Anirban Biswas
CONTENTS
Physiology of maintenance of balance: An overview
- Introduction
- Functions of the balance system
- Functions of the vestibular labyrinths
- Role of CNS in the maintenance of balance
- Vestibular reflex pathway
- Vestibular physiology in health and disease states
Approach to evaluation of patients with balance disorders
Clinical examination of balance disorder patients
- Objective of clinical examination
- Clinical features of peripheral and central vestibular disorders
- Clinical tests for diagnosis of balance disorders
- List of clinical tests in balance disorder patients
Diagnostic investigations in vertigo patients: Role of modern vestibulometry
- Vestibulometry – Where does it stand today?
- Objectives of modern vestibulometry
- Diagnostic tools in modern vestibulometry
- Ideal vestibulometric testing
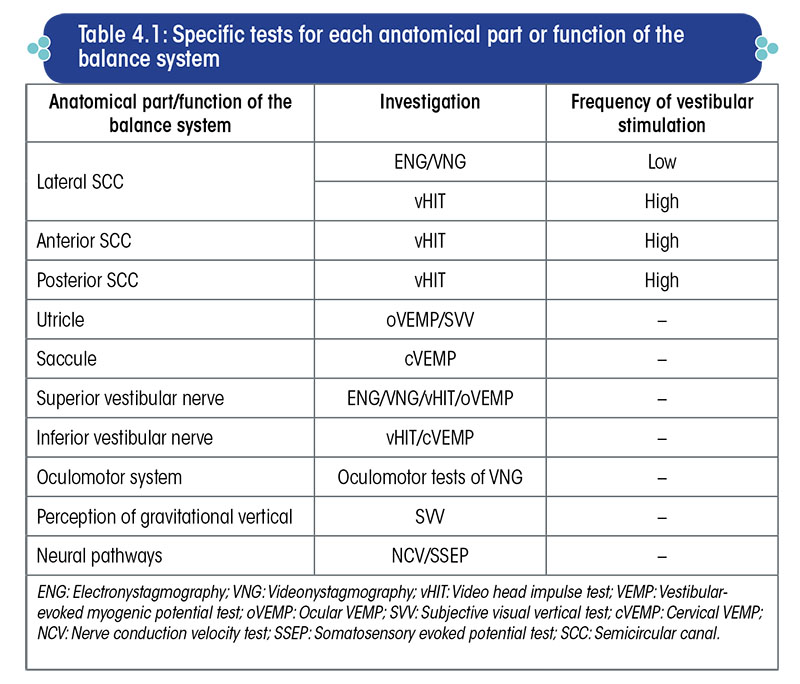
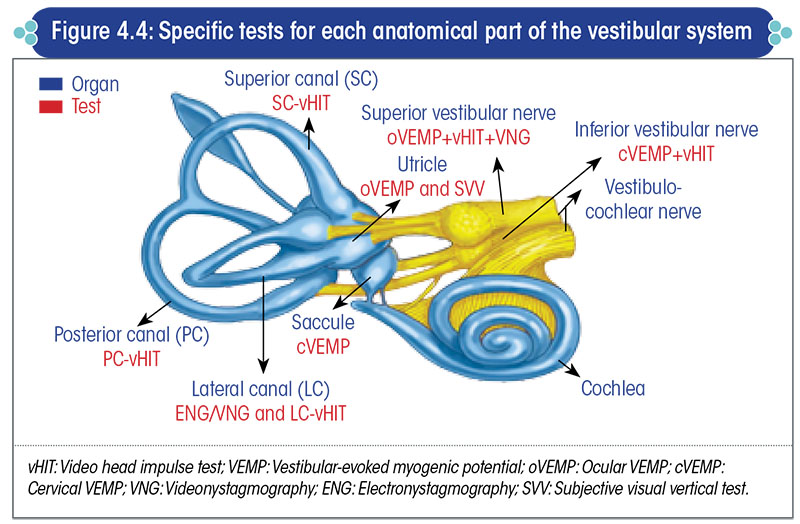
- Specific tests for different anatomical parts of the vestibular system
- Video head impulse test
- Subjective visual vertical test
- Vestibular-evoked myogenic potential test
- Posturography
Key take-home messages
Physiology of maintenance of balance: An overview
The anatomy and physiology of the balance system have been discussed in detail in a separate module titled ‘Clinical Physiology of the Vestibular System’. In this module, only a brief overview is presented for recapitulation.
Introduction
Maintenance of balance is an interplay of different physiological systems and numerous organs that comprise each of these systems.
The central and peripheral nervous systems, the vestibular system, the musculoskeletal system, as well as the cognitive and psychic systems work harmoniously and in tandem to maintain the body’s balance. A defect in any of the above systems can lead to a balance disorder.
Anatomy of the balance system
The anatomy of the balance system is pretty convoluted, consisting of a number components of various physiological systems (Figure 1.1). It is possibly the most complex biological system in the human body.
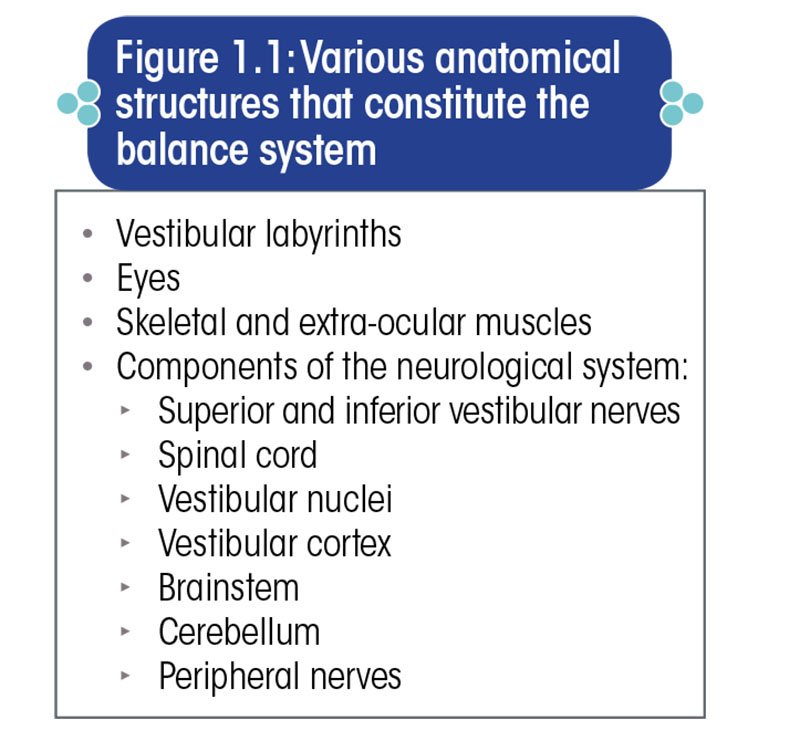
The vestibular labyrinth forms the non-auditory part of the inner ear. Its anatomical structures are depicted in Figure 1.2.
Functions of the balance system
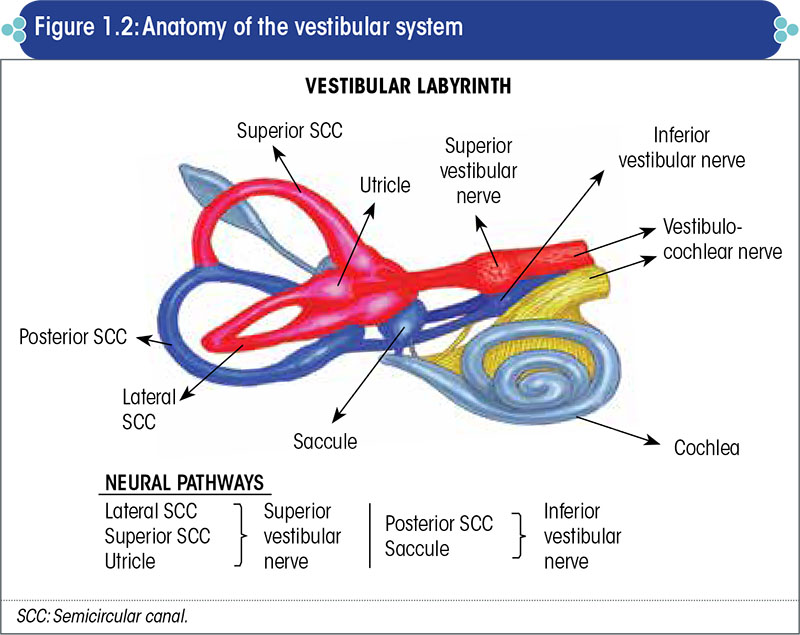
The balance system serves three primary functions, as given in Figure 1.3.
Postural stability is the faculty by virtue of which an individual can comfortably stand upright and is prevented from falling.
Gaze stabilization or visual stability is the faculty by virtue of which objects in the visual field remain stable and do not appear to be moving when the head is moved, or when the visual surroundings move, or when both, the head and the visual surroundings move.
Perception of verticality and horizontality is the subjective ability to sense the spatial orientation of an object with respect to gravity.
Functions of the vestibular labyrinths
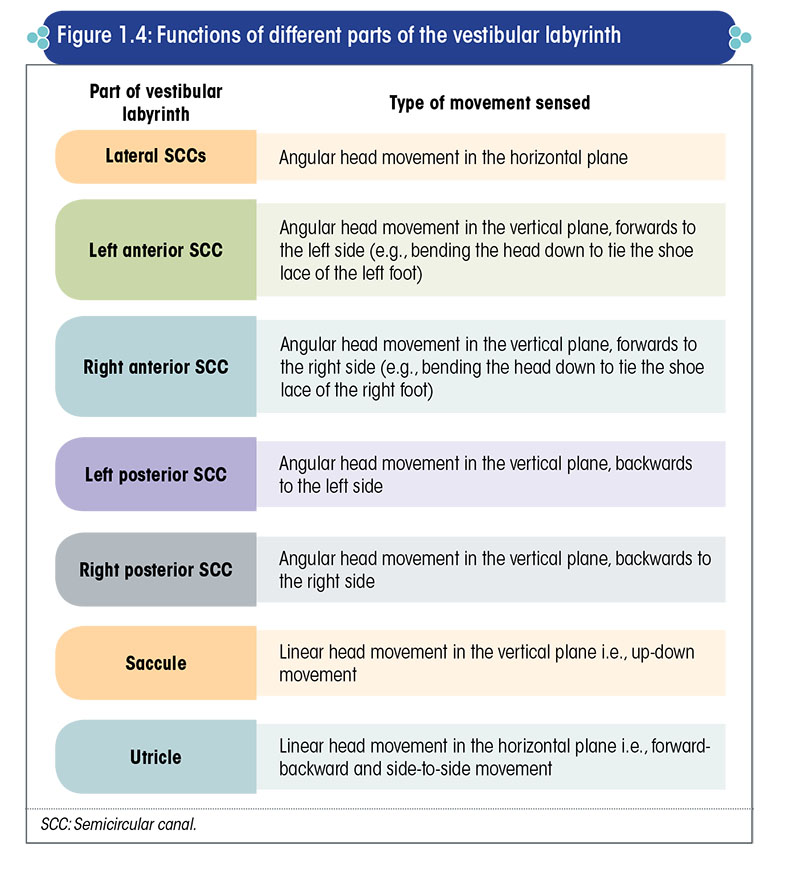
Each part of the vestibular labyrinth has a specific function (Figure 1.4).
Role of CNS in the maintenance of balance
Maintenance of balance is essentially regulated by the central nervous system (CNS) (Figure 1.5).
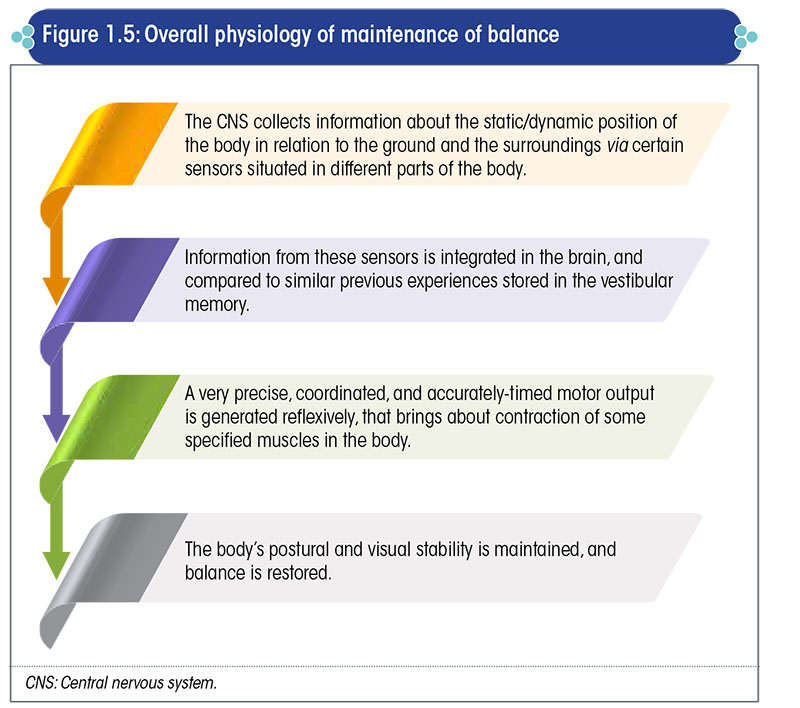
Additionally, the cognitive and psychic systems play a major role in the maintenance and control of balance.
Vestibular reflex pathway
Any reflex in the body occurs via neural pathways that involve an afferent sensory system, consisting of an afferent sensory organ and an afferent neural pathway; a reflex center; and an effector motor system, consisting of an effector neural pathway and an effector motor organ.
The components of the vestibular reflex pathway are depicted in Figure 1.6.
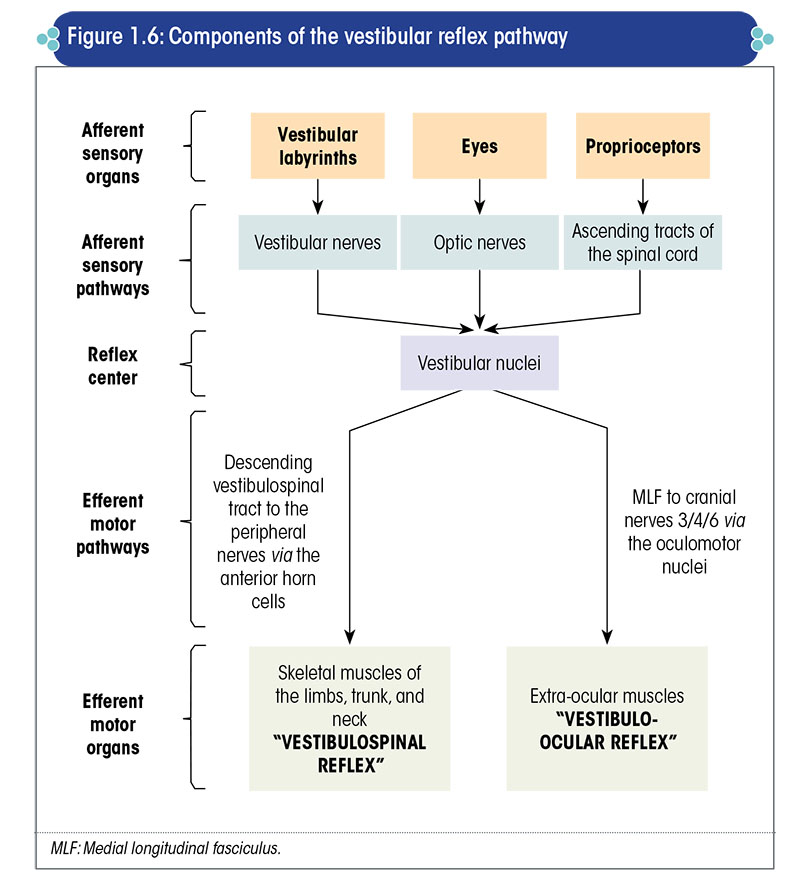
The afferent sensory system provides inputs to the brain, which are then integrated by the CNS.
The cognitive system, comprising the intelligence and cognitive skills, uses information stored in the brain to determine the nature of the motor response i.e., the manner and order of muscle contraction.
The cerebellum fine tunes the motor output by selecting the appropriate muscles and by controlling the duration/extent of contraction of each muscle involved.
Higher centers in the brain, such as the internal capsule, basal ganglia, and thalamus, also partly modulate the motor response.
The motor output generated by the brain is transmitted through the efferent motor system to produce two types of reflexes viz., the vestibulospinal reflex and vestibulo-ocular reflex. The vestibulospinal reflex is responsible for maintenance of postural stability, whereas the vestibulo-ocular reflex is responsible for maintenance of gaze stability.
