András Molnár, Stefani Maihoub MD, Prof. László Tamás, Ágnes Szirmai MD, PhD
Budapest, Hungary
Introduction
Ménière’s disease (MD) is a disorder of the inner ear, characterized by episodic rotational vertigo, sensorineural hearing loss, tinnitus, aural pressure and vegetative symptoms, such as nausea and vomiting. [1] The morphologic entity of the disease is the inner ear’s endolymphatic hydrops.
The cause of MD is thought to be multifactorial (anatomic and genetic contributions, allergy, viral infection etc.), however, the exact aetiology is still unknown. [2] It’s difficult to appreciate the true prevalence of MD, the literature reports about a prevalence of around 30-50/100 000, depending on the geographical location. [3]
So, the disorder is not expressly frequent, but the importance of the topic stems from the influence of the symptoms over the patients’ quality of life. The disease seems to be incurable, so the symptomatic, conservative pharmacologic treatment is an important question. The present study was undertaken to find out that how we could assure these patients’ symptomatic control. The study was carried out in the Department of Otolaryngology, Head-and Neck Surgery, Semmelweis University, Hungary.
The betahistine-dihydrochloride is widely used in Europe as a first line treatment in the symptomatic control for MD, however it’s not wide-spread in the USA. [4] Betahistine is a histamine-like drug that acts as both a partial histamine H1 receptor agonist and a histamine H3 receptor antagonist. [5] It’s assumed that the efficacy of betahistine results from vascular effects, inducing increase in blood flow of the inner ear, shown for example in guinea pig. [6]
However, betahistine was also found to be effective in vestibular syndromes not related to the inner ear’s vascular insufficiency, so other effects on the central vestibular system have been also suspected. In a study it was certified that histamine analogues increase the synthesis of the histamine, mostly through the blockade of the H3 autoreceptors. [7]
The side effects of the agent are slight, headache, nausea and gastrointestinal symptoms, such as distension and indigestion were described. In case of pregnancy (not enough clinical data is available) and allergy it’s not applicable, and some generics contain lactose, so these are not recommended in lactose intolerance. In Hungary betahistine could be prescribed with raised indication for patients in Ménière’s syndrome. [8]
During the IFOS Congress in 2017 a minimal consensus attained and was summarized in an algorithm (Figure 1.). [9]
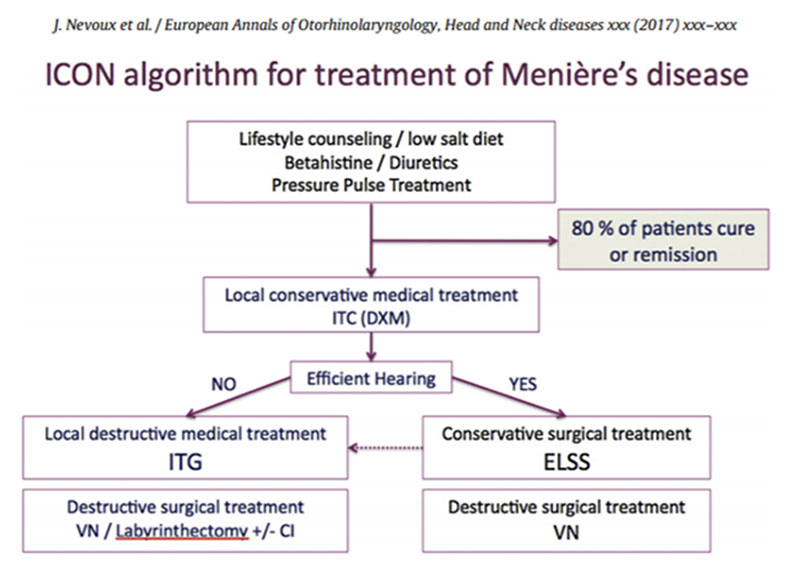
As shown in Figure 1. the first line of treatment is lifestyle counselling, diuretics and betahistine. However, several clinical studies have shown significant improvement of the disorder’s symptoms, a consensus has yet to be made considering the effectiveness and advantages of it. [10]
The possible effect of the nootropics is complex: vasodilator effects, influence on the blood’s reologic quality, exert influence over the blood cells. [11] The application of these agents is rather empirical than evidenced based, but the treatment seems to be effective. [10] Previously it was found that dual therapy is more effective in the treatment of peripheral vestibular disorders than the betahistine monotherapy. [12]
Aims of the study
The aim of our study is to evaluate how we could provide periods without complaints at the tertiary referral otoneurologic centre of our clinic. According to our assumption the different pharmacologic agents of the conservative treatment result in significant improvement in the symptomatic condition of the patients with MD.
