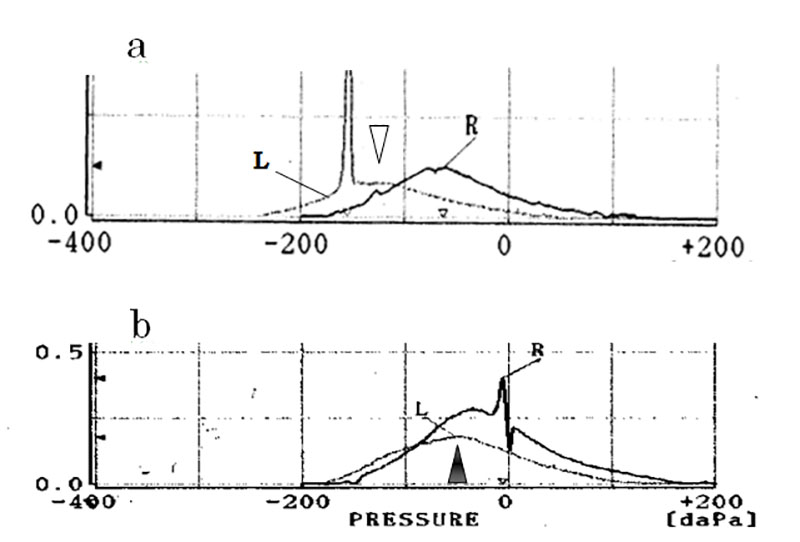
The top panel (a) shows a recording of the left ear (L) diagnosed with PET before treatment, as shown in a thin black line, and that of the unaffected right ear (R), as shown in the black line before treatment. The peak value of the affected middle ear (-133daPa) before treatment is represented at white triangle in the upper panel (a) recovered to the nearly normal value (-53daPa) just after one treatment shown at black triangle in the bottom panel (b).
There were 26 ears with negative pressure before treatment. The overall middle ear pressure after treatment of the affected ears with initial negative pressure (post-pressure), -64.6 daPa (SD: 66.5), was statistically (p<0.0199) improved over that before treatment (pre-pressure), -112.6 daPa (SD: 77.1), as shown in Table 2.
In the opposite ears, there was no significant difference between the pre- and post- pressures. These findings show that the middle ear pressure before the treatment of the affected ears with negative pressure initially, following treatment improved by the recovery of the tubal function. A positive relationship between pre- and post-pressures in the affected ears was also observed, γ=0.8051, p<0.0001.
Table 3 shows outcomes of autophony vs. opening duration of the tube and the middle ear pressure.
| Table 3 Outcomes of autophony vs. durations of opened Eustachian tubes and pressures in the affected and unaffected ears | ||||||||||
| Autophony | Affected ears | Unaffected ears | ||||||||
| Pre-time | P value | Post-time | n | P value | Pre-time | P value | Post-time | n | P value | |
| Relieved Unchanged |
1571.0(776.1) 1477.8(651.2) |
ns | 483.3.0(342.3) 850.0(893.3) |
97 8 |
0.0153 | 646.8(424.0) 1078.2(998.1) |
0.0237 | 385.2(343.0) 603.0(448.7) |
73 8 |
ns |
| Pre-pressure | Post-pressure | Pre-pressure | Post-pressure | |||||||
| Relieved Unchanged |
-113.5(78.6) -91.0(–) |
— | -63.2(67.4) -100(–) |
25 1 |
— | -35.7(64.5) -9(–) |
— | -15.9(29.9) 2.0(–) |
15 1 |
— |
| — : could not be calculated. ns: not significant. | ||||||||||
The post-time in the affected ears with relief of autophony, 483.3 msec (SD: 342.3, n=97), was statistically (p=0.0153) shorter than that without relief, 850.0msec (SD: 893.3, n=8), although the pre-time with relief in the affected ears was not different from that in ears without relief.
The pre-time with relief in the unaffected ears, 646.8msec (SD: 424.0, n=73), was statistically (p=0.0237) shorter than that without relief, 1078.2 msec (SD: 998.1, n=8) with no statistical difference in post-time in the unaffected ears with and without relief of autophony.