Vestibular physiology in health and disease states
Normally, each of the vestibular labyrinths generates tonic discharges at a frequency of ≈80–100 spikes per second. At any given time, the discharge frequencies on both sides are in a state of dynamic equilibrium, which helps to maintain the body’s balance.
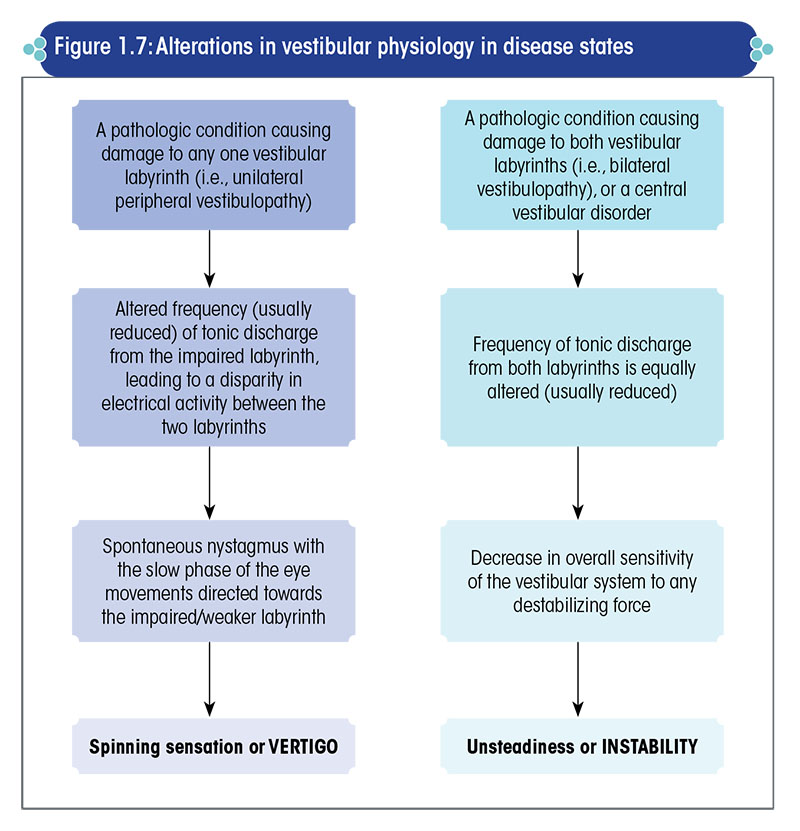
Vertigo, or the sense of spinning/rotating, occurs when there is a disparity in electrical activity between the two vestibular labyrinths.
Hence, individuals in whom one of the labyrinths is weak or damaged experience severe vertigo (Figure 1.7).
In case of damage to both the vestibular labyrinths, instability or unsteadiness, and not vertigo, is the primary symptom (Figure 1.7).
The stability of gaze and that of posture is brought about by a tonic contraction of the muscles of the eye and that of the body.
This tonic contraction is a dynamic process whereby the muscles of the eyes and that of the body are held in a state of sustained contraction, which pushes the eyes and the body to the opposite side. In other words, the left vestibular system pushes the eyes and the body to the right and vice versa.
When both the vestibular labyrinths are in a normal working condition, the force exerted by the two sides is equal, maintaining the eyes in the midline and the body in its erect posture.
Vertigo occurs when there is a disparity in tonic discharge from the two vestibular labyrinths
However, if one of the labyrinth is weak, then the other side takes the upper hand and becomes comparatively stronger, and pushes the eyes and the body to the side of the weaker labyrinth.
Thus, in left-sided vestibular weakness, the normal right side is comparatively stronger and the body tends to fall to the left side, accompanied by slow drifting of the eyes to the left side.
The slow drifting of the eyes to the left is corrected by a rapid movement of the eyes to the opposite side i.e., the right side, in an effort to bring the eyes back to the midline.
Once the eyes reach the midline, the comparatively stronger right side again slowly pushes the eyes to the left side, leading to a repetitive jerky movement of the eyes – slowly to the left and rapidly to the right.
Hence, in patients with left-sided vestibulopathy, there is a tendency to fall towards the left side, along with a right-beating nystagmus (the nystagmus is conventionally denoted by the direction of fast phase of the eye movement).
Perception of verticality is not related to muscle tone; it is primarily dependent on the function of the otolith organs (viz., the utricle and saccule, which are parts of the vestibular labyrinth), with some contribution from the cerebral cortex, as there is an element of perception in it.
One-sided vestibular weakness also induces changes in the perception of verticality, by shifting it to the side of the weaker labyrinth.
Nevertheless, as central vestibular compensation takes place, the tendency to fall to the side of the weaker labyrinth gradually subsides, the nystagmus beating towards the healthy side ceases, and the perception of verticality slowly normalizes.
Approach to evaluation of patients with balance disorders
Addressing a patient with vertigo does not imply the sole use of empiric treatment with anti-vertigo medications and continuing them eternally.
Vertigo or imbalance is merely a manifestation/symptom of an underlying disorder that needs to be accurately diagnosed and treated.
The overall evaluation of patients presenting with disequilibrium can be done using a three-pronged approach, as shown in Figure 2.1.
The sophisticated neurotological investigations like videonystagmography, video head impulse test, vestibular evoked myogenic potential test, craniocorpography, subjective visual vertical test, dynamic visual acuity, posturography, and imaging are required in only about 20% of the patients or even less.
Over-investigation is always deplorable; however, reasonable investigations to evaluate and document the functional, and in certain cases, the structural status of the vestibular system are essential.
Clinical examination of balance disorder patients
Objective of clinical examination
In patients with vertigo/imbalance, a thorough clinical examination helps to determine whether:
- The balance system is properly serving its functions of postural stability, gaze stabilization, and accurate subjective perception of the vertical (sense of verticality is a labyrinthine function, and should ideally tally with the gravitational vertical.)
- The sensory input system and motor output system of the vestibular reflex pathways are in perfect order both, structurally and functionally.
- The neural pathways connecting different anatomical structures of the balance system are in perfect order
The clinical examination does not give an idea about the psychic and cognitive control of the balance system and usually about the etiology of the balance disorder.
Clinical features of peripheral and central vestibular disorders
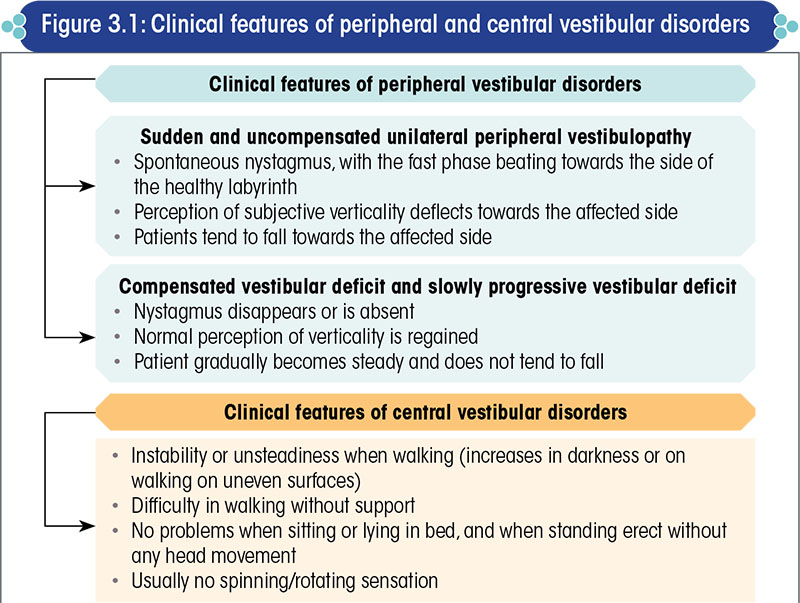
The general features of peripheral and central vestibular disorders are summarized in Figure 3.1.
Clinical tests for diagnosis of balance disorders
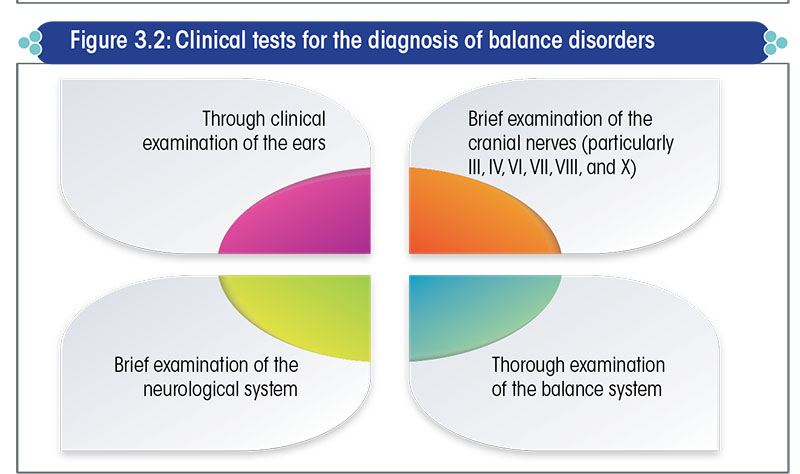
The clinical tests recommended for the diagnosis of a balance disorder (vertigo/imbalance) are listed in Figure 3.2.
Thorough examination of the ears
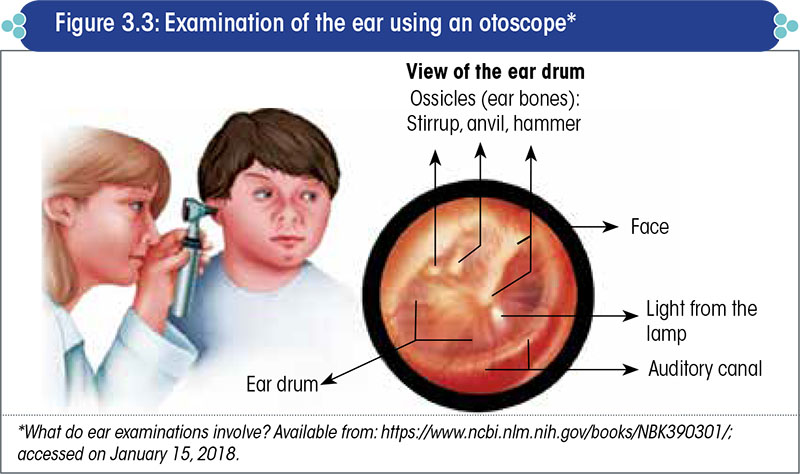
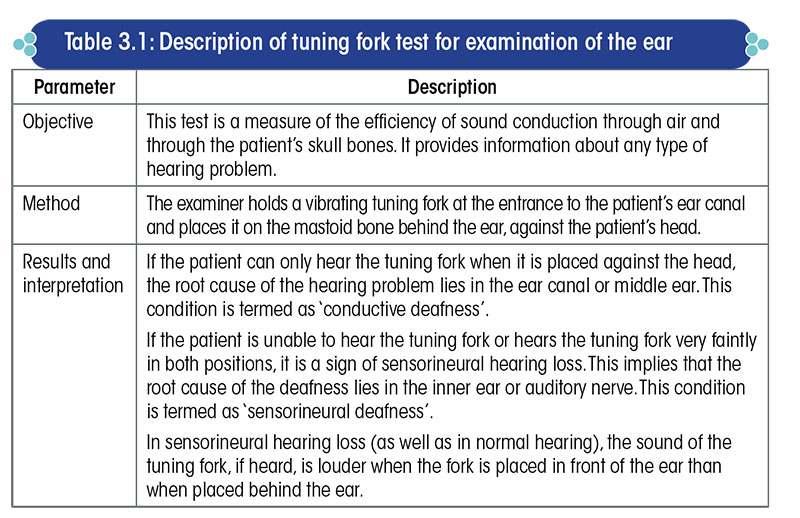
Ear examination should include otoscopy (Figure 3.3) and tuning fork tests (Table 3.1). Look for and document any perforation in the ear drum, distortion in the cone of light, or marks of surgery. Results of the tuning fork tests also need to be documented.
Additionally, the patient should be specifically asked to report any type of hearing loss or deafness, tinnitus, heaviness/fullness in the ears, and if the hearing loss/tinnitus/aural fullness increases before or during each attack of vertigo.
Brief examination of the cranial nerves
Examination of the cranial nerves requires testing of at least the third, fourth, fifth, sixth, seventh, and eighth cranial nerves, if not all.
Eye tests include the oculomotor tests, which are part of both, the eye tests and the neurological tests relevant in all balance disorder patients. The oculomotor tests are discussed separately in detail in a later part.
The eye tests form a very important part of the clinical examination.
- Eyes are one of the three main input systems to the balance system.
- The vestibular labyrinths and their vital connections to the brain are situated deep inside the skull, housed within the hardest bone and a practically inaccessible area of the human body, very difficult to reach by instruments and to visualize.
- Abnormalities in the vestibular system, comprising the vestibular labyrinths and their connections to the CNS, lead to changes in eye position and movements; hence, eyes are the best window to ascertain the functioning of the vestibular system.
- The motor mechanism that controls the movement of the eyes viz., the oculomotor system, is essential for gaze stabilization, which is one of the primary functions of the vestibular system and, hence, needs to be evaluated thoroughly.
The following basic eye tests are suggested for the examination of cranial nerves that are most relevant in vertigo patients.
Tests for eye movements
Ask the patient to follow the examiner’s finger with his eyes, without moving the head. Move the finger linearly to six cardinal points in an ‘H’ trajectory (Figure 3.4).
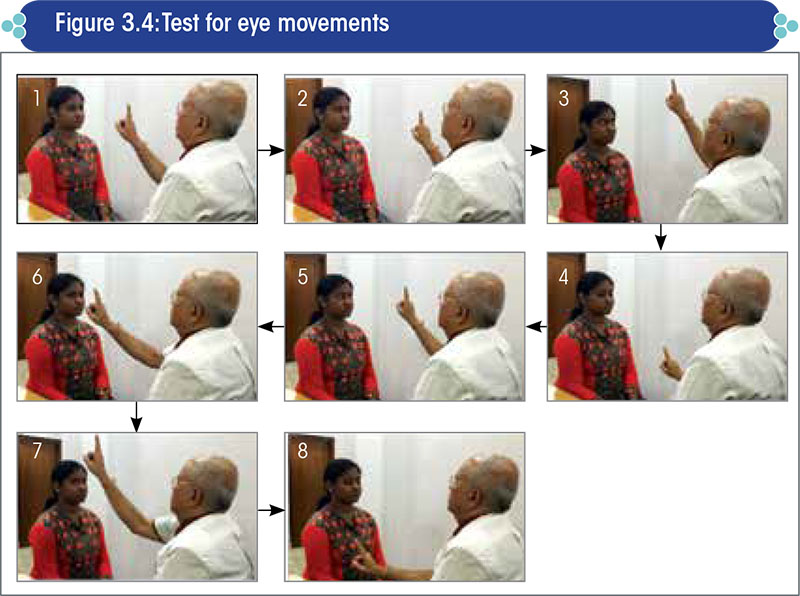
Enquire about the presence of double vision (diplopia) in any particular eye position. Also, ask the patient about any gaps or blank areas in the field of vision when observing the moving finger.
Assess for:
- Failure of smooth movement of the eyes and any fatigability and gradual drooping of the eyelids, which is indicative of myasthenia gravis. Carefully see if both the eyes lie in the same horizontal plane. If one eye is above or below the horizontal plane, it is sign of skew deviation. Although abnormalities in these tests are not very common, each and every patient must be assessed for the same.
- Nystagmus: The finger movement is to be paused to check for nystagmus during upward, downward, and lateral gaze. Hold the finger static in the center about 15 inches away from the nasion to look for nystagmus in the primary position of gaze.
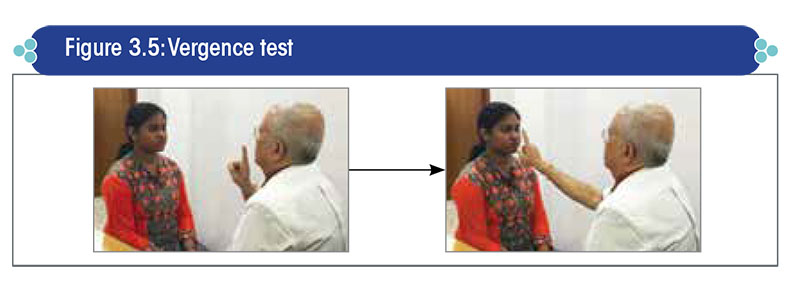
- Vergence anomalies: The examiner holds his index finger 18 inches in front of the patient`s eyes, and then gradually brings the finger in a linear fashion towards the bridge of the patient’s nose (Figure 3.5). A normal response consists of the near vision triad viz., convergence of eyes towards the midline, accommodation for near vision, and pupillary constriction. The absence of any one of the above results suggests a vergence disorder.