We wanted to ensure the potential role and efficiency of the betahistine in the control of the vertigo attacks, and to confirm or disprove the advantages of the dual therapy (betahistine plus nootropics) over the betahistine monotherapy. We would like to prove the effectiveness of the intratympanic applicated steroids in the conservative medication of the progression of the sensorineural hearing loss as well.
Materials and methods
To verify the truth of our supposition 105 (31 men and 74 women, mean±SD age, 57.4±11.05) patients with definite Ménière’s disease according to the diagnostic scale of the American Academy of Otolaryngology-Head and Neck Surgery were enrolled in this retrospective study. Beside the analysis of the hospital records the subjective complaints of the patients and the completed dizziness diaries were taken into consideration too. The typical following time of the subjects were 47.6 months±33.8, meanwhile 5 controls became due on average.
Results
Epidemiological surveys in Hungary
The mean age of the patients was identified as 57.38 years±11.07 SD, and as shown in Figure 2.
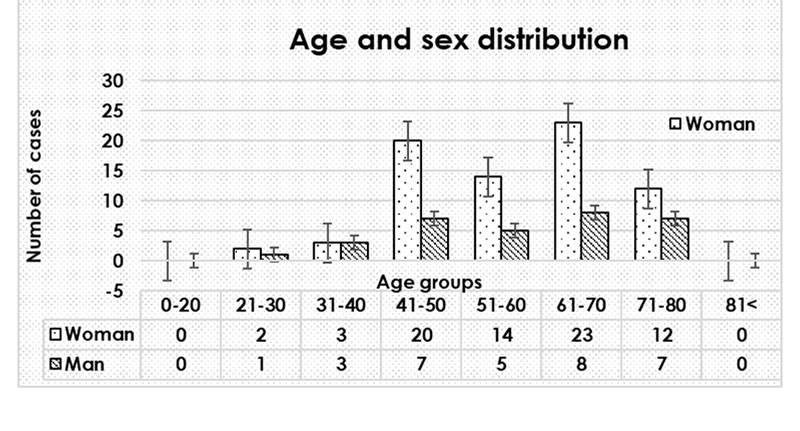
The age distribution at onset in MD peaked for both of the males and females in the middle- aged groups. Patients consisting of 31 (29.5 %) males and of 74 (70.5%) females, so it follows that a strong preponderance of females is presented in MD, such as in the other peripheral vestibular disorders. [13] In this examined population most of the patients suffering from MD were ranked among the age group of 61 to 70, however, the frequency of which rises from the middle ages unequivocally.
In summary we could find that MD is most frequent in the middle-aged groups, which is important because this interval takes in the most active years from the point of view of economic standpoints. Due to the symptoms it’s often necessary to place the MD patients on the sick list.
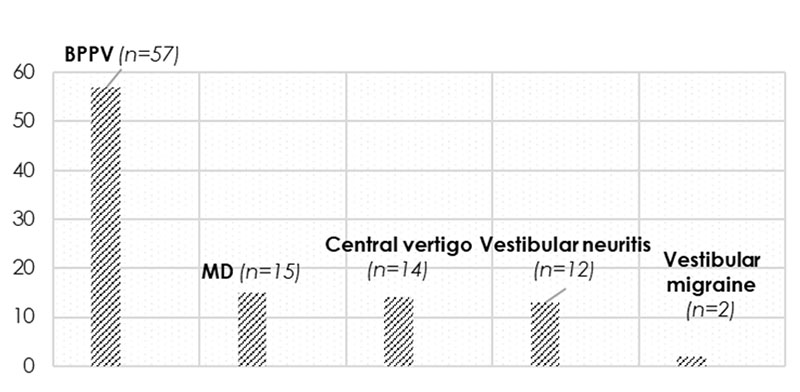
By virtue of our population by far the most common peripheral vertigo is the BPPV (benign paroxysmal positional vertigo), which has been estimated in several population-based studies [14] and Ménière’s disease seems to be the second most frequent (Figure 3).
