This article is a small part of the volunteer project for help to the victims of Russian aggression in Ukraine.
Your input should be greatly appreciated.
Vestibular disturbances after blast injury (mild traumatic brain injury mTBI)
Definition
Blast injury is a complex type of physical trauma resulting from direct or indirect exposure to an explosion. Blast injuries occur with the detonation of high-order explosives as well as the deflagration of low order explosives. These injuries are compounded when the explosion occurs in a confined space [10].
Scope of the problem
During last century blast injury is crucially increasing [5]. Primary blast injuries result from the over-pressurization wave and typically affect gas-filled body structures (eg, lungs, gastrointestinal tract, middle ear) resulting in injuries such as blast lung, tympanic membrane rupture, abdominal hemorrhage, and concussion [3].
Researchers and clinicians have estimated that approximately 300000, about 20%, from 1.6 of the million deployed to Iraq and Afghanistan have experienced mild traumatic brain injuries (mTBI) [7].
In the response of Mr. I.V. Maltsev, Head of Clean-up Commision of the State Department of Ukraine on War Veterans’ and Antiterroristic Operation (ATO) Participants’ Affairs №2493/02/04.2_19 from 03.07.19 to Mrs. Nadia Potapova it has been indicatied that in General Rgister of ATO participants by 01.07.19 there were 369 451 persons recorded. It means that among them there are at least 74000 patients with blast trauma. And besides up to six millions if civils living at that time at the territiry of Luhansk and Donetsk regions have been ignored, among which 1200000 persons with blast injury. This does not consider Ukrainian Millitary volunteers and Majdan participants, the latter might mean about 1.5 million of victims or up to 4% of the population of Ukraine.
The data about vestibulat disorders resulting from blast injury are contradictory. Among ear outcomes some authors pay attention at subjective hearing loss (57.14% examined), tinnitus (80.36%), ear fullness (80.36%), hyperacousia (32.14%) and vertigo (3.57%) [6].
In the Report of the Department of Veterans Affairs (USA) 2016 February N. Greer and coauthors have recognized that information about true prevalence of blast trauma among deployed millitary personal of USA and its consequences is limited in the literature. Hearing loss has been recognized to be clinically significant while vestibular effects were “unremarkable”. [5].
This seems to be rather equivocal because vestibular analizer is just the movement sensor and it has to produce the most signficant reaction. The possible explanation might be in the period of imagionable wellbeing, when vestibular damage has no clinical manifestations [11].
From the other side about 20% patients have complained of dizziness/vertigo from moderate to middle expression. Most of the patients have complained of tinnitus high frequency by nature. Remarcable that frequently this patients were complaining of tinnitus without objective hearing loss [14]. Other authors presented from 15% to 40% of patients complaining of dizziness, vertigo of diplopia [9]. At last, some researchers consider dizziness, vertigo instability, postural deficit and space orientation to be the most frequent symptoms of blast injury [1].
Among limited reports dedicated to vestibular consequences of blast injury posturographic and optokinetic investigations have dominated [8], while data of rotatory tests we have not find. But, just movement test might provide information about the dysfunction level of vestibular nuclei and their condition, excitation or inhibition.
To disclose the problem of vestibular disorder resulting as the consequence of blast injury we have done this investigation.
Material
164 persons have been examined. Among them 161 patient has passed the Questionnaire “Types of Dizziness”, among which non-ATO (AntiTerroristic Operation against Russian aggression in Ukraine, all survived mild Blast Brain Traumatic Injury) with the diagnosis acute hearing decrease – 18 patients, ATO participants 20 pesons (7 in acute phase, one week after contusion, 13 – chronical, mostly being exposed to explosions in 2014-2015), patients with chronical delayed vestibular dysfunctions complaining of dizziness/vertigo non-ATO (n=123). 41 persons have passed pendular test, among which АТО – 24, 7 in acute phase (1 week after trauma), 17 – in chronic, female – 4, male – 37, 17 patients with neurosensory hearing decrease, results of one patient are lost because of computer failure.
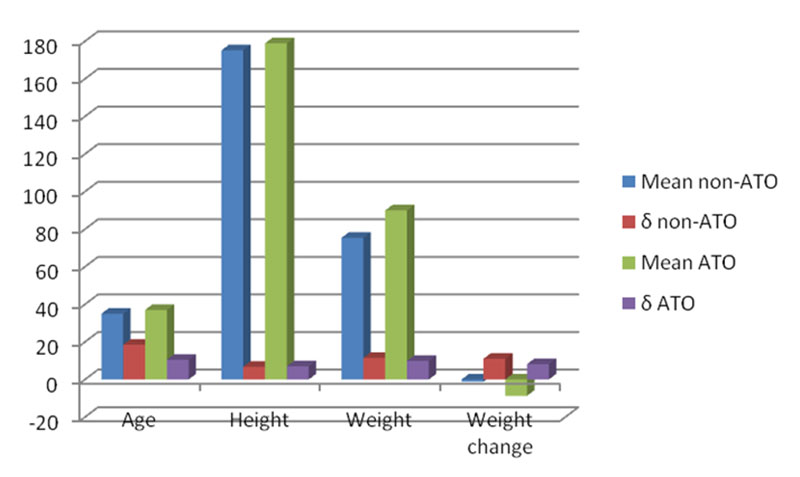
Age, height, weight are depicted at Fig. 1. Weight changes according to F-test 0.497 and Т-test 0.2365 were not significant, the same to other parameters, so the groups were well matched.