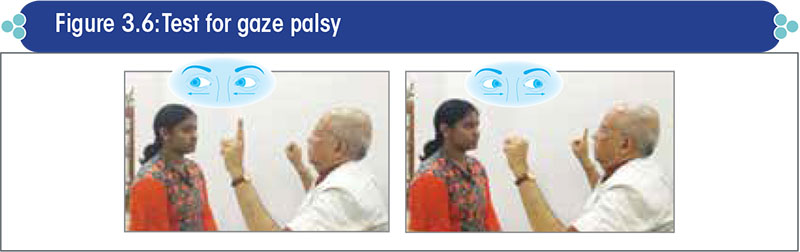
- Gaze palsies: These are suggestive of supra-nuclear lesions. Ask the patient to look alternatively at the finger of the left and right hand, held at a distance of ≈40 cm from the patient’s face and ≈30 cm away on either side of the midpoint between the two eyes (Figure 3.6).
- Impaired vestibulo-ocular reflex: It is assessed by performing the head impulse test (Figure 3.7). Instruct the patient to fix his gaze on the examiner’s nose. Then, hold the patient’s head and briskly turn it from the midline to either side, while observing the eyes for the presence of any corrective (sudden/jerky) movements immediately after (say 1/10th of a second later) the head movement. The head should be moved sideways at random by only about 10–15°, but the movement must be very fast and brisk with a sudden start and stop.

Test for corneal reflex
The corneal reflex test evaluates the cranial nerves V (afferent sensory fiber) and VII (efferent motor fiber).
Ask the patient to look up and towards one side; then, using a wisp of sterile cotton, lightly stroke the sclera on the side of the eye.
Look for blink in both eyes, and ask whether the patient can sense the stimulus.
Repeat the test on the other eye.
Test for corneal reflection
The patient is asked to fixate a torch-light at 1/3 m from the patient’s eyes. The location of reflection of light from both eyes should appear symmetric and generally slightly nasal to the center of the pupil.
In case of any asymmetry, suspect pathology of the extra-ocular muscle.
Test for eyelid control
In patients showing ptosis, suspect possibility of an oculomotor nerve pathology, Horner’s syndrome, or a neuromuscular pathology such as myasthenia gravis.
Other eye tests i.e., oculomotor tests, which are essential in a patient with vertigo, are discussed in a later sub-section under ‘Thorough examination of the balance system’.
Vestibulo-ocular tests
Disorders of the vestibular system generally cause an unsteady discharge of tonic impulses from the vestibular labyrinths. This jeopardizes the steady midline position of the eyes, and induces abnormal involuntary eye movements.
Vestibulo-ocular tests for evaluation of the balance system can be broadly classified into two groups, as under:
- Tests for abnormal spontaneous eye movements
- Tests for abnormal provoked eye movements
Tests for abnormal spontaneous eye movements
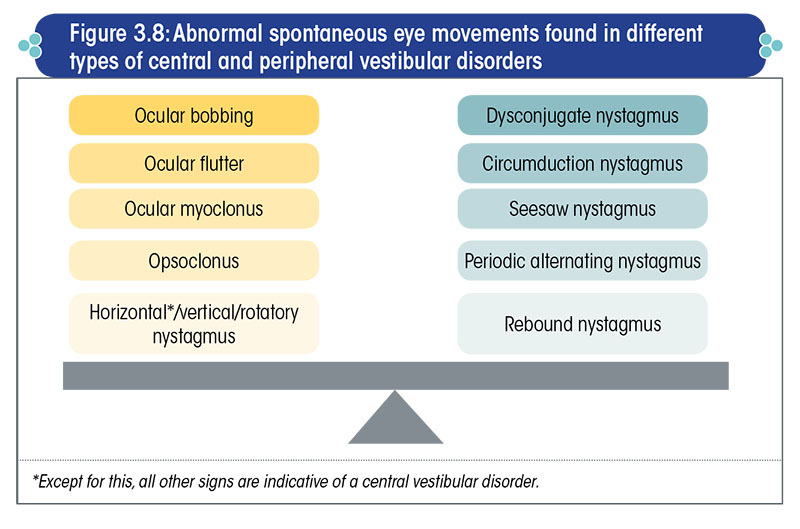
These tests simply involve asking the patient to keep his eyes open in the primary position of gaze, and looking into his eyes to identify any abnormal eye movements (Figure 3.8).
Ocular bobbing
Ocular bobbing is a distinctive disorder of eye movements, observed in patients with pontine dysfunction, but it can also occur in rare cases of acute cerebellar lesions.
It is marked by a rapid downward movement of the eyes, followed by a slow upward movement, with a slight pause which differentiates it from a down-beating nystagmus.
The simultaneous loss of horizontal eye movements suggests a bilateral pontine lesion and is a marker of very poor prognosis in neurology.
Ocular flutter
It is a rare abnormal eye movement consisting of irregular bursts of to-and-fro, bidirectional, horizontal saccades, and is frequently encountered in association with cerebellar symptoms.
It manifests as a swift horizontal oscillation in both eyes when staring straight ahead.
Ocular myoclonus
It occurs as bursts of pendular eye movements, normally associated with lesions in the midbrain.
Tests for abnormal provoked eye movements
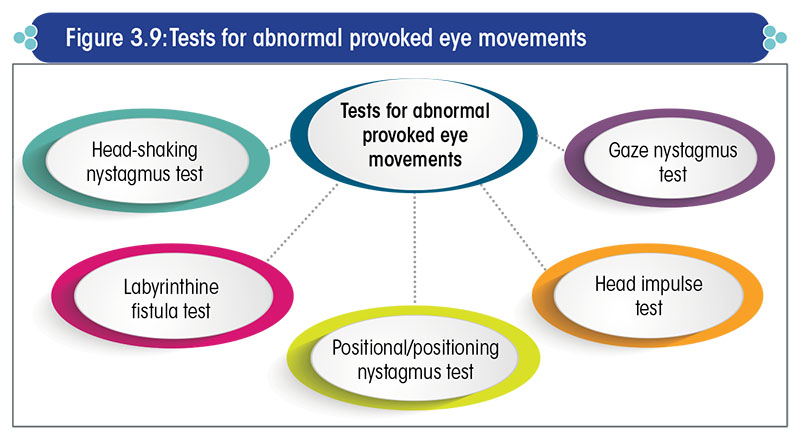
The tests for abnormal provoked eye movements are listed in Figure 3.9.
Gaze nystagmus test
This test is conducted to evaluate the gaze-holding function.
Check for nystagmus abnormally induced by looking 30o away (left, right, up, and down) from the mid-point.
Nystagmus in any position of gaze is abnormal, and suggests the presence of a lesion in the brainstem or cerebellum (usually the latter).
Head impulse test
This test assesses the vestibulo-ocular reflex (VOR) gain of the three semicircular canals in each ear.
It is considered to be one of the best and most reliable bedside tests to assess labyrinthine function.
The test procedure is the same as previously discussed in the subsection ‘Tests for eye movements’ under ‘Brief examination of the cranial nerves’.
Positional and positioning nystagmus tests
The positional and positioning nystagmus tests help to detect abnormalities in the otolith systems.
Positional nystagmus is provoked by placing the head in different positions (Figure 3.10).
- The patient ought to be tested in 11 head positions.
- Tests in other critical positions also have to be done.
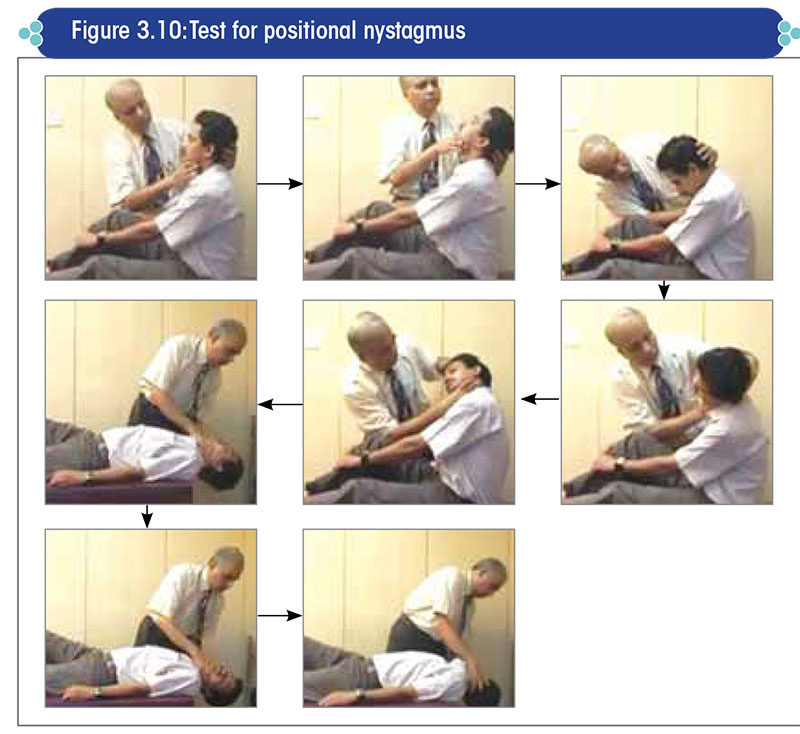
When performing the positional nystagmus test, care must be taken to ensure that the change of head position is brought about at a reasonably slow rate, to exclude dynamic influences as well as to avoid a sudden change in the head position.
The head should be maintained in each position for at least 30 seconds.
If nystagmus appears in any position, the following characteristics of the nystagmus should be noted:
- Latency
- Intensity
- Direction of beating
- Fatigability
- Vertiginous sensation
The Dix-Hallpike test is another useful test for positioning vertigo. It detects any positional nystagmus originating in the posterior SCCs, which are the commonest sites for benign paroxysmal positional vertigo.
- Before performing the test, explain to the patient what is going to be done and that any dizziness will only last a few seconds.
- Have the patient sit with his legs extended on the examination table. Ask him to keep his eyes open, and look directly at the examiner at all times.
- By placing one hand on top of the patient’s head and one hand under the chin, turn the patient’s head by 30-45° towards one side. Then, help him quickly lie back, so that the head hangs over the end of the table and is 45° to one side and about 20-30° below the horizontal (Figure 3.11).
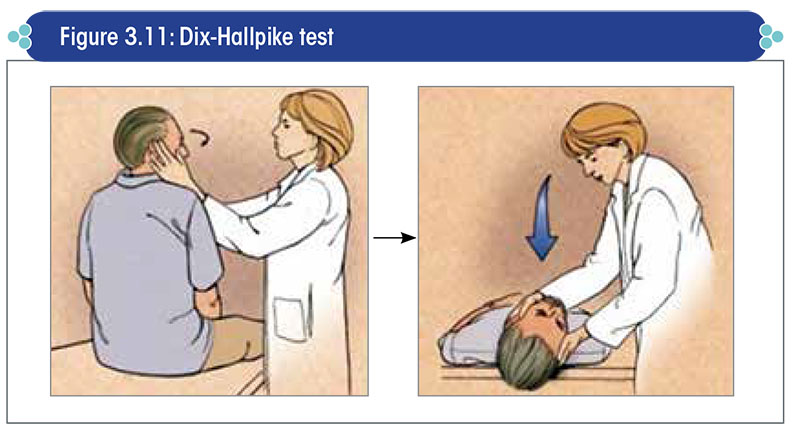
- Observe the eyes for at least 15 seconds to check for nystagmus. Usually, the nystagmus is rotatory in nature, beating mostly towards the floor (‘geotropic nystagmus’) and rarely upwards towards the ceiling (‘ageotropic nystagmus’).
- After the patient sits upright for a few minutes to recover from the vertigo, the procedure is repeated with the head turned in the opposite direction.
- Positive results include nystagmus produced when the patient is lying down with the head to one side. The side being tested denotes the side causing the positional vertigo.
- If the right side is being tested (in the ‘lying down’ position), the eye will rotate in a counter-clockwise manner during the rapid phase of nystagmus, with a minor up-beating vertical (toward the forehead) component.
- If the left side is being tested, the results are similar, except that the eye rotates clockwise.
Supine roll-over test for positional nystagmus originating in the lateral semicircular canals
The patient is made to lie down flat with his head raised by 10-15° and then turned to one side by 90°.
Any horizontal nystagmus is to be looked for; when present, it is usually on both sides. The side with a stronger nystagmus is the diseased side.
Fistula test
The fistula test is done to detect a fistula in the bony labyrinthine wall of the inner ear.
Method:
- Pressure changes in the external ear canal are brought about by applying intermittent pressure on the tragus (Figure 3.12) or, more preferably, by using a snugly fitting Siegel’s ear speculum.
- The patient’s eye movements are carefully recorded.
Positive result and interpretation:
- In a normal person, the test is negative because the pressure changes cannot be transmitted into the labyrinth (when there is no fistula).
- In fistula over the dome of the lateral semicircular canal, an increase in pressure causes a conjugate horizontal deviation of the eyes towards the normal side. As the pressure is maintained, jerk nystagmus develops with the fast component towards the affected ear. As the pressure is released, the eyes return to normal.
- Fistula of the lateral semicircular canal causes deviation of eyes to the affected side.
- Vestibular erosion causes rotatory horizontal nystagmus towards the diseased ear.
- Fistula of the posterior semicircular canal causes vertical movement of the eyes.
Head-shaking nystagmus test
Any nystagmus abnormally induced by head shaking is looked for.
The patient is instructed to keep his eyes closed, and his head is shaken from side to side for 20 times (Figure 3.13).
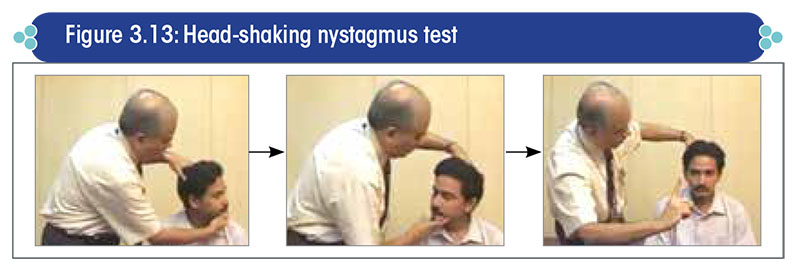
Then the patient is asked to immediately open his eyes, and nystagmus is checked.
A left-beating nystagmus indicates the presence of a right peripheral vestibular lesion and vice versa.
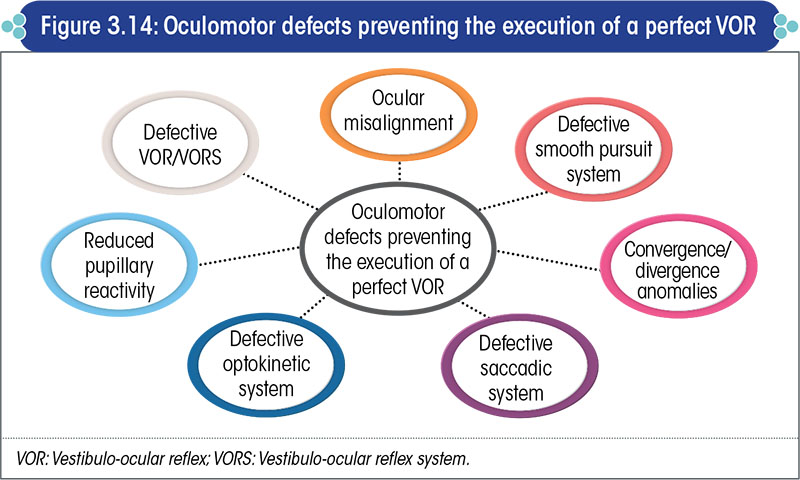
Oculomotor tests
Signs of oculomotor dysfunction
The vestibulo-ocular reflex may be jeopardized by defects in the oculomotor system (Figure 3.14).