Comparing pre-time in the affected and unaffected ears, pre-time in the unaffected ears with relief of autophony was statistically shorter than that in the affected ears with relief of autophony (p<0.0001). However, there was no difference in the pre-time between the affected and unaffected ears without relief of autophony.
These findings suggest that the tubal function in the affected and unaffected ears with relief of autophony improved more than that of ears not experiencing relief. For the pre-time and post-time values, the outcomes for autophony was negatively correlated with the post-time in the affected ears (Odds ratio: 0.998, CI: 0.996-0.999, p=0.0247). These findings show that the recovery of the tubal function in the affected ears without relief were not sufficient to relieve autophony.
Table 3 shows that outcomes of autophony vs. the pressures in the affected ears and unaffected ears. The average post-pressures, -63.2 daPa (SD: 67.4, n=25) in the affected ears with relief of autophony was statistically higher (p=0.0021) than the pre-pressures in the affected ears with relief, -113.5 daPa (SD: 78.6, n=25) although statistics could not be performed in those of the pressures without of relief because of the small number this applied to.
The outcomes of autophony were negatively correlated with the pre-pressure (Odds ratio: 0.48651, p=0.0006) and positively with the post-pressure (Odds ratio: 3.09651, p=0.0091) in the affected ears. The relief of autophony was correlated with the middle pressure level before treatment and the changes in the pressure following treatment.
There were 34 ears which showed low tone hearing loss (HL), 16 with ear drum movement and 26 with the negative pressure. Among ears with negative pressure, low tone HL and ear drum movement, the least squares method showed a positive correlation between the ear drum movement and the post-time in the affected ears following treatment (p=0.0002).
Among ears with durations of more than 900msec, presence of the plateau, ear drum movement, and sound pressure level below 105 dB at the nostril, the least squares method showed that there were positive relationships between the post-time in the affected ears vs. the presence of the plateau pattern and ear drum movement, p=0.032, p=0.0089, respectively.
These findings suggest that the presence of ear drum movement and plateau pattern show severe PET and so the presence of these may disturb recovery of the tubal function.
Discussion
For diseases with symptoms of autophony other than PET there are several diseases such as superior canal dehiscence syndrome (SCDS) (4) and acute onset of sensorineural deafness. With SCDS, it may lead to an abnormally amplified bone conduction of sound into the inner ear.
Patients with SCDS typically hear not only their own voice but also their heartbeat, footsteps, chewing sounds, and more. In addition to audition, typical symptoms of SCDS include sound- or pressure-induced vertigo as well as disequilibrium. In the study reported here there were no vertigo patients who complained of sound- or pressure-induced vertigo. However, because of cost no CT tomography was performed to establish a differential diagnosis. Acute onset of sensorineural deafness especially conditions such as sudden deafness or low tone deafness could be causes of autophony.
But in such cases the patients typically hear not only their own voices but also the surrounding sounds or voices of other persons. Patients hearing the surrounding sounds loudly in addition to their own voice were excluded here.
Tinnitus caused by PET is characterized by breathing synchronized tinnitus and rustling sounds caused by the ear drum movement (1, 2). Therefore, treatment for the tinnitus of PET origin basically could be achieved by improvements in the Eustachian tubal function. This study showed that the post-time duration of opening in the affected ears in patients with tinnitus relief improved significantly (p=0.0183), compared with the pre-time duration. Improvements in the Eustachian tubal function caused relief of the autophony and ear fullness in addition to relief of tinnitus.
There were no differences in the rate of tinnitus relief of PET origin and tinnitus of other origins showed that the treatment administered here could relieve not only PET related tinnitus but also tinnitus of other origins. The treatment was used to relieve tinnitus, for example caused by NVCS by improving the blood circulation and relieving the congestion of the vessels (paper submitted to the Journal of Otology & Neuro-otology entitled “Results of Treatment of 523 patients for Tinnitus Which May Have Originated in Neurovascular Compression” (3). This agrees with the finding that there was relief of tinnitus of PET and other origins, and is as could be expected.