Methods
To standardize the complaints the Questionnaire “Types of Dizziness” has been used according to “International Clinical Protocol on Vestibular Disorders (Dizziness)” [12].
Documentation of the vestibular function was made with the pendular test performed at rotatory chair produced by Interacoustics, Denmark. We have investigated gain, phase shift and symmetry. Gain – ratio of SPV to chair velocity (American system); ratio of nystagmus frequency to chair motion frequency (European system), normative data – 0.15-0.95. Asymmetry of gain is gain ratio of right to left eye movements in %.
The normative data for these parameters are considered to be the next (age 15-55 y.o.). Gain: at frequencies 0.01 Hz – 0.25-0.49; 0.02 Hz – 0.37-0.65; 0.04 Hz – 0.44-0.59; 0.08 Hz – 0.49-0.65; 0.16 Hz – 0.50-0.71; 0.32 Hz – 0.50-0.85; 0.64 Hz – 0.50-0.92. Gain asymmetry – normative data do not exceed 14.76%.
Phase shift – difference between phase angles of eye and chair positions (for healthy at frequencies 0.01 Hz – 16.72-58.62; 0.02 Hz – 6.16-33.97; 0.04 Hz – 2.64-22.53; 0.08 Hz – (-3.69)-(+13.02); 0.16 Hz – (-9.51)-(+12.32); 0.32 Hz – (-14.78)-(+8.45); 0.64 Hz – (-14.96)-(+2.64) [4]. Spectral purity means ratio of frequencies filling between input and output, 95% means normative range, many investigators use 60% as borderline.
Results
Questionnaire “Types of Dizziness”
The complaints structure among ATO and non-ATO participants according to Questionnaire “Types of Dizziness” is reproduced at Fig. 2.
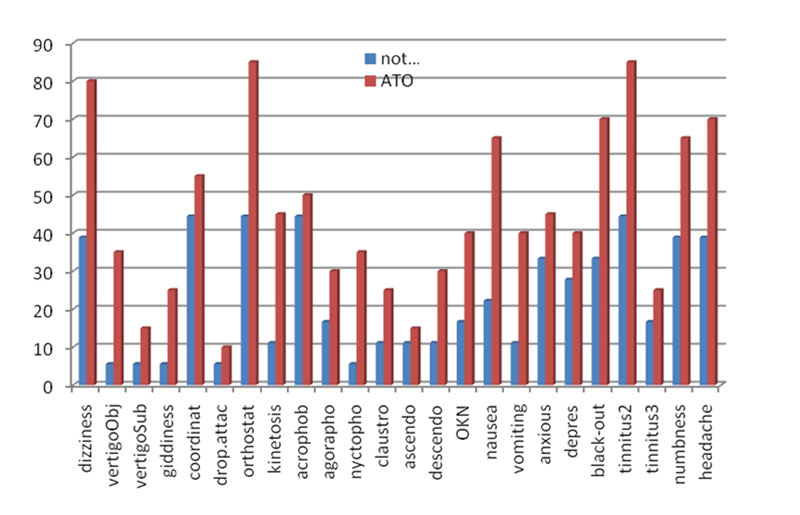
The attention was paid at differencies of 20% (significant difference) and 37% (very significant difference). It could be seen that among ATO participants very significant appeared to be complaints of dizziness, ortostatics, nausea, black-outs and II type of tinnitus. Significant being complaints of kinetoses, nyctophobia, optokineses, vomiting spells, numbness and headaches.
Comparizon of the complaint profiles for patients with delayed chronic vestibular disorder (first figure), patients with acute neurosensory hearing decrease (second figure), ATO paticipants (third figure) is presented (in brackets % of difference, 20% is significant in bold).
dizziness – 58.92%; 39.89; 80.00 (21.08)
objective vertigo – 23.26%; 5.56; 35.00 (11.74)
subjective vertigo – 17.05%; 5.56; 15.00
giddiness – 27.13%; 5.56; 25.00
imbalance – 57.36%; 44.44; 55.00
ortostatics – 54.26%; 5.56; 10.00
kinetosis – 30.23%; 11.11; 45.00 (14.77)
acrophobia – 50.39%; 44.44; 50.00
agoraphobia – 51.94%; 16.67; 30.00
nyctophobia – 27.91%; 5.56; 35.00 (7.09)
claustrophobia – 21.71%; 11.11; 25.00 (3.29)
ascendophobia – 14.73%; 11.11; 15.00
descendophobia – 20.16%; 11.11; 30.00 (9.84)
optokinesis – 20.93%; 16.67; 40.00 (19.07)
nausea – 41.86%; 22.22; 65.00 (23.14)
vomiting – 12.40%; 11.11; 40.00 (27.60)
headache – 34.11%; 38.89; 70.00 (35.89)
black-out – 42.64%, 33.33; 70.00 (27.36)
tinnitus – 59.69%; 44.44; 85.00 (25.31)
numbness – 66.67%; 38.89; 65.00
Patients with chronic delayed vestibular dysfunction had more expressed dizziness complaints than the patients with acute neurosensory hearing decrease and had not very significant difference in comparizon with ATO group. In ATO contingent significant complaints were of headaches – 35.89%; vomiting – 27.60; black-out – 27.36; tinnitus – 25.31; nausea – 23.14 and dizziness – 21.08%.
Comparizon of the complaint profiles of patients with acute and delayed blast injuries is presented at Fig. 3.