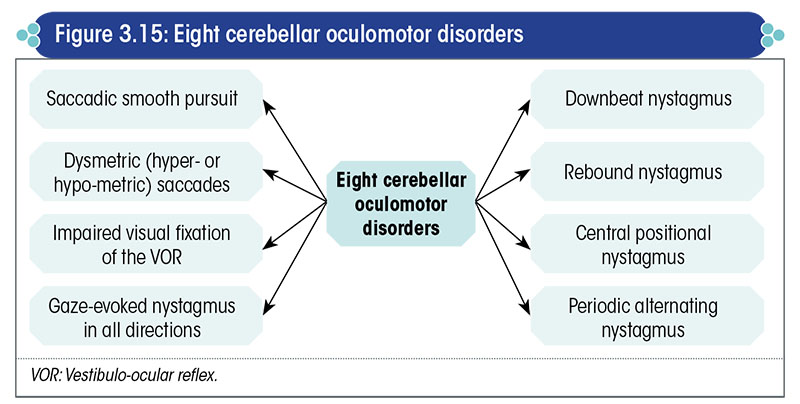
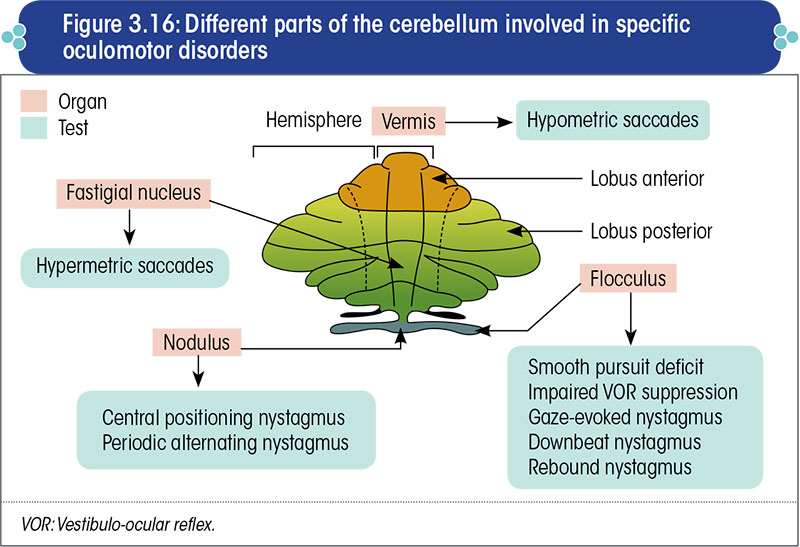
The cerebellar oculomotor disorders relevant to the assessment of the balance system are presented in Figure 3.15.
The specific anatomical part of the cerebellum that is responsible for each of these disorders is shown in Figure 3.16.
Eye tests relevant to the vestibular system are as under:
Head-tilt test
A contraversive tilt indicates (Figure 3.17):
- Lesions in the medial longitudinal fasciculus
- Superior oblique muscle paresis
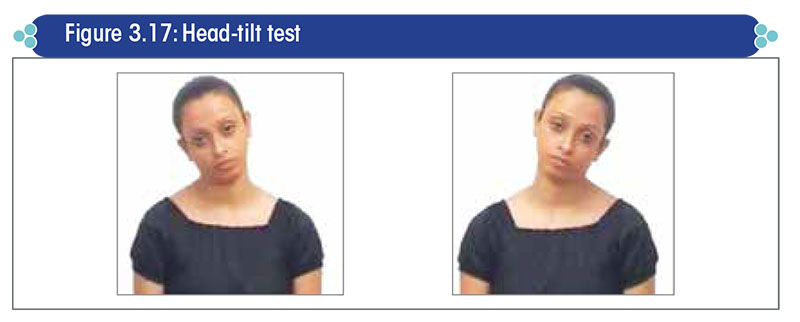
An ipsiversive tilt indicates:
- Peripheral vestibular lesions
- Lower pontomedullary lesions
Test for heterotropia (Cover test)
The cover test is also known as ‘test for skew deviation’.
It is a very important clinical test for patients with suspected central disorders, and is aimed to detect any misalignment of the visual axes.
In skew deviation, the cornea of one eye is at a slightly higher level than that of the other eye.
To perform the test, the patient is asked to fixate both eyes (Figure 3.18):
- At a near target (≈1 feet away)
- At a distant target (≈20 feet away)
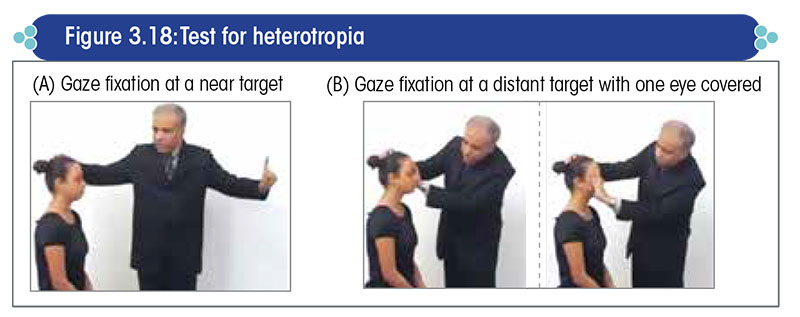
Then, as the patient fixates his eye continuously on a distant target, cover one eye and look for movement in the other eye.
A positive test is a sign of ocular misalignment or abnormal skew.
On covering one eye, if there is perceptible movement of the other eye, then the cover test is considered as positive and is indicative of heterotropia.
Test for smooth pursuit
The patient visually tracks a target (usually the examiner’s finger) moving at a speed of 15–200/sec, 18 inches in front horizontally and vertically (Figure 3.19).
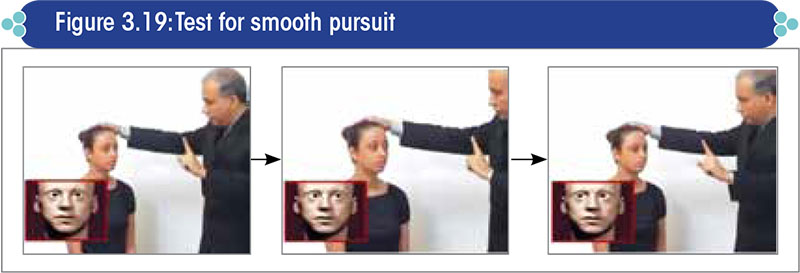
Any jerky eye movement is to be looked for. Normal subjects are able to perform the test very smoothly, with the eyes moving in a smooth, sinusoidal fashion.
The presence of saccades or jerks indicates a disorder in the smooth pursuit system (e.g., a cerebellar disorder such as spinocerebellar ataxia).
Vergence test
This test is the same as discussed earlier in the sub-section ‘Tests for eye movements’ under ‘Brief examination of the cranial nerves’ .
Saccade test
The patient looks back and forth between two objects (examiner’s fingers) placed two feet away from each other in horizontal and vertical axes (Figure 3.20).
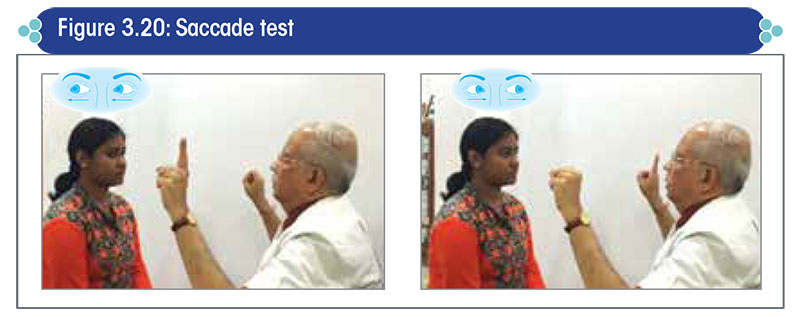
Observe the eyes for:
Any to-and-fro movement on reaching the target before fixation; look carefully if the eyes are overshooting or undershooting the endposition.
- Any oscillation
- An abnormality suggests the presence of a central vestibular lesion involving the cerebellum.
Brief examination of the neurological system
It involves the following assessments:
Test for deep tendon reflexes
Test for Babinski reflex
Muscle strength + sensory test of the face and limbs Oculomotor tests
Thorough examination of the balance system
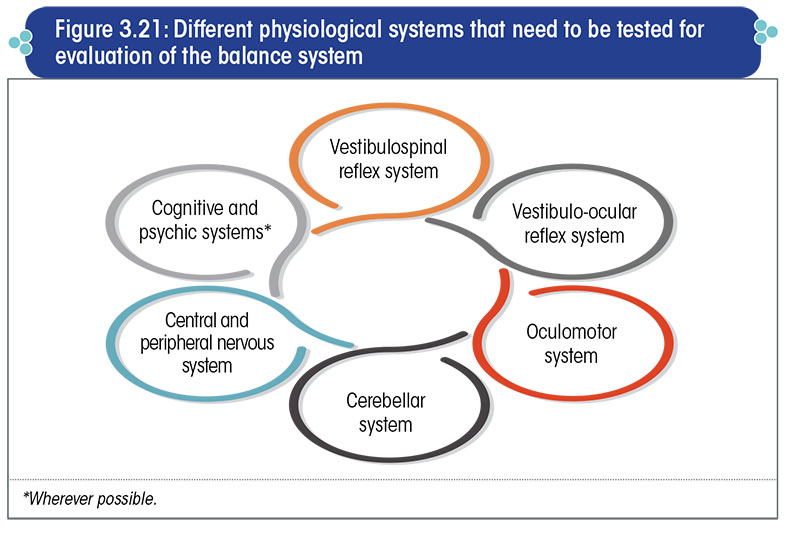
When investigating the balance system, it is important to ascertain the perfect functioning of certain physiological systems as well as the structural and functional integrity of the neural pathways (Figure 3.21).
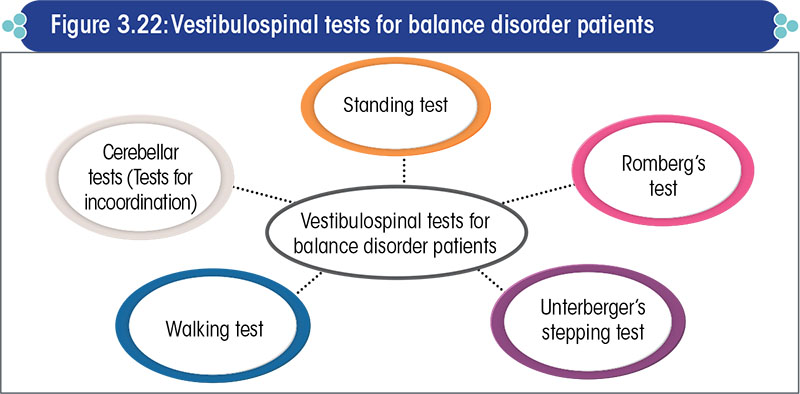
Vestibulospinal tests
These include tests to assess the functioning of the trunk and limbs (Figure 3.22).
Standing test
Method: Ask the patient to keep his feet together and hands extended in the front and stand upright
- On both legs with eyes open
- On both legs with eyes closed
- Alternately on one leg with eyes open and then, if possible, with eyes closed
The examiner must be prepared to support the patient in case of any unsteadiness or tendency to fall (Figure 3.23).
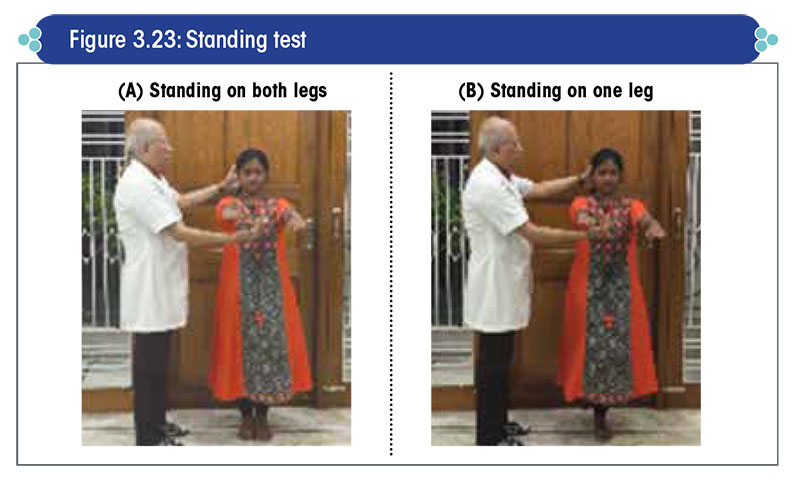
The examiner must take utmost care to hold the patient in case of any propensity to fall, and a fall must be prevented under all circumstances. Allowing a patient to fall is a criminal offence, and is tantamount to criminal negligence. This applies to all balance disorder tests.
Positive result: Any sway or tendency to fall is abnormal. Minor gyrations are not abnormal.
Modified standing test:
- The sensitivity of the standing test can be increased by asking the patient to stand upright on a foam pad, so as to further reduce the proprioceptive input.
- A person who can stand on one leg with eyes closed for 10 secs on a foam pad may be accepted to have a perfectly normal vestibular system for all practical purposes.
- However, this is a difficult test and an inability to perform this test does not necessarily suggest an abnormality in the vestibular system.
Romberg’s test
Although commonly thought to be a test of cerebellar disease, this is actually a test of proprioception. It tells us whether the proprioceptive input system is functioning properly or not.
In fact, in patients with partially advanced cerebellar ataxia, it is not even possible to perform the Romberg’s test as the patient will hardly be able to stand.
Method:
- The patient stands upright with his feet together and hands extended, and is then asked to close his eyes (Figure 3.24). The test can be further sensitized by asking the patient to stand with his feet tandem i.e., one foot in front of the other.
- The examiner should remain close at hand, in case the patient begins to sway or fall.
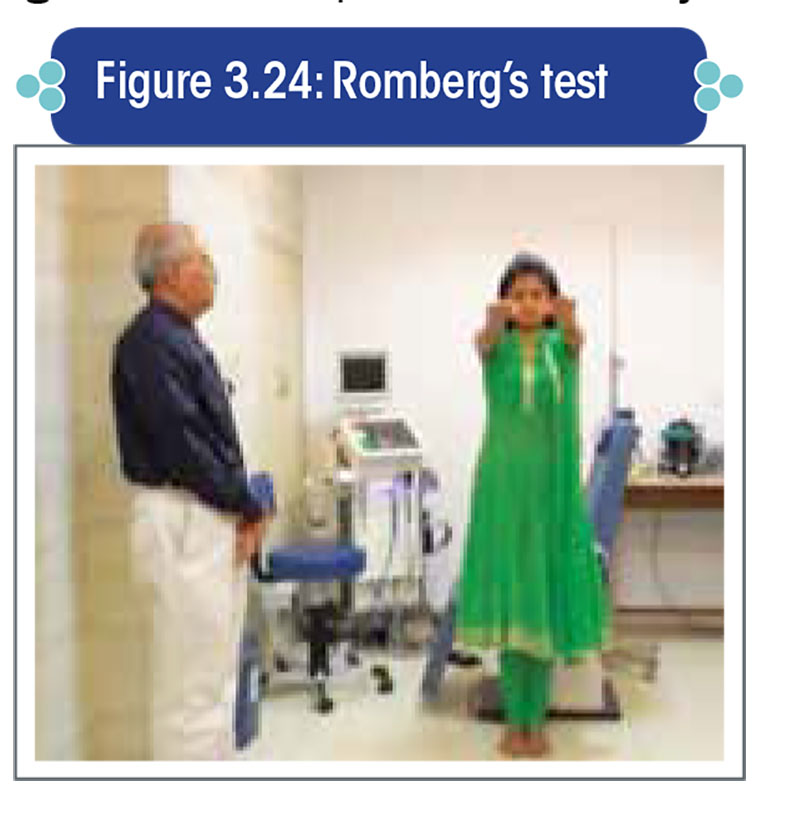
Positive result:
- A loss of balance without self-correction is interpreted as a positive Romberg sign.
- Gross swaying with correction is not a positive result.
Interpretation:
- A positive test is indicative of sensory ataxia caused by lack of proprioception, rather than cerebellar ataxia.
- Gross swaying may occur in cerebellar disease, but other features of cerebellar disease will be present.
Unterberger’s stepping test
Method: The patient is asked to keep his eyes closed and arms extended, and step on the same spot for 90 times in a span of one minute (Figure 3.25).
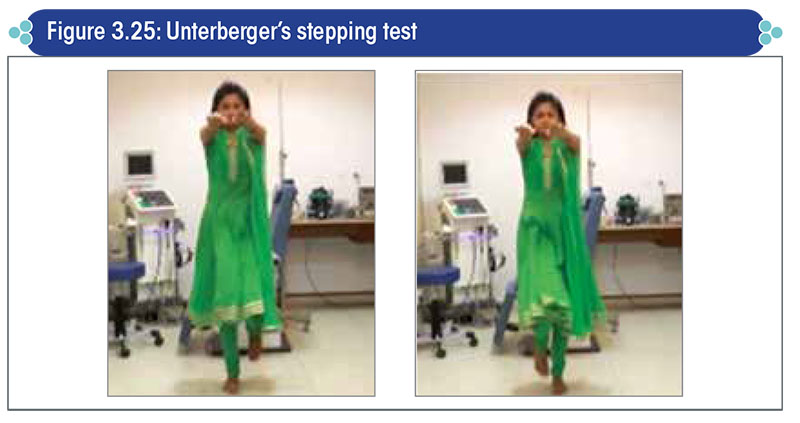
Positive result: Any rotation/deviation or abnormal side-to-side sway is a positive result.