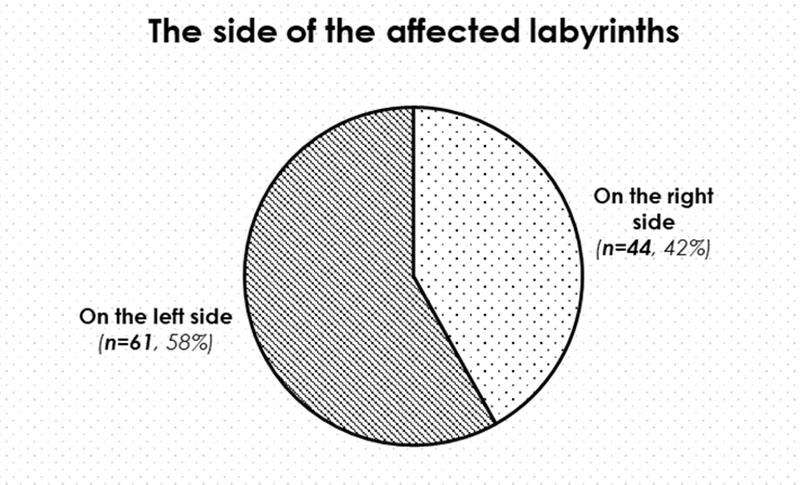
We also examined which side of the labyrinths were affected in the EH. We found that MD was more frequent on the left side in the analysed population than on the right side (Figure 4) and no bilateral MD could be found.
The monitoring of the subjective symptoms on the strength of the vertigo diaries
As shown in Figure 5. by completing the vertigo diaries our patients can take account of the symptoms’ characteristic. In cases of the vertigo attacks the duration of the episodes is specifically important: we can talk about MD attack only if the vertigo is described as rotary and if it’s duration lasts at least 20 minutes long (according to the AAO-HNS criteria).
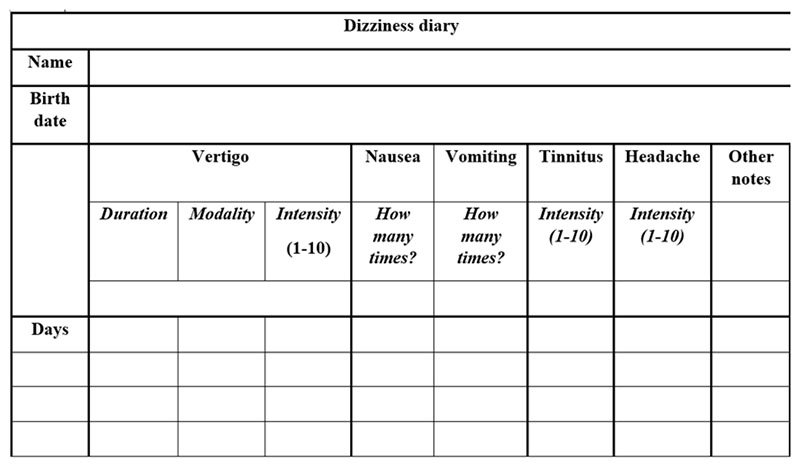
The typical characteristics of the symptoms were determined using the 125 completed diaries, collected from our MD patients:
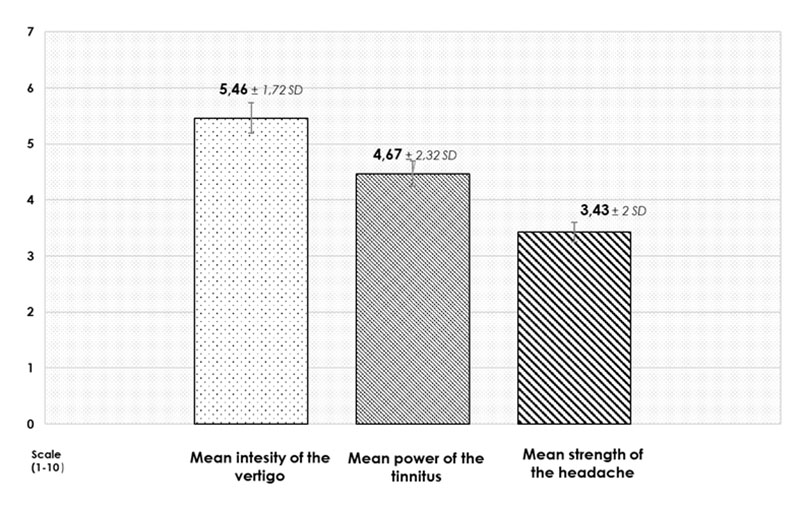
According to the diaries, our patients reported about 1552 episodes of dizziness and 52.7% of these episodes seemed to be described as rotational vertigo (Figure 7), the frequency of which was 2.35±1.4 attacks pro month on average.