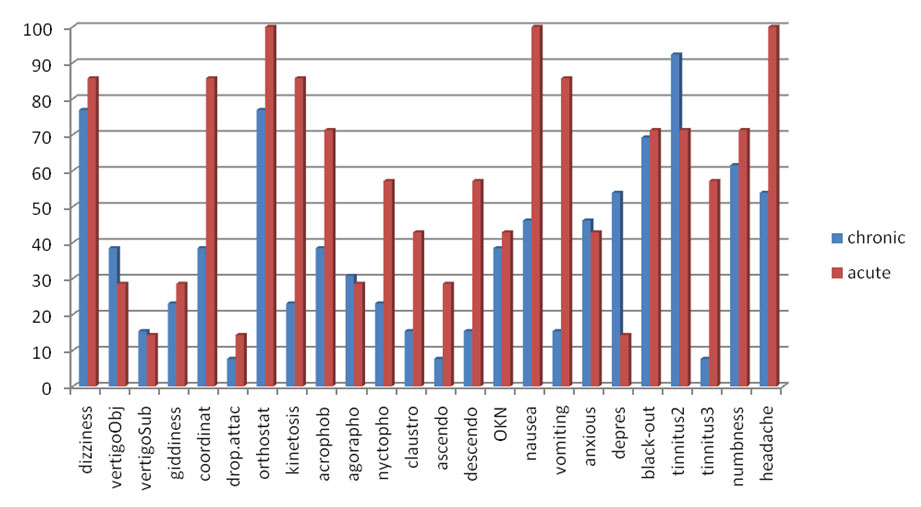
Attention was paid to significant difference (20%) and very significant difference (37%). In the acute period very significant appeared to be: imbalance, kinetoses, descendophobia, nausea, vomiting, tinnitus III type. Significant were: acrophobia, nyctophobia, claustrophobia, ascendophobia.
In the delayed period (in the order of decrease): depression, tinnitus II type, objective vertigo, anxiety, agoraphobia, subjective vertigo.
Tinnitus II type [2] mascable, related to neurosensory disorders of peripheral hearing apparatus, wanted special investigation. Therefore most of the patients have passed tonal audiometry, the results of which being presented at Fig. 4. This type of data have been observed in the most of the ATO patients examined.
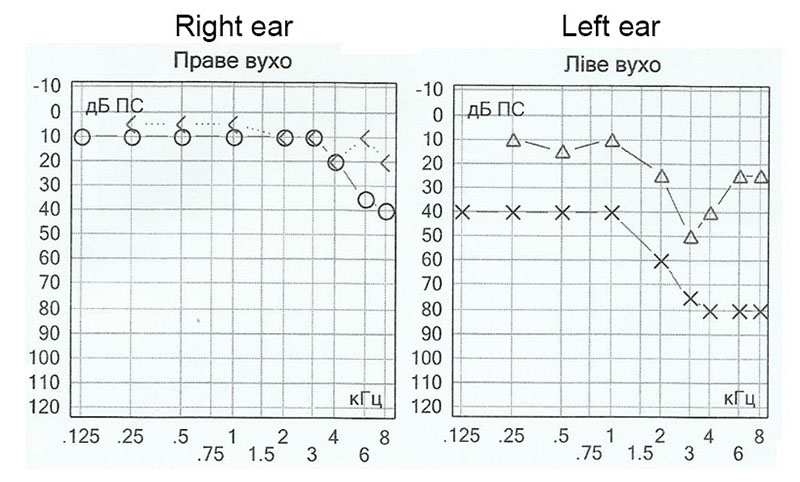
The audiogram presented have shown in delayed period the development of disorder both by air and bone conduction, which appeared not at the moment of explosion but developed later. This indicated the long-lasting degenerative processes.
Headache structure in the ATO and non-ATO groups have been presented at Fig. 5.
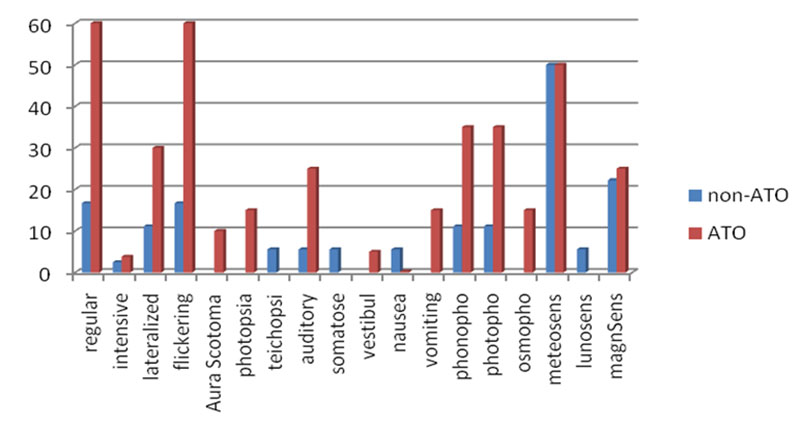
Among ATO group much more patients have complained of regular flickering. Less expressed, but significant have been laterized headaches, with acoustic aura, phono, photophobia, vomiting spells and osmophobia.
We pay special attention that symptoms of paroxismal disorders like migraine in ATO group have been met up to 60% regular and flickering headaches and in more than 30% cases the syptoms being laterized, with photo and phonophobia.
Headache intensity was estimated by the patient according to 5-point score:
- 1 point – patient was able to perform all types of activity both professional and routine;
- 2 point – patient was unable to perform difficult activities;
- 3 points – patient could perform simple tasks;
- 4 points – patient could only serve himself;
- 5 points – patient need special medical service.