In clinical practice, the standing test and Romberg’s test are usually combined.
Interpretation:
- Rotation/deviation by >50° to one side suggests ipsilateral peripheral vestibulopathy i.e., a peripheral vestibular lesion on the side towards which the patient deviates and/or rotates.
- Widened side-to-side sway with gradually widening base is a sign of ataxia due to a central lesion.
NOTE: In clinical practice, the standing test and stepping test are usually combined.
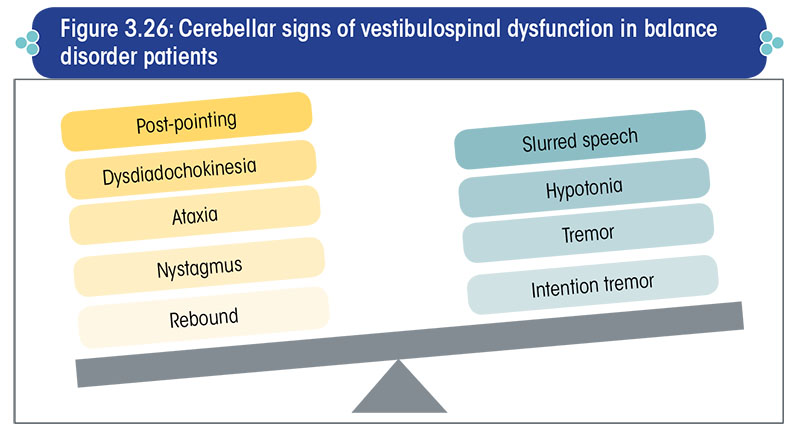
Cerebellar tests (Tests for incoordination)
Cerebellar signs indicative of vestibulospinal dysfunction
Cerebellar function needs to be very thoroughly tested in all patients presenting with a balance disorder.
Defects in the cerebellar system manifest as various signs that need to be picked up by the clinician.
The overall cerebellar signs suggestive of vestibulospinal dysfunction are summarized in Figure 3.26.
A cerebellar disorder is a common, although not the sole cause of ataxia/gait disorders.
Ataxia and gait disorders
Any clinician dealing with a balance disorder patient must have a thorough understanding of ataxia and gait/locomotion disorders.
Ataxia is marked by a lack of coordination of movement that involves contraction and relaxation of a group of muscles, harmoniously in a definite order.
It is a non-specific neurological sign of improper functioning of parts of the CNS that coordinate the movement.
An incoordination in muscular contraction hinders the smooth execution of any movement.
Since the cerebellum is the main instrument of the CNS to coordinate movement, any ataxia should first raise an index of suspicion for a cerebellar defect. A cerebellar disorder is a common, although not the sole cause of ataxia/gait disorders.
Gait is defined as the manner of execution of locomotion.
Ataxia is usually accompanied by defective locomotion, as locomotion involves the smooth, sinuous, alternate movement of the limbs for forward/backward propulsion of the center of gravity of the body in a harmonious manner.
Patients with ataxia and gait disorders often present to the clinician with complaints of unsteadiness/spinning, despite the absence of true unsteadiness/spinning, as most patients cannot distinguish between the two conditions.
Ataxia and abnormal gait must be recognized by the clinician when the patient walks into the clinic. The tandem walking test with eyes closed unravels any ataxia very easily.
The signs of cerebellar disorders are as under:
Abnormal posture
An abnormal posture is suggestive of either truncal ataxia or appendicular ataxia. In advanced cerebellar dysfunction, both, truncal and appendicular ataxia are observed.
Truncal ataxia is an impairment of the ability to perform smoothly coordinated voluntary movements.
- It may affect the limbs, trunk, eyes, pharynx, larynx, as well as other structures. Unequal steps or sudden stops when the patient is walking should arouse the suspicion of truncal ataxia.
- It results from dysfunction of the spinocerebellum (vermis and associated areas near the midline of the cerebellum), which is characterized by a wide-based ‘drunken sailor’ gait.
Appendicular ataxia, which also occurs in cerebellar disease, is incoordination of the limb movements.
- A patient with appendicular ataxia will have difficulty in performing daily activities like eating, drinking, brushing their teeth, writing, and/or typing. These have to be specifically asked for in patients presenting with unsteadiness.
- This condition is caused by dysfunction of the lateral hemispheres of the cerebellum, which specifically control coordination and movement of the extremities, including the arms, hands, legs, and feet.
Wide-based/unstable gait
Cerebellar gait or ataxic gait is a wide-based gait with lateral veering, unsteadiness, and irregularity of steps. It is often accompanied by a tendency to fall to one side, forwards or backwards.
The patient may have a staggering gait, often slow and unsteady, similar to that of a drunk person. In unilateral cerebellar disease, the patient can veer towards the side of the lesion.
Wide stance
A broad-based stance is noted in patients with cerebellar disease.
Slurred speech
Patients of cerebellar dysfunction usually have a characteristic slurred, staccato speech.
Tremor
Tremors are basically of two types viz., action tremor and resting tremor.
- Action tremor occurs only during active or voluntary movements of the body muscles (e.g., while raising the hand or lifting a cup towards the lips) and not when the limb is at rest.
- Resting tremor occurs even in the absence of any active or voluntary movement of the muscles i.e., when the muscle is relaxed (e.g., while resting the hand on the lap). It is a common symptom of Parkinsonism.
Intention tremor:
- In cerebellar disorders, there is usually a slow but high amplitude tremor that occurs only during voluntary movements (e.g., lifting a cup towards the lips) and increases in amplitude towards the end of the movement as the limb reaches the target.
- This type of action tremor is termed as ‘intention tremor’.
- It occurs as a rhythmic oscillation of the involved body part at a frequency of 3-5 Hz, and is evident in the finger-nose test or pastpointing test described below.
Orthostatic tremor:
- Orthostatic tremor is a very high frequency tremor of an unknown cause, which affects the legs on standing and compels the patient to either sit or start walking immediately.
- It is not one of the accepted signs of cerebellar dysfunction, as its cause is unknown; however, it is mentioned here as it is also a form of tremor that causes instability.
- Although unrelated to cerebellar disorder, orthostatic tremor must be looked for in vertigo/balance disorder patients. This is because orthostatic tremor is often reported by patients as vertigo, which may lead to misdiagnosis.
- It is physically felt by touching the legs of patients who complain of unsteadiness on sudden standing.
Dysdiadochokinesia
Caused by cerebellar dysfunction, dysdiadochokinesia is an impairment of the ability to perform movements exhibiting a rapid change of motion.
It is attributed to an inability to switch-on and -off the antagonizing muscle groups in a coordinated fashion as a result of hypotonia.
Tests for cerebellar dysfunction
The most important aspect in cerebellar tests is the clinician’s acumen of sensing and identifying any incoordination or lack of smoothness of movement.
The following tests are performed to assess cerebellar disease related to vestibulospinal dysfunction in balance disorder patients:
Finger-to-nose test
The finger-nose test is a measure of upper-extremity coordination. It ascertains whether there is any incoordination in the upper limbs.
Method: The patient holds out his index finger, alternatively extends his left and right arm fully to one side and then touches the tip of his nose. This sequence is repeated a few times (Figure 3.27).
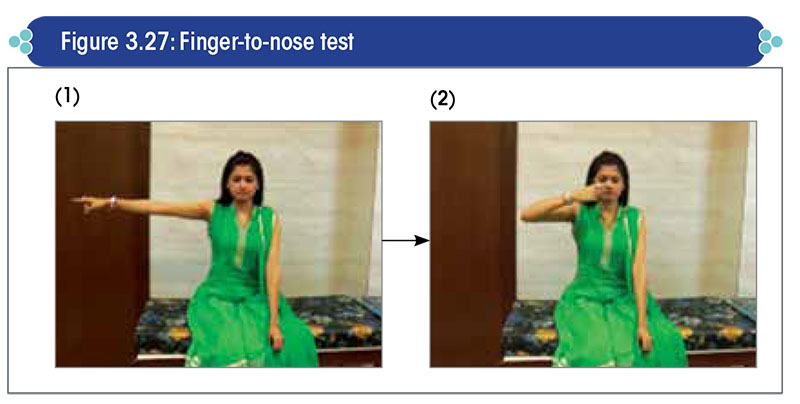
Positive result: Check for evidence of intention tremor (i.e., tremor at the end of the movement) or action tremor (i.e., tremor throughout the movement).
Heel-to-knee test
The heel-to-knee test evaluates lower-extremity coordination and position sense.
Method:
- With the patient lying supine, instruct him to place his right heel on the left shin just below the knee, and then slowly slide it down the shin to the top of the foot and back up again, as quickly and as accurately as possible (Figure 3.28).
- Have the patient repeat this maneuver on the opposite leg.
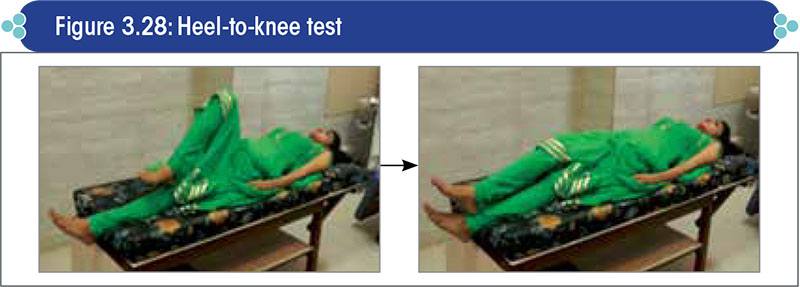
Lack of smoothness of movement while executing the finger-to-nose test (for upper limbs) or heel-to-knee test (for lower limbs) is a sign of poor coordination of motor activity, and is suggestive of a cerebellar lesion.
Positive result: Observe for inaccuracy of heel placement, and any deviation or jerking when sliding the heel down the shin.
Rapidly alternating task test
Method:
- The patient is asked to alternatively touch the palm and dorsum of one hand with the palm of the other hand, as rapidly as possible (Figure 3.29).
- This sequence is to be repeated a number of times.
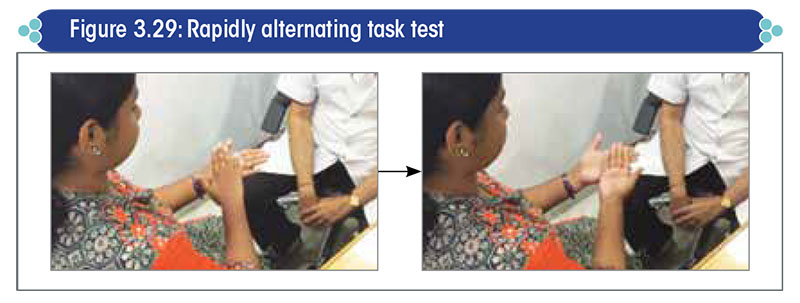
Positive result and interpretation: Check for any inaccuracy in performing the sequence, which indicates dysdiadochokinesia.
Rebound test
Method: Have the patient pull on your hand, and then suddenly let go off your hand (Figure 3.30).
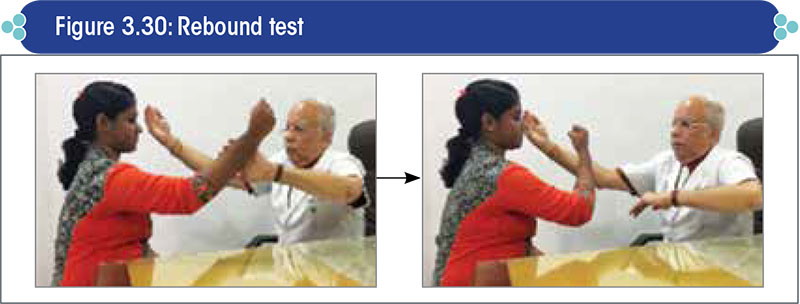
Positive result and interpretation:
- Normally, the antagonist muscles will contract and stop their arm from moving in the desired direction as soon as the opposing force exerted by the clinician is released.
- However, in cerebellar disease, this response is completely absent, which allows the limb to continue moving in the desired direction.
- Be careful that you protect the patient from the unarrested arm movement, causing them to strike themselves.
Tandem (‘heel to toe’) walking test
Method: Ask the patient to walk in a straight line with their heels to their toes, first with the eyes open and then with the eyes closed (Figure 3.31).

Positive result: Check for any deviation in the patient’s gait, any tendency to fall, unsteadiness, or irregularity/lack of smoothness while walking. Minor abnormalities are accepted as normal.
Interpretation:
- This is a very sensitive test and will exaggerate any unsteadiness.
- It is particularly sensitive at assessing the function of the cerebellar vermis, which is the first function to be affected in patients with alcoholic or other forms of cerebellar cortical degeneration.
Past-pointing test
Method:
- With the patient holding out his index finger, ask him to touch the examiner’s finger held ≈20 cm in front of the patient’s face and then the tip of his nose (Figure 3.32).
- This sequence is repeated a number of times, with the examiner changing the position of the finger each time.
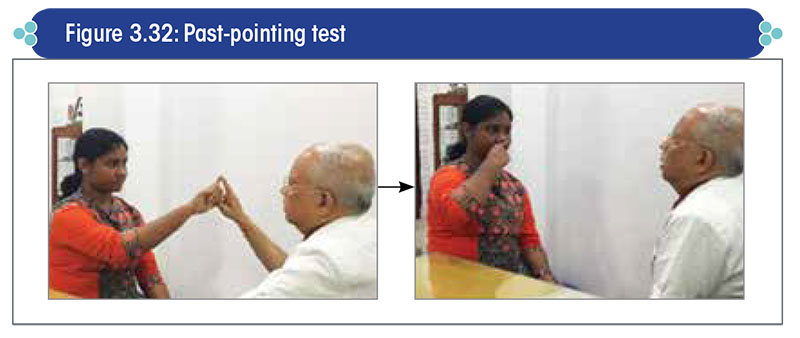
Positive result:
- Look for any tremor of the hand towards the end of the movement, and also whether the patient is able to perform the movements smoothly each time without wavering or faltering.
- In case of any wavering or faltering, check whether the subject is overshooting or undershooting the target.
Knee-jerk test
Method:
- Position the patient such that his lower leg is hanging freely off the edge of a bench.
- Using a reflex hammer, tap the patient’s patellar tendon, which lies just below the kneecap (Figure 3.33).
- Repeat and compare with the other leg.
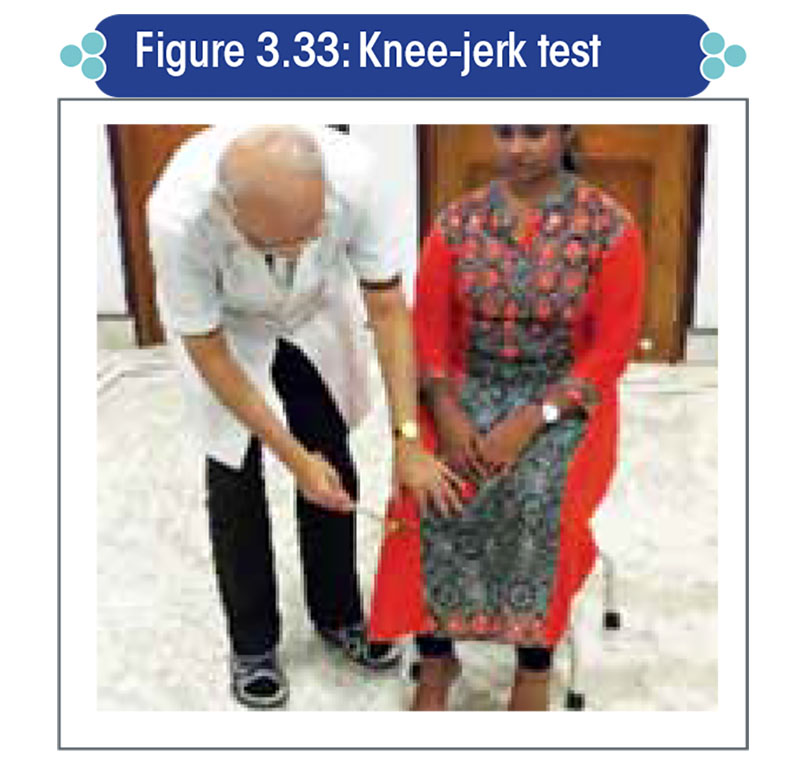
Positive result: The leg keeps swinging for more than four times after the knee jerk (‘pendular knee-jerk reflex’); three times or less is normal.
Interpretation: A pendular knee-jerk reflex is a sign of hypotonia, which suggests the presence of a cerebellar disorder.