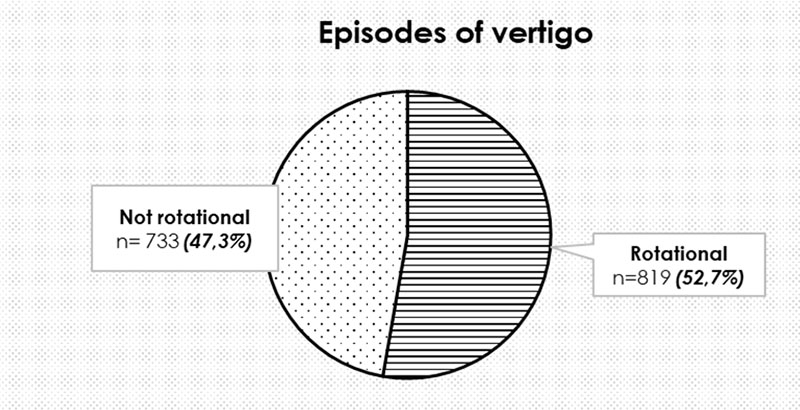
The intermittent attacks of vertigo lasted 6.16 hours and their strength was around 5.46±1.7 on a scale of one to ten. The mean value of the intensity of the tinnitus appeared to be 4.46±2.3 on a scale of ten and headache was associated with the episodes in 82% of the cases (Figure 6 and 7). The associated vegetative symptoms are important too: nausea appeared in 98.1%, while vomiting in 89.5% of the cases.
The vertigo diaries are helpful in the analysis of the patients’ subjective symptoms: we can make sure that the characteristics of the attacks meet the requirement of the criteria and by using the diaries the following of the effectiveness of the pharmacologic treatment is easier as well.
Analysis of the conservative treatment’s possibilities
After working up of the data the following results appeared according to the statistical analysis.
- Under the betahistine treatment the vertigo attacks seemed to appear rarely than among those patients not treated (allergy, pregnancy or arbitrary reducing of the medicine’s dosage). The mean dose in the symptomatic treatment seemed to be 87.5±27.2 mg pro day, however, no apparent connection was found between the dose of the agent and the symptomatic control, so it’s important to set up the dosage for every patient individually.
- We wanted to confirm or disprove the advantages of the dual therapy (betahistine plus nootropics) over the betahistine monotherapy. According to our results in case of dual therapy the vertigo episodes appeared significantly less often in comparison with those treated by betahistine only.
- Intratympanic steroid therapy is the first line treatments of the hearing loss [15], and also of the sensorineural hearing loss in MD. [16] Our results are the following:
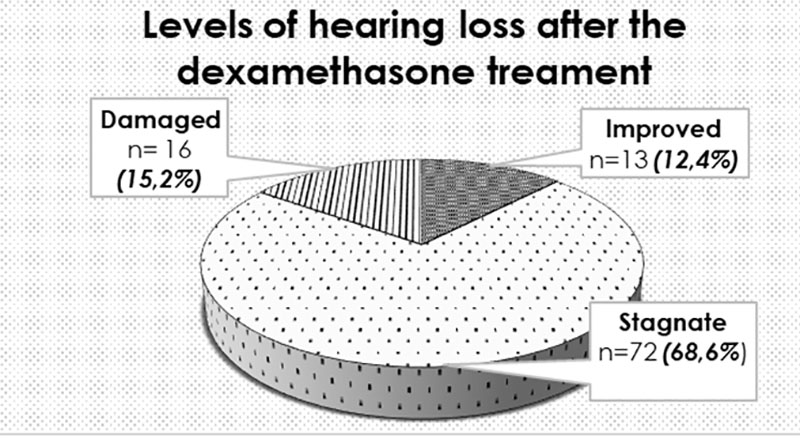
In most of the cases (68.6%) after the intratympanic dexamethasone treatment stagnation in the hearing profile seemed to be achieved, but all patients from the “improved” group were treated with intratympanic dexamethasone, while improvement without steroid treatment could never be attained.