The results are presented at Fig. 6.
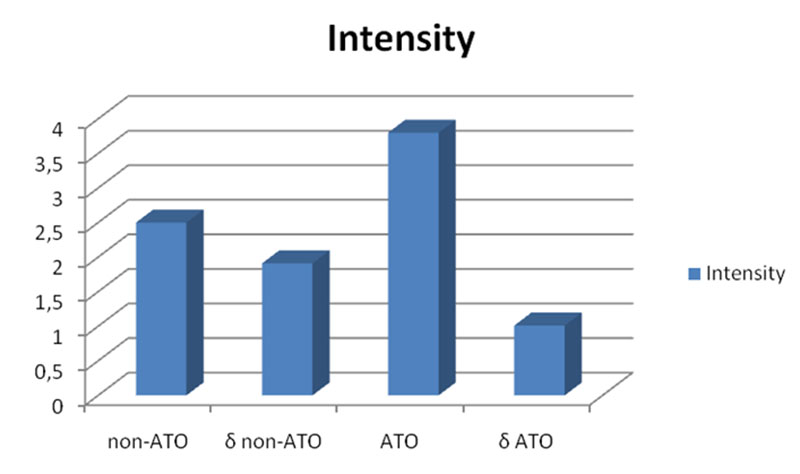
Difference significance between non-ATO and ATO according to F-test was 0.08, T-test – 0.27. It is possible to suppose that the increase of the number of patients should present the significant difference of the headache intensity between ATO participants and non-ATO contingent according to qualitative F-test, which is important to establish that ATO group has specific disease.
Headache structure in the acute and chronic period after blast injury is presented at Fig. 7.
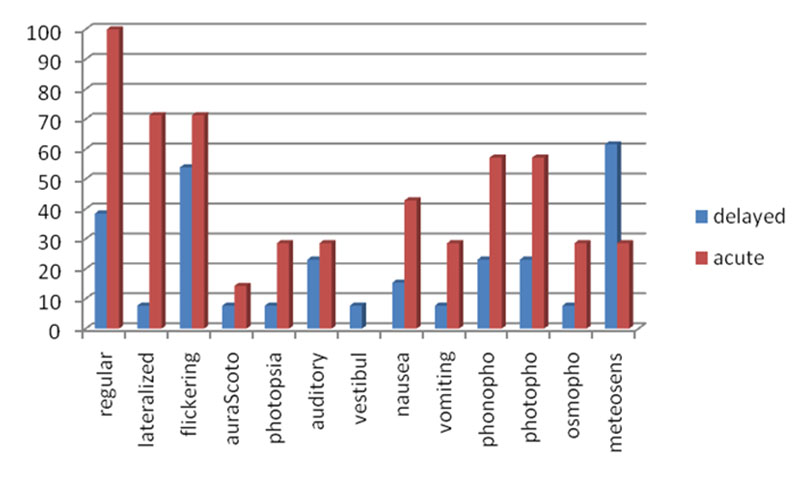
Important is the fact that almost all acute period patients had regular headaches, about 70% patients in acute period had laterized and flickering spells, 40-50% had phono and photophobia, more than 40% – nausea and up to 30% – different types of aura with vomiting and osmophobia, indicating severe dysfunction. The headache intensity has been estimated by patients to be the same in acute and chronic periods.
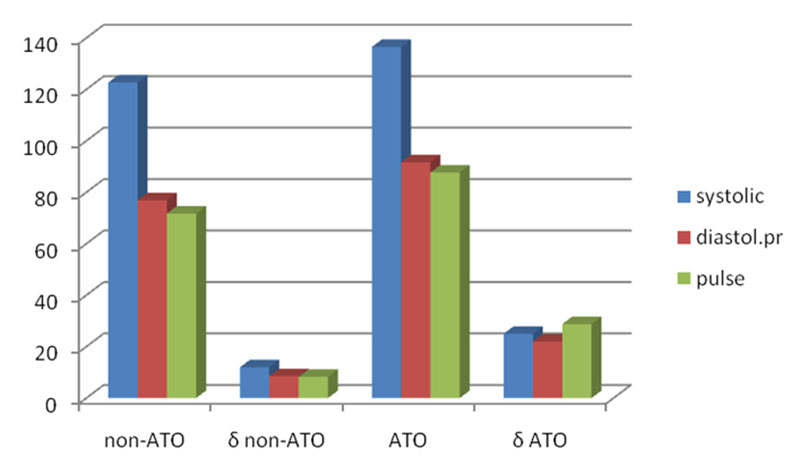
Blood pressure and pulse in non-ATO and ATO groups are depicted at Fig. 8. and at Table 1 the significances of differencies are presented according to F-test and T-test data.
| Table 1. Significances of the differencies for blood pressure and pulse in non-ATO and ATO groups | |||
| systol.pres | diastol.pr | pulse | |
| F-test | 0.015105 | 0.002247 | 0.00053 |
| Т-test | 0.070722 | 0.027351 | 0.197324 |
According to F-test in the ATO participants blood pressure have been significantly higher, thus indicated the additional quality in this group – hypertension as disease.
Pendular test
Spontaneuos Nystagmus, percentages and directions in non-ATO (patients with neuro-sensory hearing decrease) and ATO groups are presented at Fig. 9.