Tests for extrapyramidal disorders
An extrapyramidal disorder is characterized by degeneration of some part of the extrapyramidal system, most commonly the corpus striatum, basal ganglia, substantia nigra, or subthalamic nucleus.
It causes slowness of movement, tremor, motor restlessness, irregular jerky movements, continuous muscle spasms, and muscle rigidity. All of the above conditions lead to unsteadiness/imbalance and, in some cases, head spinning, though the latter is difficult to explain.
The basal ganglia are believed to be involved in the control of posture, maintenance of resting muscle tone, generation of some spontaneous coordinated movements (e.g., swinging the arms while walking), initiation of movement (e.g., getting up from a chair to start walking), and certain facial muscular actions related to emotions such as frowning, laughing, crying, etc. These functions need to be assessed when evaluating the extrapyramidal system.
Anti-psychotic drugs and some other drugs like calcium channel blockers (e.g., cinnarizine and flunarizine) are notorious for inducing extrapyramidal disorders quite often.
Cinnarizine-induced Parkinsonism, the commonest form of extrapyramidal disorder, is pretty frequent in patients presenting to a vertigo clinic.
This is because drugs like cinnarizine are rampantly prescribed for prolonged periods by clinicians in many places, especially in India and the neighboring countries.
Whenever a continuous tremor or tremor at rest is seen, the clinician should always ask whether the patient is on cinnarizine or flunarizine or some antipsychotic medication.
The two widely recognized extrapyramidal disorders are chorea and Parkinsonism or Parkinsonian syndrome.
The former is an involuntary movement disorder with irregular movements of the trunk and limbs, which is not very common.
Parkinsonism patients often present with imbalance/falls, and are unable to adjust to any change of posture.
If suddenly pulled from behind, a normal person can easily adjust his posture and prevent a fall by stepping backwards by a step or two at the most; however, a patient of extrapyramidal disorder will fall backwards like an uprooted coconut tree.
Hence, postural imbalance is a marked feature in patients with extrapyramidal disorders. Such patients often present with unsteadiness, which is commonly reported as ‘head-spinning’ although there is no true spinning, as most patients cannot differentiate between unsteadiness and head-spinning. It is the clinician’s job to differentiate between the two conditions by asking leading questions.
If the clinician is callous and does not carry out a detailed clinical examination, the hapless patient will, in all probability, be prescribed drugs like phenothiazines (prochlorperazine) or cinnarizine that will only aggravate the disorder. This is very commonly encountered in clinical practice.
General inspection
Hypomimia (reduced facial expression)
Stooped posture (bent forwards)
Resting tremor (pill-rolling type)
- Tremor in Parkinson’s disease (PD) is ‘pill-rolling’ type. It appears as if the patient is rolling an imaginary pin between his thumb and index finger.
- A PD-associated tremor usually starts asymmetrically, commonly at the hands and/or feet.
- Later in the disease, the tremor may spread to all the four limbs, and sometimes the face (lips or chin) as well.
- Patients with drug-induced PD (e.g., after prolonged use of cinnarizine) generally present with a symmetrical tremor.
Dysarthria: It is marked by a slow, thick, indistinct, ‘Donald duck’-like speech.
Tongue spasticity: The tongue will appear stiff with reduced movement.
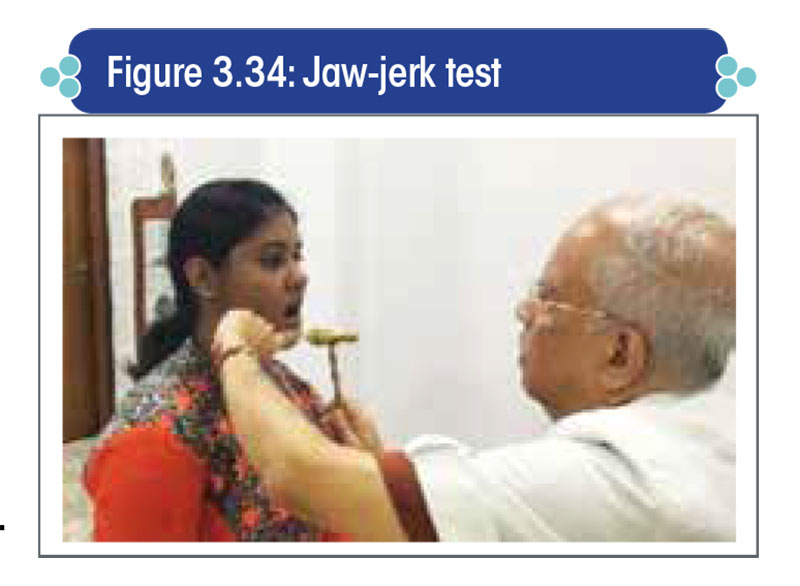
Brisk jaw jerk: It occurs due to hyperactivity of the cranial nerve V following upper motor neuron lesion.
- To elicit the jaw-jerk reflex, the patient is instructed to let his mouth fall open slightly and keep the jaw relaxed. The examiner places his index finger over the middle of the patient’s chin, and taps the finger with a reflex hammer, delivering a downward stroke (Figure 3.34).
- An exaggerated closure of the mouth is suggestive of an upper motor neuron lesion.
Pull test
It is a test for postural instability.
With the patient facing away from you and having explained what you are about to do, pull back hard on his shoulder so as to unbalance him (Figure 3.35).
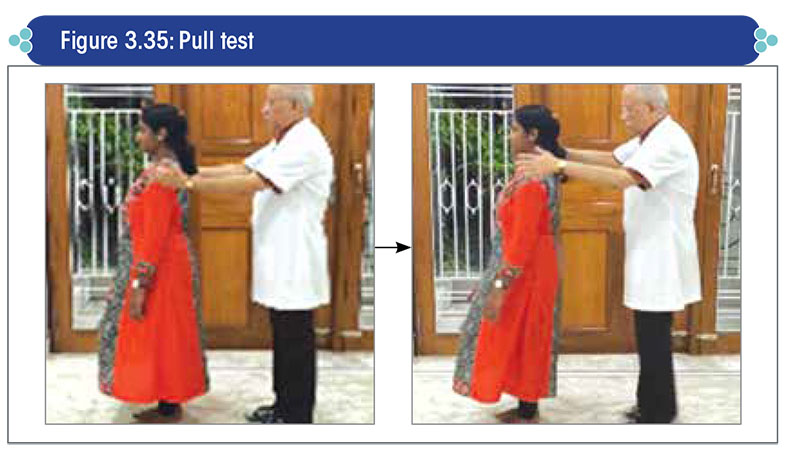
Normally, an individual will regain his balance by taking 2–3 steps backwards and will not fall. However, Parkinsonian patients often need to take more steps than these, or will fall back, as they have a very poor faculty of postural adjustment.
While performing this maneuver, stand close behind the patient and keep your hands by his shoulders without touching him, in order to prevent the patient from falling to the ground. A patient with an extrapyramidal disorder like Parkinsonism will, in all likelihood, fall backwards similar to a log of wood.
Gait test
Gait is evaluated by having the patient walk across the room, turn, and then walk in the opposite direction repeatedly under observation.
Check for
- Difficulty in initiating movement (hesitancy)
- Small, shuffling steps
- Festination (speeding up while walking)
- Reduced arm swing
- Turning en bloc
Cerebellar tests
The cerebellum is affected in multiple system atrophy (MSA) in patients with Parkinson-plus syndrome. MSA and spinocerebellar ataxia are two common causes of unsteadiness due to a cerebellar disorder.
Tests include finger-to-nose test, past-pointing test, and test for dysdiadochokinesia as described earlier. In case of a combination of both, extrapyramidal signs and cerebellar signs, chances are high that the patient is having a Parkinson-plus disorder.
Cognitive and psychic systems
In addition to the above tests, it is also important to assess the cognitive and psychic systems wherever possible, as these systems play a major role in the maintenance of balance.
If the clinician is not trained in psychology and/or psychiatry, evaluation of the cognitive and psychic systems can be done using a questionnaire prepared by a professional.
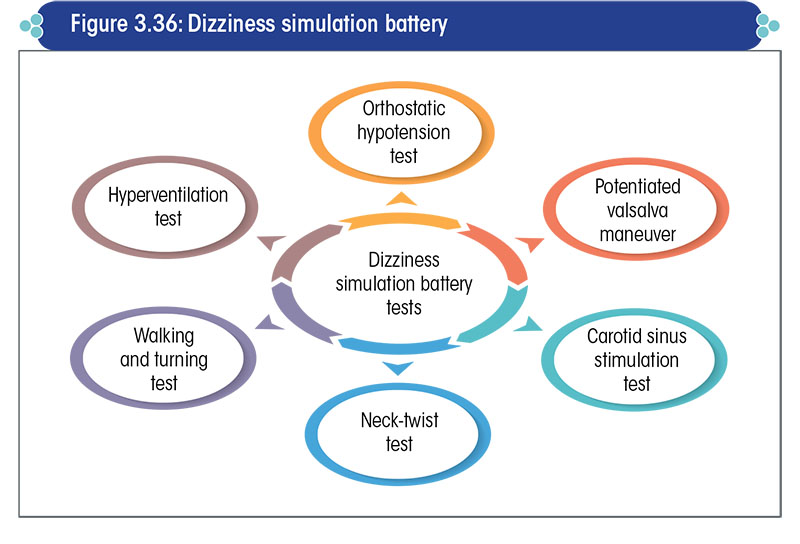
Dizziness simulation battery
It comprises of six tests, as enlisted in Figure 3.36.
Orthostatic hypotension
Measure the blood pressure (BP) of the patient
- In the supine position
- On immediate standing
- At three minutes after standing
A positive test is detected by a fall in the systolic BP by 20 mmHg or in the diastolic BP by 10 mmHg.
It suggests that the brain may be deprived of requisite blood due to a fall in BP, causing the patient to feel dizzy on suddenly standing up.
Potentiated Valsalva maneuver
Ask the patient to perform squats for 30 seconds, then stand and strains with closed glottis.
Carotid sinus stimulation
With the patient in the supine position (never in the sitting/standing position), unilaterally massage the carotid sinus for 15 seconds, and monitor the pulse rate.
Look for any irregularity or sudden fall in the pulse rate.
In case of any suspicion, refer the patient to a well-equipped cardiology unit (capable of cardiological resuscitation, if required) for electrocardiogram monitoring during carotid massage.
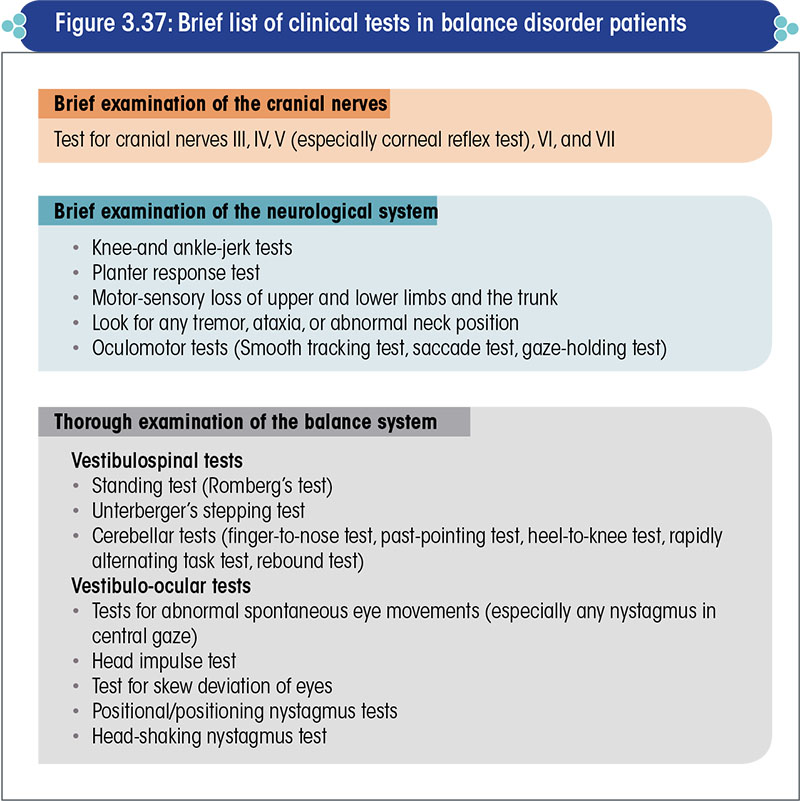
List of clinical tests in balance disorder patients
The brief list of clinical tests in balance disorder patients is presented in Figure 3.37.
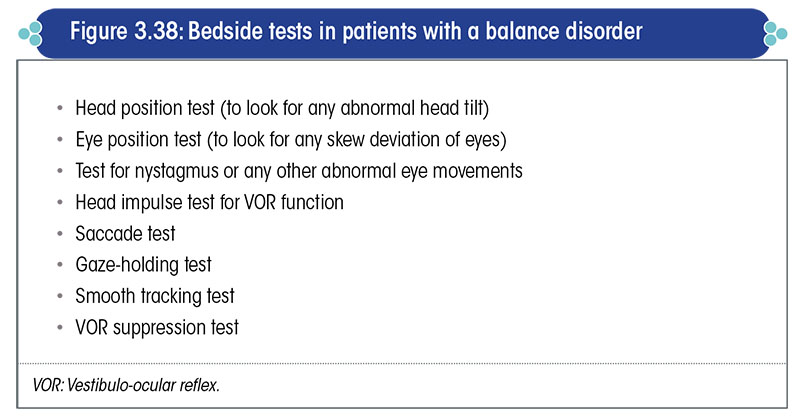
The bedside tests recommended in patients with a balance disorder are listed in Figure 3.38.
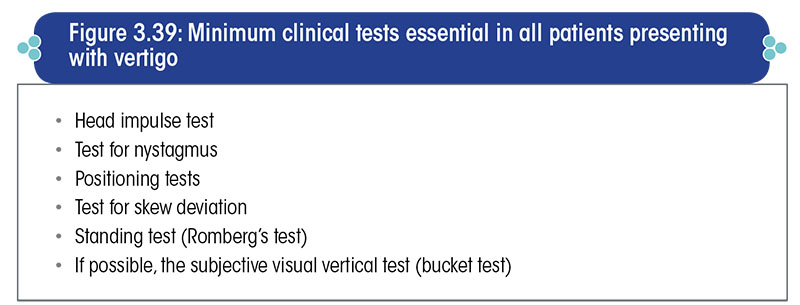
Minimum clinical tests essential in all patients presenting with vertigo are given in Figure 3.39.
Diagnostic investigations in vertigo patients: Role of modern vestibulometry
Vestibulometry – Where does it stand today?
Recent advances in neurotology
Neurotology is no longer an occult science whereby the site and nature of a lesion could not be diagnosed and therapy consisted of only camouflaging the symptoms of vertigo using anti-vertigo drugs, resulting in disastrous consequences.
The last 10-15 years have witnessed rapid developments in the field of neurotology, making it a completely evidence-based science, with accurate diagnostic techniques and highly specific therapies for all neurotological disorders.
Diagnostic significance of modern vestibulometry
Contemporary vestibulometry has enabled diagnosis of any abnormality in the vestibular system with utmost precision.
With the technology now available, we can accurately diagnose, for instance, whether
- There is a defect in the superior vestibular nerve of the left ear or in the utricle of the right ear.
- There is a poor gain of the vestibulo-ocular reflex (VOR) of the right anterior semicircular canal (SCC) or of the left posterior SCC.
- The latency of the saccadic eye movement is abnormally low.
- There is a poor VOR gain on left-to-right movement in the visual field, and at what speed of the movement does the oculomotor system fail in stabilizing the image in the visual field
Today, vestibulometry is a high-precision, scientific evidence-based reality. A lesion in any part of the vestibular labyrinths or the vestibular system can be diagnosed with pin-point accuracy.
Moreover, it is possible to exactly pinpoint the site of a lesion as well as document the extent of the lesion (e.g., whether there is a 47.8% deficit or 92% deficit of the maculo-ocular reflex from the macula of the left utricle), simply at the press of a button.
Thus, with the facilities available today, modern vestibulometry is a high-precision, scientific evidence-based reality.
Shift in patients’ perception
Now-a-days, patients have easy access to medical information on the internet, and can instantly find out whether the clinician has carried out the requisite diagnostic tests and on the basis of what scientific evidence has the treatment been prescribed.
In fact, most patients are willing to pay for the tests and, medicolegally, the doctor can be penalised if the necessary tests have not been conducted.
Failure to recommend the requisite diagnostic investigations in a patient is regarded as criminal negligence. Not suggesting necessary tests in an effort to save the patient’s money is utter foolishness, as the patient may use that money to sue the doctor legally on the ground that requisite diagnostic tests were not advised.