The diagnosis for PET is not straightforward. All patients here complained of autophony, and the diagnosis of PET here was made based on positive signs of sonotubometry and the finding of ear drum movement. Among the criteria described above in METHOD, presence of ear drum movement and the “plateau pattern” show severe PET and so the presence of these may disturb recovery of the tubal function. However, this study does not discuss PET criteria. The main object here is to consider improvements in autophony.
The treatment for PET is more difficult than just establishing the diagnosis. For severe PET there are reports of invasive procedures conducted through the tympanic inlet such as autologous cartilage injection, fat grafting, and silicon tubes (5). Surgical closure of the pharyngeal inlet is also a possible choice of treatment. For less invasive treatments there are procedures conducted through the pharyngeal inlet such as spraying or applying liniments and injection of collagen into the mucosa (5).
However, these treatments are not necessarily critical for recovery of the tubal dysfunction. Conditions that tend to be associated with PET include pregnancy (6), hormone therapy, fatigue, stress, and weight loss. These conditions can alter the physical characteristics of cartilaginous tubes and surrounding tissues (7-8). Possible etiologies of PET include atrophy of the peritubal fat tissue (9), loss of venous tone of the pterygoid venous plexus (10), and peritubal musculature dysfunction (11).
Conditions for a diagnosis of PET include temporary relief of autophony when lying down. This phenomenon may be induced by venous pooling of the pterygoid venous plexus, muscular swelling and edema in patients (10). For the mechanism of tinnitus from NVCS, in addition to anatomical causes of NVCS, there would be enlargement of the arteries due to blood flow congestion in the brain with the occurrence of NVCS (12).
A treatment battery including IV drip and psychological therapies was effective for relief of tinnitus arising from NVCS. Thinking about the mechanisms causing tinnitus from NVCS and the prompt response to treatment, the treatment improved the blood flow and then decreased or removed congestion around the ET, inducing the recovery of the pterygoid venous plexus tone, muscular swelling, and edema, leading to recovery of the tubal function. Less severe PET cases are advised to perform rehydration or to improve the blood circulation in the edema of tissue around the ET (13).
Limitations
One question here is why patients experience abnormally loud audio signals of the own voice. There were some patients with longer durations of ET who did not complain of autophony.
This raises the question whether it is possible to explain the mechanism of autophony as arising only based on the Eustachian tubal function or whether it would be possible to exclude the presence of other phenomena such as sensory affects, hyperacusis, and recruitment, which results from the elevated threshold of hearing and is governed by purely peripheral mechanisms caused by a loss of outer hair cells (OHCs) in the cochlea and the physical aspects, hydrops in patients with low tone HL (14) and ear drum movement (15)?
All patients selected here complained of autophony, so we were not able to compare data for patients with and without autophony.
The efficacy of the treatment reported here for autophony, tinnitus, and ear fullness was high. The treatment was little invasive, led to curing of the condition, and was highly effective. However, there is a psychological component in the therapy of the treatment, so the efficacy of this method depended strongly on the abilities of the administering physician.
Conclusion
In conclusion, to my knowledge this is the first study where results of tinnitus and autophony caused by PET is statistically analyzed.
This study shows that the tubal function in PET could recover by conservative therapy and it took only a few trials for most patients to experience the positive outcome.
When patients experiencing autophony with probable ET origin paid the first visit, the first step was to advocate a treatment aiming at rehydration and improving the blood circulation around the Eustachian tube.
Getting poor results from this after a few trials, a more invasive treatment should be advised for patients suffering distress due to this condition.
Abbreviations
PET, patulous Eustachian tube; ET: Eustachian tube; SD: standard deviation; daPa: dalton pascal; HL: hearing loss; IV intravenous; VB: vitamin B; SCDS: superior canal dehiscence syndrome; NVCS; neuro-vascular compression syndromes.
Competing interests
The authors declare that they have no competing interests to declare.