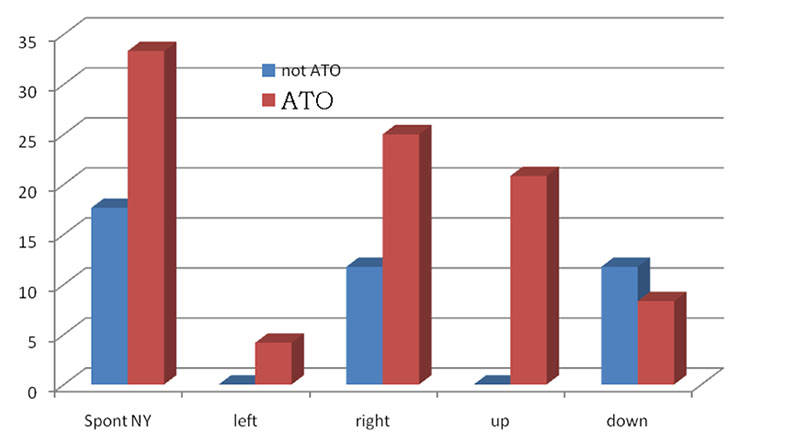
The data presented shown that spontaneous nystagmus was observed more frequently in the ATO group. Tolerability of the rotatory tests have been also different in two groups. 94.12% of non-ATO group tolerated well pendular test at 0.01 Hz, while only 83.33% from ATO contingent. All the othe frequencies non-ATO group tolerated 100%, while only 83.33% among ATO participants.
Gain compatizon for non-ATO and ATO groups is presented at Fig. 10.
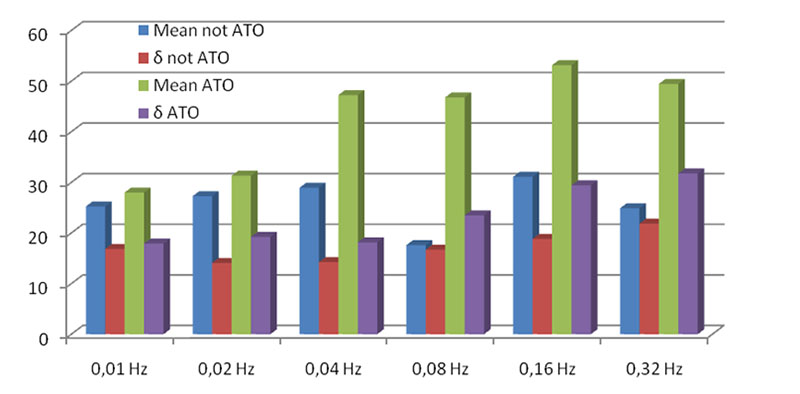
At 0.02, 0.08 and 0.32 Hz frequencies gain was decreased in comparizon to norm for ATO, for non-ATO the gain was decreased at all the frequencies, starting from 0.02 Hz and higher. At the frequencies 0.08 and 0.32 Hz the differencies appeared to be significant. The singficances of difference according to F-test and T-test are presented at Table 2.
| Table 2. Gain coefficients and their difference significances according to qualitative F-test and quantitative T-test. Bold font is used to indicate the parameters outside of normative range, significant and close to significant differencies | ||||||
| Frequency | 0.01 | 0.02 | 0.04 | 0.08 | 0.16 | 0.32 |
| Mean non-АТО | 25.24 | 27.29 | 28.94 | 17.60 | 31.12 | 24.88 |
| σ non-АТО | 16.84 | 14.09 | 14.26 | 16.70 | 18.83 | 21.83 |
| Mean АТО | 28.00 | 31.32 | 47.25 | 46.80 | 53.16 | 49.47 |
| σ АТО | 17.91 | 19.23 | 18.16 | 23.49 | 29.42 | 31.79 |
| F-test | 0.81 | 0.21 | 0.33 | 0.17 | 0.07 | 0.14 |
| T-test | 0.62 | 0.46 | 0.002 | 0.072 | 0.11024 | 0.01 |
Gain is rather variable parameter, therefore its diagnostic value is limited. Nevertheless attention has to be paid at the fact of decrease of the gain in both contingents and significantly higher level of it in ATO participants. The latter indicates the higher reactivity of the vestibular pathway nuclei.
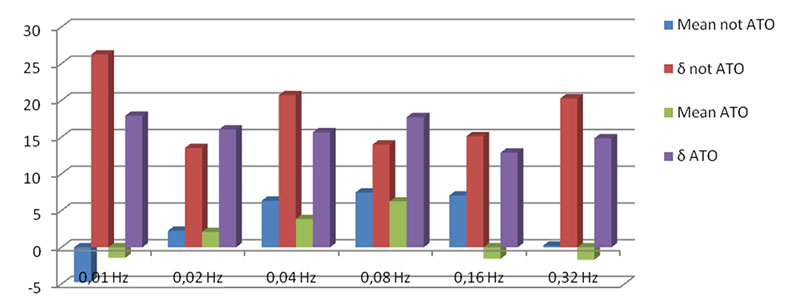
Phase shift – difference between phase angles of eye and chair positions (norm for healthy at frequencies): 0.01 Hz – 16.72-58.62; 0.02 Hz – 6.16-33.97; 0.04 Hz – 2.64-22.53; 0.08 Hz – (-3.69)-(+13.02); 0.16 Hz – (-9.51)-(+12.32); 0.32 Hz – (-14.78)-(+8.45); 0.64 Hz – (-14.96)-(+2.64) [4]. Phase shift is considered to be the most diagnostically important parameter, its data are presented at Fig. 11.