Objectives of modern vestibulometry
The objectives of modern vestibulometry are outlined in Figure 4.1.
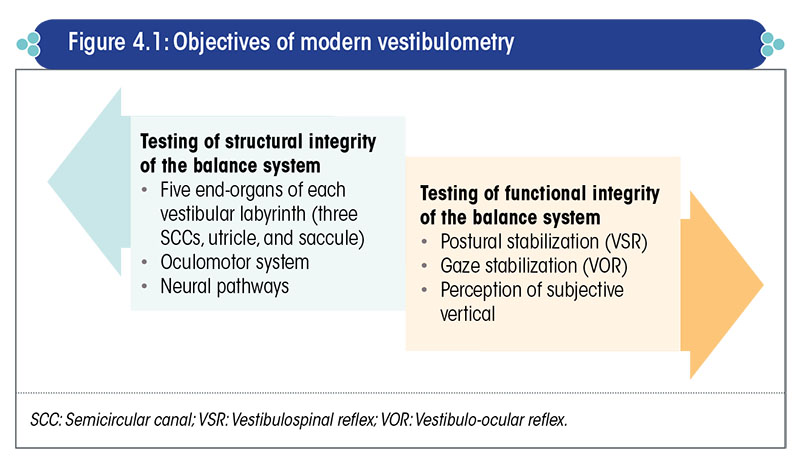
Each part of the two vestibular labyrinths has a specific function; a defect in any one of these parts can completely jeopardize the balance system, and cause vertigo or imbalance.
These 10 sense organs (five in each vestibular labyrinth) have to be evaluated separately and, when possible, at different frequencies of vestibular stimulation.
If one organ is normal, it does not imply that all the other organs are also normal.
Therefore, recommending a caloric test [electronystagmography (ENG)/videonystagmography (VNG)] alone is injudicious, as it evaluates only the lateral SCC and that too at a very low frequency of vestibular stimulation.
A patient with a normal lateral SCC can have a defect in the posterior SCC (at a high frequency of vestibular stimulation) or in the inferior vestibular nerve.
Hence, a test battery approach comprising all the vestibulometric tests is essential.
Diagnostic tools in modern vestibulometry
The different vestibulometric tests available today are listed in Figure 4.2.
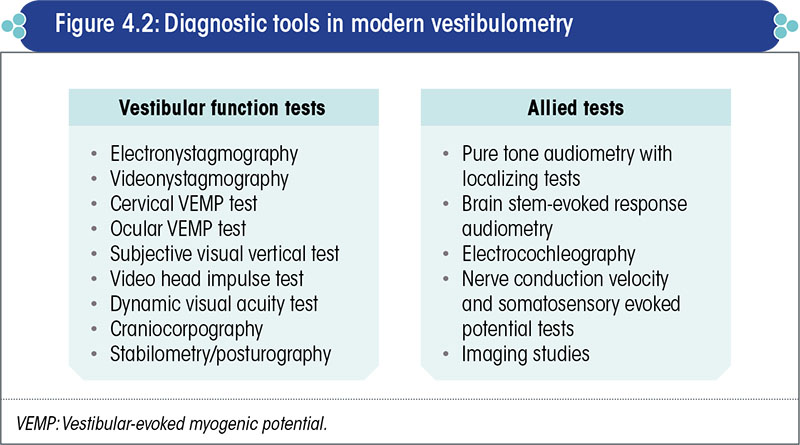
Each of these tests evaluates a specific anatomical part of the vestibular system or a specific function of the balance system.
None of these tests can be used as a standalone test or as a replacement for another.
It is important to adopt a test battery approach in order to accurately ascertain the structural and functional integrity of different organs that constitute the balance system.
Vestibulometric findings hold value only when each and every part of the balance system has been separately tested.
Ideal vestibulometric testing
The fundamentals of ideal vestibulometric testing are summarized in Figure 4.3.
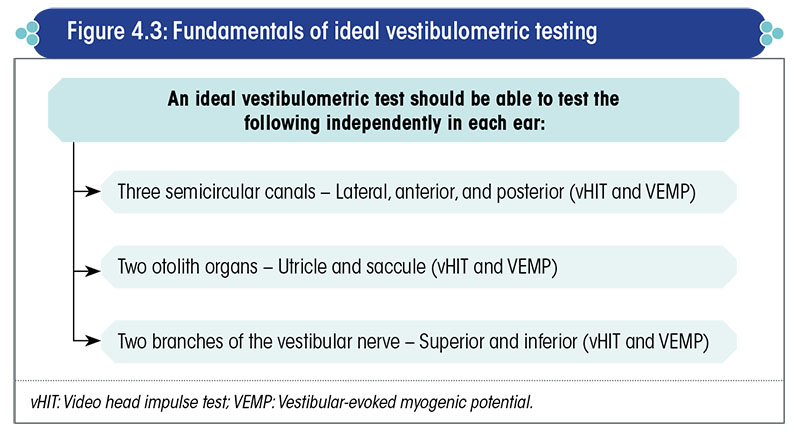
Evaluating the vestibular system is, no doubt, a time-consuming and complicated procedure. It requires the services of trained and dedicated medical professionals with adequate knowledge, insight into the subject, and in-depth understanding of the nuances of vestibular physiology in health and disease.
Nevertheless, by combining the video head impulse test (vHIT) and vestibular evoked myogenic potential (VEMP) test, the clinician can have a good working knowledge about the functioning of each vestibular part in a very short span of time (i.e., in not more than half an hour).
Specific tests for different anatomical parts of the vestibular system
Different vestibulometric tests evaluate specific anatomical parts of the vestibular system (Table 4.1, Figure 4.4).
Evaluation of vestibular response at different frequencies of stimulation
Each of the different tests of vestibular function evaluates the vestibular system at a specific frequency of vestibular stimulation (Figure 4.5).
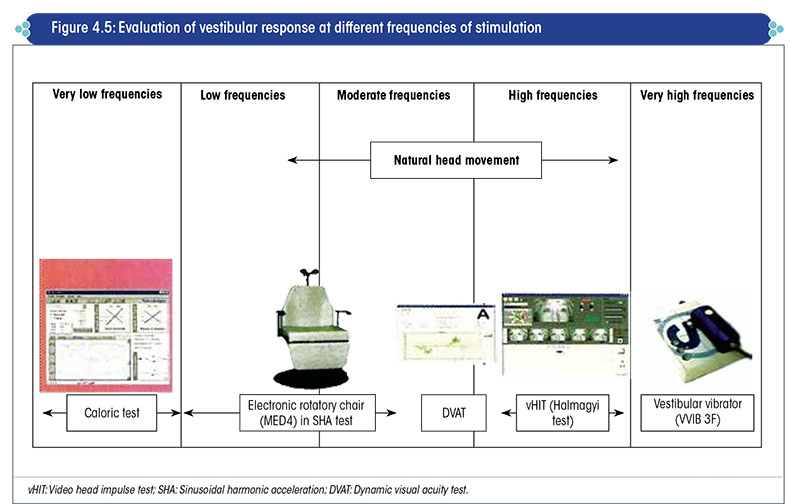
Natural head movements are the commonest form of vestibular stimulation in our day-to-day life, and occur at a frequency of 0.05-4.0 Hz.
Hence, to evaluate how the vestibular system can perform in our daily life, it is essential to test the system at least between the above frequency range i.e., 0.05-4.0 Hz.
The very popular caloric test, which was the only method of vestibular testing a decade and half ago, evaluates only the lateral SCC.
Moreover, the evaluation is done at a frequency of 0.005 Hz, 100 times lower than the minimum frequency of natural head movements.
It is surprising that this crazy, unphysiological, and cumbersome test has not only survived, but also dominated the field of diagnostic neurotology for more than a century.
No wonder, most patients with vertigo showed normal findings in the caloric test and vice versa. Moreover, many subjects with no vestibular problems whatsoever, who underwent the caloric test at some point of time, were found to have abnormal test results.
Contribution of the oculomotor system and VOR at different frequencies of head movement
The main purpose of evaluating the SCCs is to determine the gain of the VOR.
The function of the VOR is to move the eyes at a speed that is equal to the speed of the head movement when the head is suddenly moved.
Gain of the VOR is the velocity of eye movement divided by the velocity of head movement.
The speed at which vestibular stimulation occurs during caloric testing is not adequate to evoke the VOR.
- At such a slow speed of eye movement, it is only the oculomotor system, especially the smooth tracking system, that can maintain gaze stabilization.
- Hence, the caloric test does not even assess the VOR.
The contribution of different mechanisms to head impulse responses is illustrated in Figure 4.6.
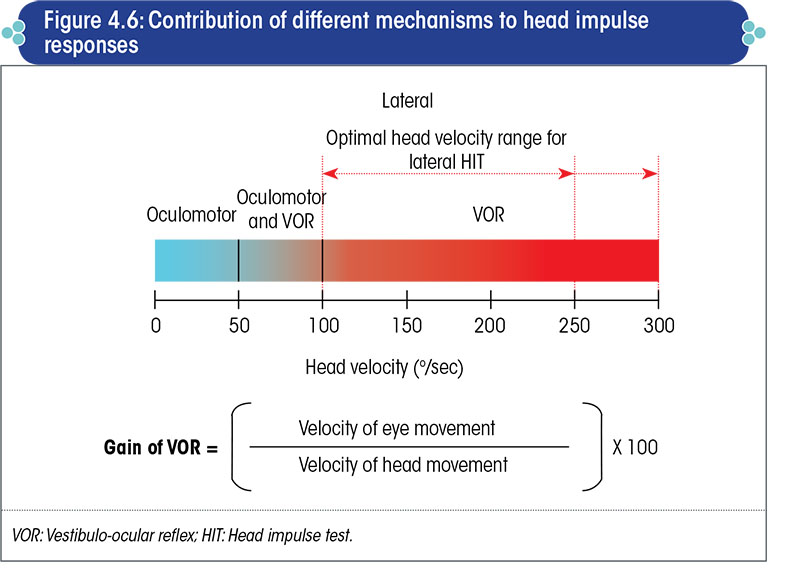
- Head impulse responses for head velocities below 50o/sec are mediated entirely by the tracking (smooth pursuit) mechanism of the oculomotor system.
- Both, the oculomotor and VOR mechanisms contribute to eye movement responses for head velocities between 50-100o/sec (the ratio varies as per age and other factors).
- Head impulse responses for head velocities above this are mediated entirely by the VOR.
- Therefore, to evaluate pure VOR, the speed of head movement should be above 100o/sec.
Standard ENG/VNG test battery
ENG/VNG testing evaluates:
- Oculomotor system (higher precision testing with VNG vs. ENG)
- Sensitivity of lateral SCC only
- Anatomy of the lateral SCC and superior vestibular nerve
It does not evaluate:
- Utricle
- Saccule
- Anterior and posterior SCC
- Inferior vestibular nerve
It tests lateral SCC at a very low frequency of vestibular stimulation.
The setup for ENG/VNG testing is depicted in Figure 4.7.

Although VNG is the most popular test in vestibulometry today, the caloric test portion of VNG – to which most importance is attached – is not informative at all and may soon be overtaken by other more informative tests.
Evaluation of the oculomotor system is a vital part of vestibulometry, and VNG is the best test to evaluate the same.
However, the caloric test part of VNG is overhyped and given too much undue importance.
- It tests only a very small part of the vestibular labyrinth, and the function it tests is not what we use in day-to-day activities.
- It is an unphysiological test which evaluates only the lateral SCC at a sub-optimal frequency.
Video head impulse test
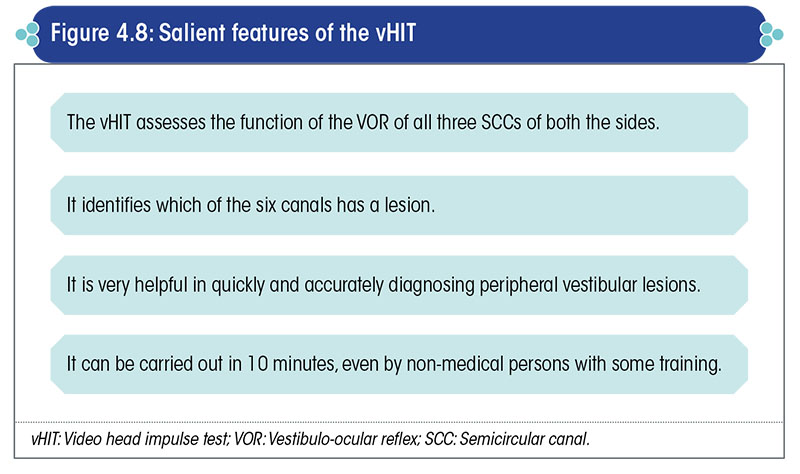
The video head impulse test (vHIT) incorporates a new technology that uses a pair of high-speed, light-weight video goggles to measure (left or right) eye velocity and record “catch-up” saccades (and other abnormalities) in patients with an impaired VOR.
vHIT provides a quick and objective measure of the VOR in response to head movements in the natural range of daily motions.
The vHIT evaluates the functional integrity of all the three SCCs in the vestibular labyrinth of side.
It can evaluate the VOR of each of these three SCCs at different high frequencies of stimulation, which closely match the range of frequencies at which normal head movements take place.
Hence, this test is much more relevant than the caloric ENG/VNG tests.
- The latter stimulates the vestibular labyrinth at an impractically low frequency that is nowhere near the frequency of vestibular stimulation during natural head movements.
- Furthermore, the caloric test part of ENG/VNG evaluates only the lateral SCC and not the superior and posterior SCCs.
The salient features of vHIT are given in Figure 4.8.
The setup and test protocol for the Ulmer vHIT is depicted in Figure 4.9.
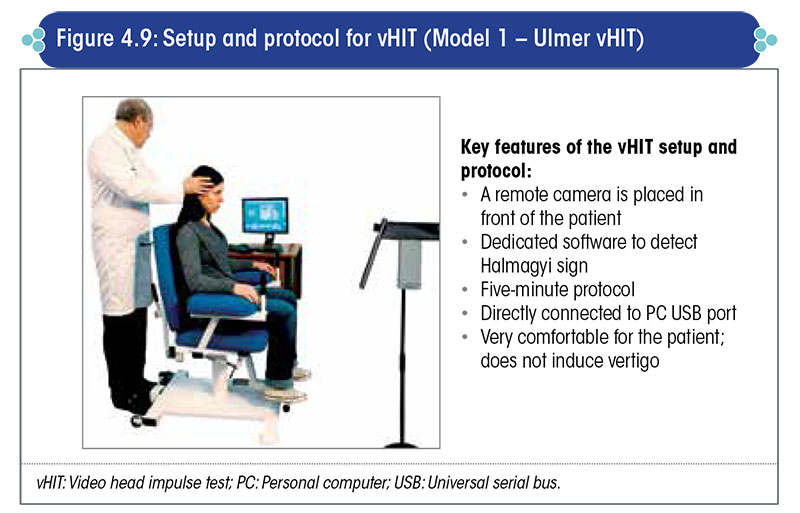
In this model, the clinician stands behind the patient and moves the patient’s head in the plane of the SCCs.
A remote camera records the head and eye movements.
The machine can record both, the speed of the eye movement and that of the head movement, and so the gain of the VOR (obtained by dividing the speed of the eye movement by the speed of the head movement) can be calculated for all the six SCCs.
Another type of model for vHIT ‘ICS Impulse’ is shown in Figure 4.10.