Refference
- Kikuchi T, Kobayashi T, Oshima T, Takata I, Oshima H, Ikeda R, Kawase T. High false-positive rate of the Sonotubometry in the diagnosis of the patulous Eustachian tube. 2013; Otol Jpn 23 (3):193- 197.
- Murakami D, Kimituki T, Komune S. Eustachian tube function tests (tubo-tympano-aerodynamic graphy and sonotubometry) in patients with pastulous Eustachian tube. 2011; Otol Jpn 21(3): 233-237.
- Matsushima J. Matsushima A. Results of treatment of 523 patients for Tinnitus which may have originated in Neurovascular Compression. Submitted to Otol Neurotol 2018.
- Chi FL, Ren DD, Dai CF. Variety of audiologic manifestations in patients with superior semicircular canal dehiscence. Otol Neurotol 2010; 3:2-10.
- Luu K, Remillard A, Fandino M, Saxby A, Westerberg BD: Treatment effectiveness for symptoms of patulous Eustachian tube: A systematic review. Otol Neurotol 2015; Dec; 36(10):1593-600. doi: 10.1097/MAO.0000000000000900.
- Graig SD. Pregnancy tube and nasal function during pregnancy: A prospective study. Otolaryngol Head Neck Surg 1988; 99: 6, 558-65.
- Sheer FJ, Swarts JD, Ghadiali SN. Three-dimensional finite element analysis of Eustachian tube function under normal and pathological conditions. Med Eng Phys Author manuscript; available in PMC 2013 Jun 1. Med Eng Phys 2012; Jun; 34(5): 605–616. Published online 2011; Oct 12. doi: 1016/j.medengphy.2011.09.008 PMCID: PMC3267871 NIHMSID: NIHMS328954 PMID: 21996354
- Yoshioka S, Naito K, Fujii N, Katada K. Movement of the Eustachian tube during sniffing in patients with patulous Eustachian tube: evaluation using a 320-row area detector CT scanner. Otol Neurotol 2013; Jul; 34(5):877-83. doi: 10.1097/MAO.0b013e31827d0963.
- Gabriela Pascoto G, Cassiana Abreu C, Silva ML, Weber R, Pignatari SS, Stamm The impact of acute loss of weight on Eustachian tube function. Int Arch Otorhinolaryngol 2014; Oct; 18(4): 376–379. Published online 2014; Jul 18. doi: 10.1055/s-0034-1382097. PMCID: PMC4296987PMID: 25992125.
- Oshima T, Ogura M, Kikuchi T, Hori Y, Mugikura S, Higano S, Takahashi S, Kawase T, Kobayashi T. Involvement of pterygoid venous plexus in patulous Eustachian tube symptoms. Acta Oto-Laryngologica. 2007; 127:7, 693-699. doi: 10.1080/00016480600987818.
- Casselbrant ML, Cantekin EI, Dirkmaat DC, Doyle WJ, Bluestone CD. Experimental paralysis of tensor veli palatini muscle. Acta Otolaryngol Sep-Oct; 106(3-4):178-85. 1988.
- Ohashi N, Yasumura S, Nakagawa H, Mizukoshi K, Kuze S: Vascular cross-compression of the VIIth and VIIIth cranial nerves. J Laryngol Otology 106: 5; 436-9. 1992.
- Smith ME, Scoffings DJ, Tysome JR. Imaging of the Eustachian tube and its function: a systematic review. Neuroradiology 2016; 58: 543–556. Published online 2016 Feb 27. doi: 10.1007/s00234-016-1663-4. PMCID: PMC4877436. PMID: 26922743.
- Ogi K, Manabe Y, Yamada T, Takabayashi T, kimura Y, Narita N, Fujieda S. Meniere’s disease with patulous Eustachian tube. J Neuro Neuroscience Vol. 2015; 6 (3): 28. doi: 10.21767/2171-6625.100028
- Boedts M: Paper patching of the tympanic membrane as asymptomatic treatment for patulous Eustachian tube syndrome. J Laryngol Otol 2014; 28, 228–235. doi:10.1017/S0022215114000036