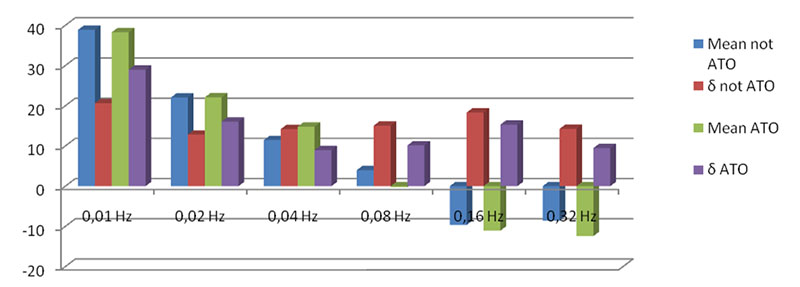
At the frequencies of 0.01-0.04 Hz and 0.16 and 0.32 Hz ATO group results were almost the same and being in the normal range. At 0.08 Hz ATO data exceeded norm and at 0.04 Hz the tendency has been seen to significant difference between non-ATO and ATO groups according to qualitative F-test. Attention was paid to big levels of standard devialion.
Difference significancies of the phase shift coefficients according to F-test and T-test are presented at Table 3.
| Table 3. Phase shift coefficients and their significance according to F-test and T-test. Bold font is used to indicate the parameters outside of normative range and close to significant differencies | ||||||
| Frequency Hz | 0.01 | 0.02 | 0.04 | 0.08 | 0.16 | 0.32 |
| Mean non-АТО | 38.88 | 22.06 | 11.47 | 4.00 | -9.65 | -8.59 |
| σ non-АТО | 20.63 | 12.82 | 14.20 | 15.06 | 18.32 | 14.26 |
| Mean АТО | 38.29 | 22.09 | 14.80 | -0.25 | -11.05 | -12.42 |
| σ АТО | 28.98 | 16.06 | 8.98 | 10.16 | 15.32 | 9.48 |
| F-test | 0.16 | 0.36 | 0.059 | 0.10 | 0.46 | 0.098 |
| T-test | 0.94 | 0.99 | 0.41 | 0.33 | 0.805 | 0.36 |
The result obtained might indicate the hyperexcitation of the midbrain nuclei.
Asymmetry data comparizon for non-ATO and ATO groups are presented at Fig. 12.
Difference significances for asymmetry coefficients according to F-test and T-test are presented at the Table 4.
| Table 4. Asymmetry coefficients and their significances for asymmetry coefficients according to F-test and T-test. Bold font is used to indicate the parameters outside of normative range | ||||||
| Symmetry | 0.01 | 0.02 | 0.04 | 0.08 | 0.16 | 0.32 |
| Mean non-АТО | -4.73 | 2.25 | 6.35 | 7.47 | 7.06 | 0.24 |
| σ non-АТО | 26.26 | 13.54 | 20.71 | 13.99 | 15.13 | 20.28 |
| Mean АТО | -1.43 | 2.10 | 3.85 | 6.25 | -1.56 | -1.68 |
| σ АТО | 17.92 | 16.06 | 15.67 | 17.73 | 12.89 | 14.86 |
| F-test | 0.10528 | 0.4269 | 0.246 | 0.3431 | 0.5175 | 0.205 |
| T-test | 0.67413 | 0.9753 | 0.6857 | 0.8164 | 0.08 | 0.75 |
Gain asymmetry – gain ratio of the right and left eye, normal values does not exceed 14.76%. The data obtained indicated great deviation in both groups without visible asymmetry. This means the absense of local unilateral lesions in the patient groups investigated.
In many patients nystagmus frequency and Slow Phase Velocity (SPV) were different even during one test, as it being shown at Fig. 13.
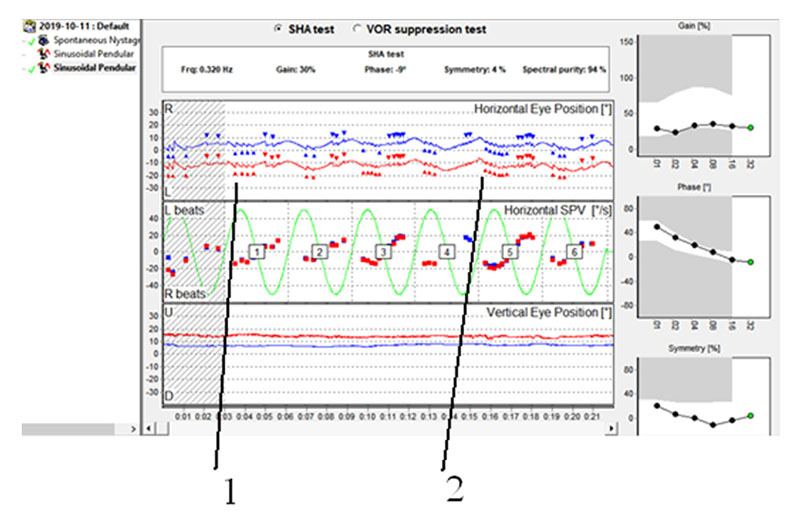
Even more exaggerated it is ween at Fig. 14, moreover one could boserve also the episodes of eyes convergence during the nystagmus birsts.