Conclusions
According to the dizziness diaries the most tormenting symptoms are the vertigo attacks, so the symptomatic treatment of these episodes seems to be prominent. The second most determining symptom is the tinnitus, so it’s important to talk about that too.
Betahistine, the agent widely used in Europe as a first line treatment for MD seemed to be successful in the conservative treatment of the symptoms according to our observations.
However, in case of dual therapy (betahistine and nootropics) the vertigo episodes appeared significantly less often in comparison with those treated by betahistine only. In the conservative treatment of the sensorineural hearing loss it was successful to confirm the efficiency of the intratympanic administered steroid injections.
References
- J. Harcourt, K. Barraclough, A. M. Bronstein, Meniere’s disease. British Medical Journal. 2014:349:g6544.
- Saumil N. M., Joe C.A., Joseph B. N., Pathophysiology of Ménière’s syndrome: are symptoms caused by endolymphatic hydrops? Otology and Neurootology. 2005;26:74-81.
- Ménière’s disease: overview, epidemiology, and natural history. Otolaryngologic Clinics of North America. 2002; 35(3): 455-95.
- Jeffrey D. S., Carolina T., Michael C. S., John P. C., Treatment of Ménière’s Disease. Current Treatment Options in Neurology. 2015. 17:14.
- Timmerman, H., Histamine agonists and antagonists. Acta Oto-Laryngol., Suppl. 1991. 479, 5–11.
- Laurikainen, E., Miller, J. M., Nuttall, A. L., Quirk, W. S., The vascular mechanism of action of betahistine in the inner ear of the guinea pig. Eur. Arch. Otorhinolaryngol. 1998. 255, 119–123.
- Brahim T., Suzanne T., Christiane M., Carole C., Michel L., Betahistine dihydrochloride interaction with the histaminergic system in the cat: neurochemical and molecular mechanisms. European Journal of Pharmacology. 2002. 446, 63-73.
- Szirmai Ágnes: Differentialdiagnosis and therapy of balance disorders. (Szirmai Á., Az egyensúlyzavarok differenciáldiagnosztikája és terápiája. Semmelweis, 2006. Hungarian). Semmelweis Kiadó, Budapest, 2006. ISBN 9639656 03 8.
- Nevoux, M. Barbara, J. Dornhoffer, W. Gibson, T. Kitahara, V. Darrouzet, International consensus (ICON) on treatment of Ménière’s Disease. European Annals of Otorhinolarnygology, Head and Neck diseases. 2017.
- Shakeel R. S., Diagnosis and treatment of Ménière’s disease. British Medical Journal, 1998.
- Gyires Klára, Fürst Zsuzsanna, Ferdinandy Péter, Pharmacology and Clinical Pharmacology (Farmakológia és Klinikai Farmakológia. Hungarian), Medicina Kiadó, Budapest, 2017.
- O. A. Melnikov, S. V. Lilenko, J. Nauta, M. J. N. M. Ouwens, Betahistine plus piracetam dual therapy versus betahistine monotherapy for peripheral vestibular vertigo: a confounder-corrected subanalysis of the OSVaLD study. Current Medical Research and Opinion. 2015; 1951-1962.
- Neuhauser H.K., von Brevern M., et al., Epidemiology of vestibular vertigo: A neurotologic survey of the general population. Neurology. 2005;65(6);898–904.
- von Brevern M., Radtke A., et al., Epidemiology of benign paroxysmal positional vertigo: A population-based study. Journal of Neurology, Neurosurgery and Psychiatry. 2007;78(7):710–715.
- Robert J. S., Sujana S.C., Sanford M. A., et al., Clinical Practice Guideline: Sudden Hearing Loss. Otolaryngology-Head and Neck Surgery, 2012.
- Faramarz M., Fatemeh H., Effect of Intratympanic Dexamethasone on Controlling Tinnitus and Hearing loss in Meniere’s Disease. Iranian Journal of Otorhinolaryngology. 2014; 26(76): 129–133.