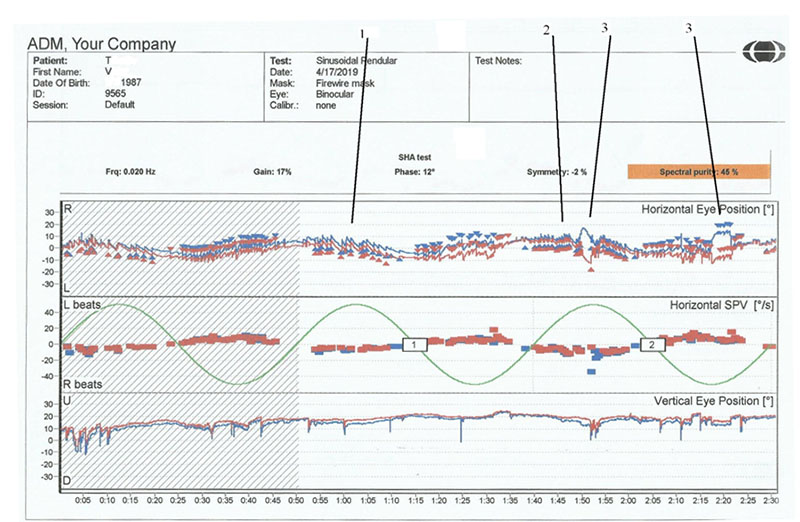
This phenomenon has influenced Spectral purity data. Spectral purity data comparizon while performing pendular test for non-ATO and ATO groups are presented at Fig. 15.
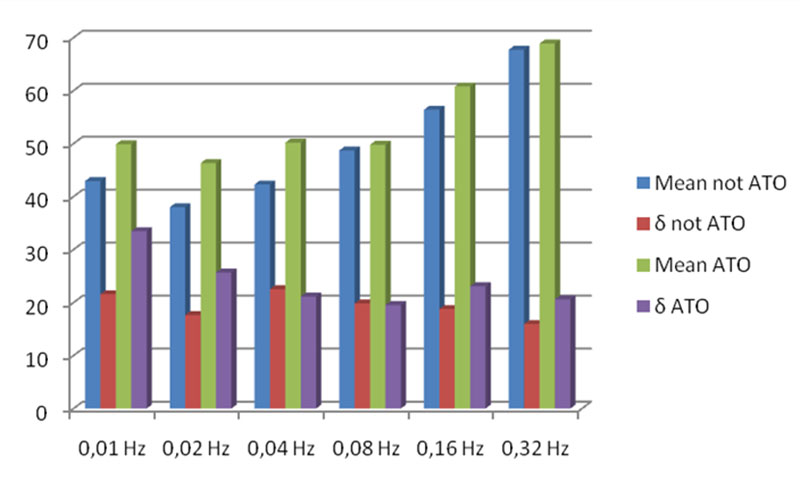
Difference significances for them according to F-test and T-test are presented in the Table 5.
| Table 5. Percentages of spectral purity and their significancies for asymmetry coefficients according to F-test and T-test. Bold font is used to indicate the parameters inside of normative range, and close to significant differencies | ||||||
| Spectral purity | 0.01 | 0.02 | 0.04 | 0.08 | 0.16 | 0.32 |
| Mean non-ATO | 42.94 | 38.00 | 42.29 | 48.71 | 56.40 | 67.73 |
| δ non-ATO | 21.57 | 17.64 | 22.54 | 19.84 | 18.79 | 15.95 |
| Mean ATO | 49.88 | 46.32 | 50.20 | 49.80 | 60.79 | 68.89 |
| δ ATO | 33.47 | 25.67 | 21.13 | 19.53 | 23.09 | 20.63 |
| F-test | 0.0747 | 0.1408 | 0.7785 | 0.9366 | 0.4993 | 0.33286 |
| T-test | 0.4253 | 0.244 | 0.2818 | 0.8673 | 0.5398 | 0.85433 |
Minimal significant spectral purity is not less than 60%. It has increased with the increase of pendular frequency and in ATO contingent has been insignificantly higher.
Discussion
In ATO group the complaints of vestibular and hearing disorders have appeared to be much more expressed. The latter might be explained using the results of animal experiments. The authors observed significant loss of stereocilia on hair cells in the central zones of all the receptor organs (I type hair cells), while peripheral zones of receptors (II type hair cells) appeared to be intact up to 1 month after blast-wave exposure. Following a single blast exposure, the number of stereocilia in the central regions were reduced to about half of the normal number. Most of the stereocilia damage observed consisted of a complete loss of all cilia on each affected hair cell.
Damage remained throughout the 28 days post-blast exposure period, suggesting that little stereocilia repair during this time frame occurred. Significant reductions in the ability to perform the righting reflex and balance on a rotating rod that lasted several weeks after blast exposure were prominent behavioral effects. A significant reduction in horizontal vestibuloocular reflex gain and phase lags in the eye movement responses that lasted many weeks following a single blast exposure event were also observed. Initially observed an increase in hVOR gains (hypermetric response) 1 day post-blast exposure. Subsequent days’ post-blast exposure exhibited gain decreases and phase lags that lasted through post-blast day 28 [8].
In ATO participants more exaggerated appeared to be complaints of dizziness, ortostatics, nausea, black-outs and type II tinnitus. Patients with delayed consequences of vestibular disorders had higher complaints expression than in the patients with acute neurosensory hearing decrease; ATO group comparizon has not revieled very significant differencies in symptomatics. In ATO contingent complaints of headache, vomiting spells, black-out, tinnitus, nausea and dizziness have been more often.
In acute period of blast injury imbalance, kinetoses, descendophobia, nausea, vomiting, type III tinnitus and headaches are more expressed. Type III tinnitus non-mascable, related to hyperacousia, has indicated the primary cochlea hair cells irritation, which later transformed into their degeneration manifested by type II tinnitus.
In delayed period (in the order of expression decrease): depression, type II tinnitus, objective vertigo, anxiety, agoraphobia and subjective vertigo were prominent. We have shown that I type hair cells are mostly responsible for vertigo, while II type hair cells – dizziness [13], being the explanation for the symptoms dynamics described.
It was logic to suppose that in the case of mild blast injury the ligaments between hearing ossicles were initially impaired, which later developed ossification. Hair cells and cochlear nerve fibres have degenerated in parallel.
Among ATO group much more patients complained of regular flickering, lateralized headaches with acoustic aura, photo and phonophobia, vomiting spells and osmophobia. These indicated paroxismal, migraine like character of headache.
Especially in acute period almost all patients had regular headaches, about 70% patients in acute period had laterized and flickering spells, 40-50% had phono and photophobia, more than 40% – nausea and up to 30% – different types of aura with vomiting and osmophobia, indicating severe dysfunction.
In ATO participants blood pressure (BP) has been significantly higher, thus indicating the necessity of the BP controll in the delayed period of the blast injury patients.
Spontaneous nystagmus in ATO contingent was met more often than in other patients, for the first the most typical was upbeating and for latter – downbeating nystagmus. Tolerance to rotation tests was different for patient groups described, ATO members demonstrated clearly expressed vegetative reaction to motion and poor tolerability of pendular loading.
Gain has been decreased in both groups of patients, and in ATO group it was significantly higher than in non-ATO team. This fact has indicated the higher activity of vestibular tract nuclei in ATO participants.
Phase shift in ATO members manifested that their midbrain vestibular nuclei were in excited condition.
Asymmetry data indicated the absense of local unilateral damages of vestibular system in both patient groups.
In many patients pendular test caused nystagmus of variable frequency, amplitude and SPV, thus resulted in lower values of spectral purity. The fact of variability of nystagmus and its SPV needs special investigation.
Conclusions
In АТО patients with moderate whole body blast exposure our investigation has revieled significant vestibular dysfunction.
In the acute period excitatory processes prevailed, therefore patients need vestibular blockers: histaminic, calcium, muscarinic.
In delayed period depression, type II tinnitus, vertigo spells dominated, requiring combined management, especially with nootrops.
Audiometric data in delayed period indicated combined hearing impairment: otosclerosis with neurosensory hearing decrease. Patients needed complex management.
Otosclerosis might want aladronates or risadronates.
Neurosensory impairment needed nootrops, nucleotides, sulfur group donators, Crebbs cycle activation, PRP-technologies.
ATO members need BP monitoring and correctiion.
Literature
- Akin FW, Murnane OD. Head injury and blast exposure: vestibular consequences. Otolaryngol Clin North Am (2011) 44(2):323–34.10.1016/j.otc.2011.01.005
- Claussen CF., Franz B. Contemporary & practical neurootology. Solvay, Hannover, 2006, 410p.
- Cernak I, Noble-Haeusslein LJ. Traumatic brain injury: an overview of pathobiology with emphasis on military populations. J Cereb Blood Flow Metab. 2010;30(2):255-266.
- Desmond AL. Vestibular function: evaluation and treatment. Thieme, New York, Stuttgart, 2004, 228p.
- Greer N, Sayer N, Kramer M, et al. Prevalence and Epidemiology of Combat Blast Injuries from the Military Cohort 2001-2014 [Internet]. Washington (DC): Department of Veterans Affairs (US); 2016 Feb
- Haesendonck G Van, Van Rompaey V, Gilles A, Topsakal V, Van de Heyning P. Otologic Outcomes After Blast Injury: The Brussels Bombing Experience. Otol Neurotol. 2018 Dec;39(10):1250-1255. doi: 10.1097/MAO.0000000000002012
- Hoge CW, Goldberg HM, Castro CA: Care of war veterans with mild traumatic brain injury-flawed perspectives. N Engl J Med 2009;360:1588–1591
- Lien S., Dickman J. D. Vestibular Injury After Low-Intensity Blast Exposure. Front Neurol. 2018;9: 297. Published online 2018 May 14. doi: 10.3389/fneur.2018.00297 PMCID: PMC5960675 PMID: 29867715
- Scherer MR, Schubert MC: Traumatic brain injury and vestibular pathology as a comorbidity after blast exposure. Phys Ther 2009;89(9):1–13
- Stuhmiller J.H. Blast Injury Translating Research Into Operational Medicine. Edited by Santee W.R., Friedl K.E., Borden institute, Publisher: Office of the Surgeon General 2010, 71 p. ISBN: 0160854474
- Trinus K. Vestibular system: morpho-physiology and pathology. Lambert Academic Publishing. 2012, 544 p. ISBN 978-3-659-11350-5
- Trinus KF., Claussen C.-F. International Clinical Protocol on Vestibular Disorders (Dizziness). Neurootology Newsletter, 2016, Vol. 10, № 1, ISSN 1023-6422 http://sites.google.com/site/dizzylita http://happyvertigo.com
- Trinus KF., Claussen CF., Barasii SM. Vertigo and dizziness: differential diagnostics and individual treatment procedures. Neurootology Newsletter, 2008, Vol. 8, №2, 6-15.
- Tun C., Hogan A., Fitzharris K. Hearing and vestibular dysfunction caused by-blast injuries and traumatic brain injuries. The Hearing Journal: November 2009 – Volume 62 – Issue 11 – p 24-26 doi: 10.1097/01.HJ.0000364272.60094.e6