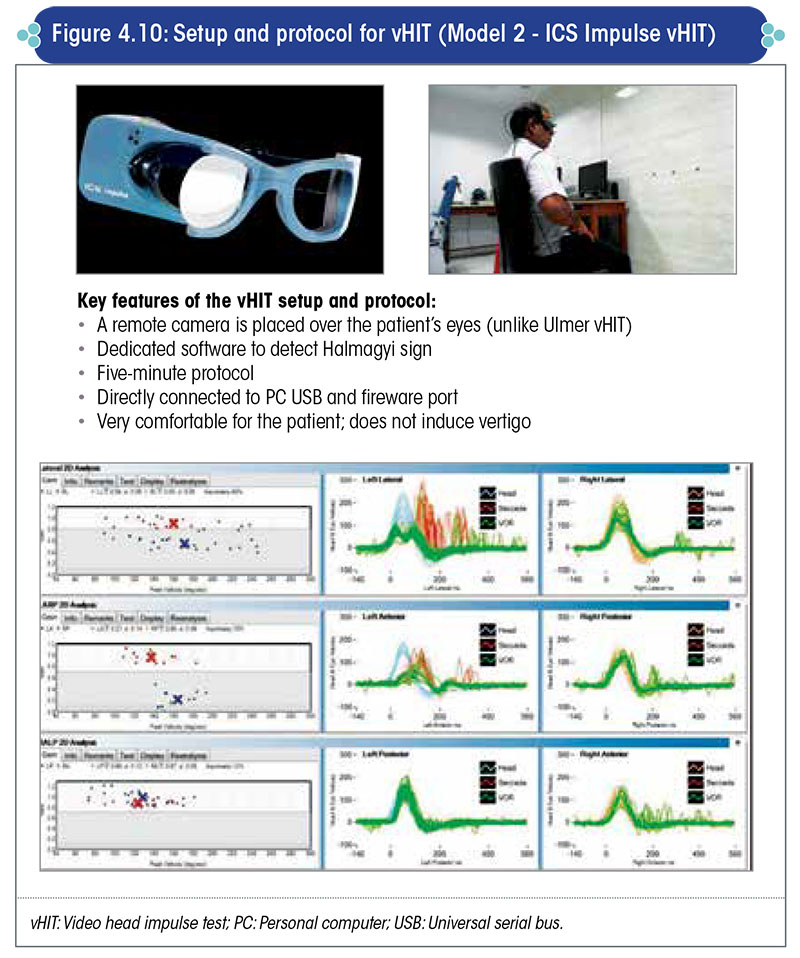
The remote camera, which is placed inside the goggles, records eye movements.
The goggles are worn by the patient. These goggles also house a gyroscope to record head movements. The clinician stands behind the patient and moves the patient’s head in the plane of each of the SCCs.
The software of the machine calculates the gain of the VOR of each SCC.
The speed of the eye movement divided by the speed of the head movement is the gain of the VOR. If both are equal, then the gain is 100%. If the gain is below 70%, then that particular SCC is supposed to be defective.
Subjective visual vertical test
The subjective visual vertical (SVV) test is done to evaluate the perception of the visual vertical.
In the SVV test, a roof mounted projector projects a straight line on the screen (Figure 4.11).
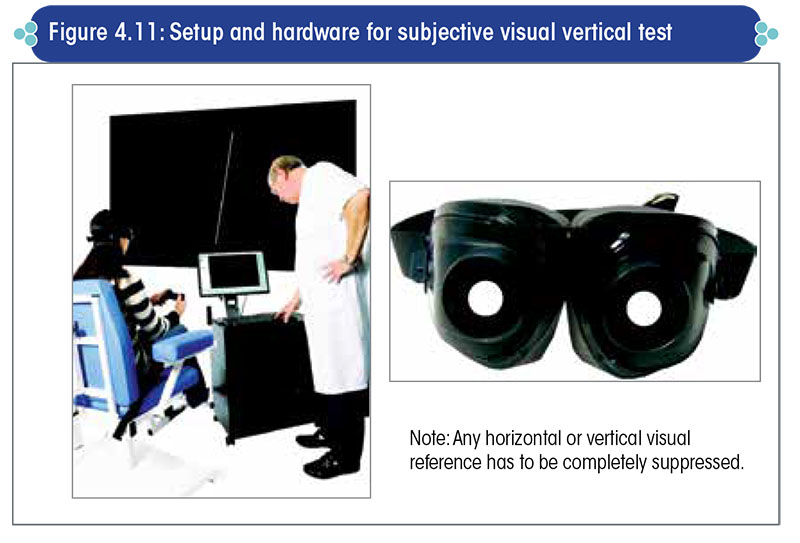
The machine’s software randomly changes the angle of the straight line, and the patient is asked to make the line vertical using a joystick.
A normal person is able to make this straight line vertical; in contrast, a subject with an uncompensated vestibular lesion will not be able to make it vertical and will deviate the straight line towards the side of the lesioned labyrinth.
The amount of deviation from the gravitational vertical is calculated by the machine’s software. Any deviation >2.5° from the gravitational vertical is considered abnormal and indicative of an uncompensated peripheral vestibular lesion.
This is a very easy and informative test.
For accurate orientation of the visual surroundings, the perceived visual vertical has to coincide with the gravitational vertical.
The perception of the visual vertical is believed to be a function of the otolith organs in conjunction with the cerebral cortex.
The vestibular system is instrumental in tallying the gravitational vertical with the visual vertical.
In uncompensated vestibular lesions, the visual vertical does not tally with the gravitational vertical and the visual surroundings appear tilted.
This peculiar sensation causes the subject to experience a feeling of imbalance. Similar to gaze stabilization and postural stabilization, the perception of visual vertical is also a function of the vestibular system.
The SVV test objectively identifies this vestibular defect.
The salient features of the SVV test are given in Figure 4.12.
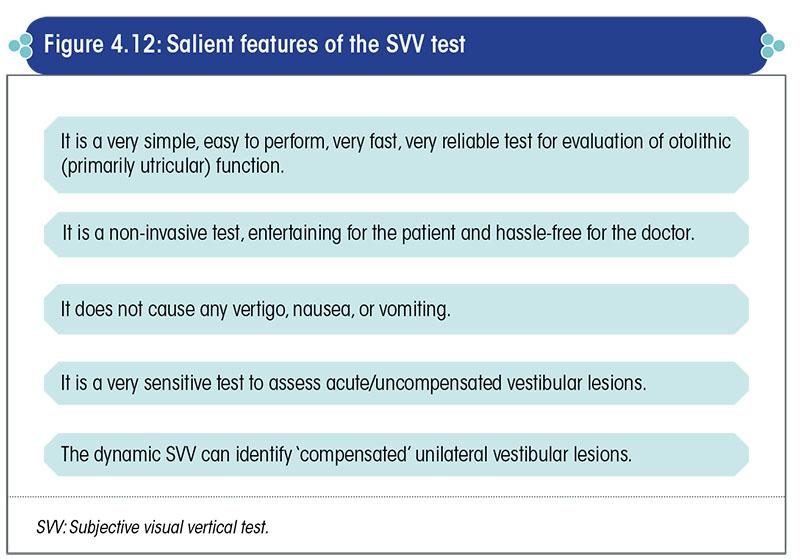
Two types of SVV tests are available viz., the static SVV and dynamic SVV tests.
The SVV measurement is a very important part of vestibulometry, as it is the only test to assess the perception of verticality, which is an otolithic function.
Static SVV test
In the static SVV test, the patient is asked to look at a vertical line projected on the screen.
A computer program tilts this vertical line at random repeatedly and using a joystick, the patient is instructed to make the straight line vertical i.e., tally it with the gravitational vertical. Ideally, there should be no difference between the perceived visual vertical and the gravitational vertical.
Normal persons and persons with a compensated vestibular lesion can do it within 0 to 2.5°, but patients with acute or uncompensated vestibular lesions cannot do so and invariably tilt the straight line towards the side of the comparatively weaker labyrinth (Figure 4.13).
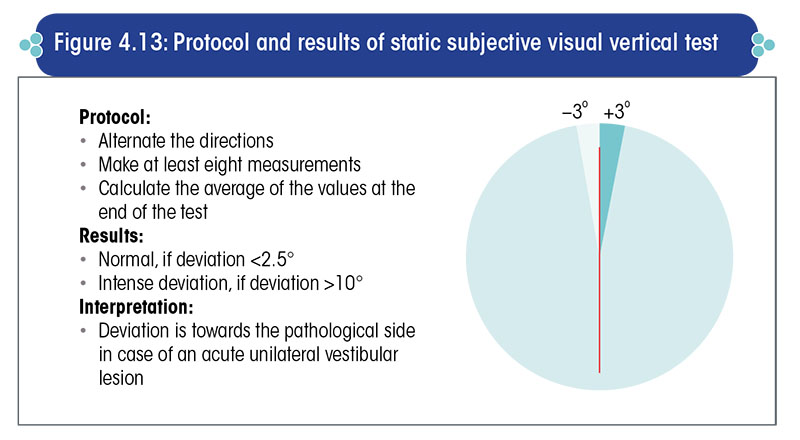
This test is very suitable for patients having acute vertigo as well as for small children, in whom a caloric test is not advisable.
Dynamic SVV test
In the dynamic SVV test, the patient is asked to make the projected straight line absolutely vertical while there is an optokinetic stimulation of the background in either clockwise or anticlockwise direction (Figure 4.14).
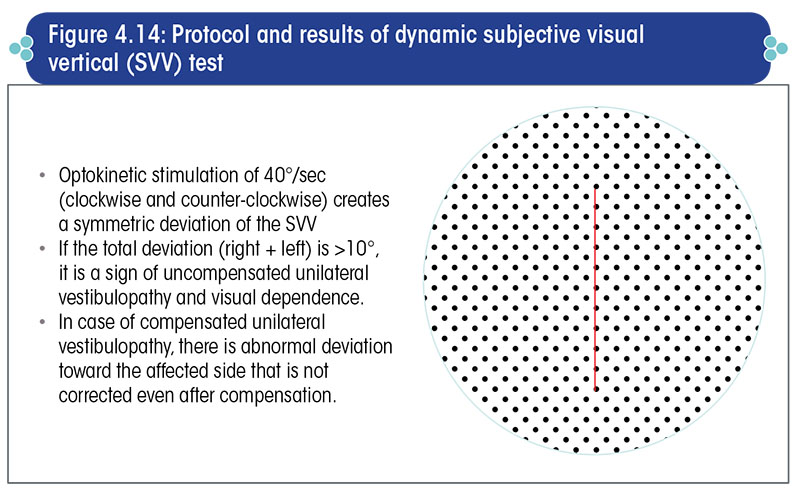
Apart from this, the overall test process remains the same as that for static SVV.
If the subject has a compensated unilateral peripheral vestibular lesion, then he will perform poorly during the dynamic SVV test i.e., he will not be able to place the straight line and coincide it with the gravitational vertical during the dynamic SVV test, but will be able to do so during the static SVV test.
Thus, this is a very good test to distinguish between compensated and uncompensated unilateral peripheral vestibular lesions.
Vestibular-evoked myogenic potential test
The vestibular-evoked myogenic potential (VEMP) test comprises two tests viz., ocular VEMP (oVEMP) and cervical VEMP (cVEMP). In both the tests, the otolith organs are stimulated by an auditory stimulus.
If the otolith organs are functioning normally, then this otolithic stimulation triggers a contraction of the extraocular muscles due to the VOR and a contraction of the skeletal muscles due to the vestibulospinal reflex.
Contraction of the extraocular muscles results from utricular stimulation which is recorded by the oVEMP test and contraction of the neck muscles results from stimulation of the saccule which is recorded by the cVEMP test.
oVEMP involves recording of the VOR or, more specifically, the maculoocular reflex, as the utricular macula is stimulated. In contrast, cVEMP involves recording of the vestibulospinal reflex, rather than the maculospinal reflex, as the saccular macula is stimulated.
Hence, a defect in the oVEMP is indicative of a utricular lesion and a defect in the cVEMP is indicative of a saccular lesion.
VEMPs are just another peep-hole into the very complex functioning of the vestibular system. They are not a replacement for other vestibular function tests (VFTs), and VEMP findings need to be analyzed in light of the clinical findings and other VFT findings like VNG, vHIT, craniocorpography, and posturography for relevance.
A VEMP is basically a myogenic response from the muscles of the neck or eyes, in response to loud acoustic stimulation of the otolith organs (viz., the saccule and utricle).
Otolithic sensitivity can be evaluated very simply by the VEMP tests.
Ocular VEMP
In the oVEMP test, an air conducted sound is presented to one ear, which stimulates the utricle of that side and induces a contraction of the extraocular muscles that is best picked up from the other side (Figure 4.15).
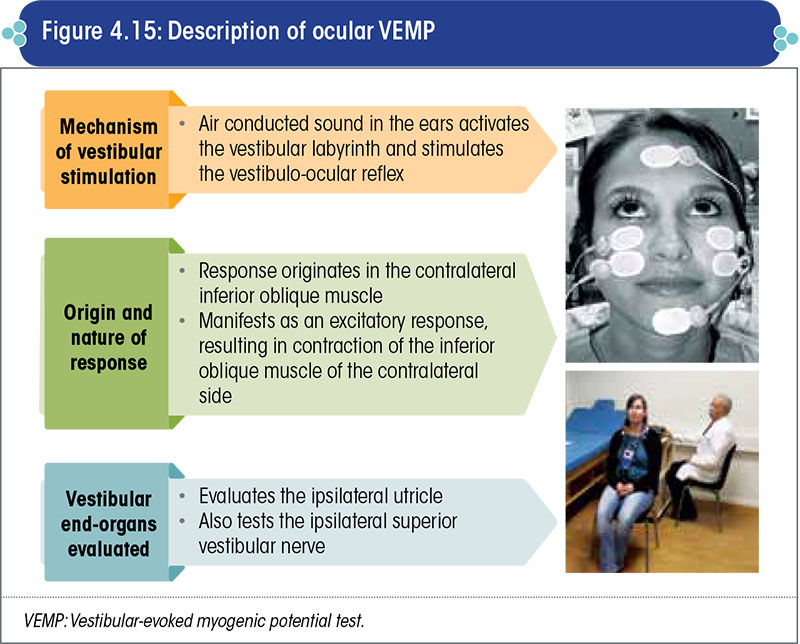
An electromyographic electrode is placed close to the inferior oblique muscle and contraction of the inferior oblique is documented. If the contraction is of sufficient strength, then the utricle is accepted to be functioning normally.
This is a quick, objective, and non-invasive test, but a very reliable test of utricular function.
Cervical VEMP
In the cVEMP test, an air conducted sound is presented to one ear, which stimulates the saccule of that side and induces a contraction of the cervical muscles that is best picked up from the sternocleidomastoid muscle of the same side (Figure 4.16).
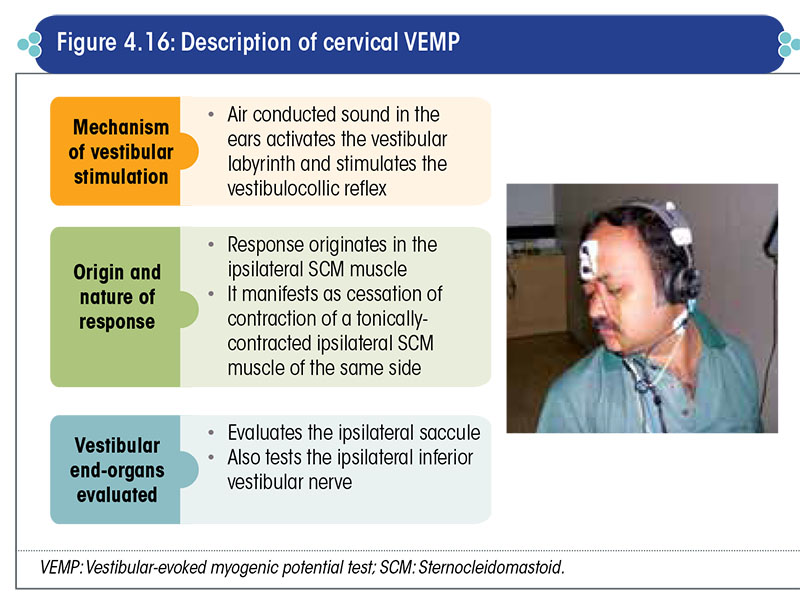
An electromyographic electrode is placed on the belly of the sternocleidomastoid muscle and contraction of the muscle is documented. If the contraction is of sufficient strength, then the saccule is accepted to be functioning normally.
Like oVEMP, cVEMP is also a quick, objective, and non-invasive test, but a very reliable test of saccular function.
VEMPs are very reliable, non-invasive, non-nauseogenic, and nonvertigenic tests of utricular and saccular function.
While ENG/VNG testing evaluates the ampullary function of the vestibular labyrinths, VEMP testing evaluates the macular function of the otolith organs.
Routine combined use of ocular and cervical VEMP, along with vHIT and VNG, helps in complete evaluation of the vestibular labyrinths.
Posturography
Posturography is an essential tool to document and qualitatively as well as quantitatively measure any instability in the patient.
Stabilometry can track changes in the center of gravity of the subject, when exposed to different external conditions, such as when the patient is made to stand on a hard surface with eyes open and then with eyes closed i.e., with normal proprioceptive and visual input, and then with normal proprioceptive input but no visual input (Figure 4.17).
- Additionally, it can track the center of gravity of the subject (by detecting any abnormal sway in the center of gravity) when the subject is made to stand on a soft surface with eyes closed (i.e., with reduced proprioceptive input and no visual input) and other such conditions.
- It is also useful for documenting the progress of the patient and the effectiveness of treatment.
Computerized dynamic posturography is an advanced test modality to ascertain the stability of a subject.
- In this test method, the visual and proprioceptive inputs can be manipulated, and the patient’s stability in different external conditions can be documented (Figure 4.18).
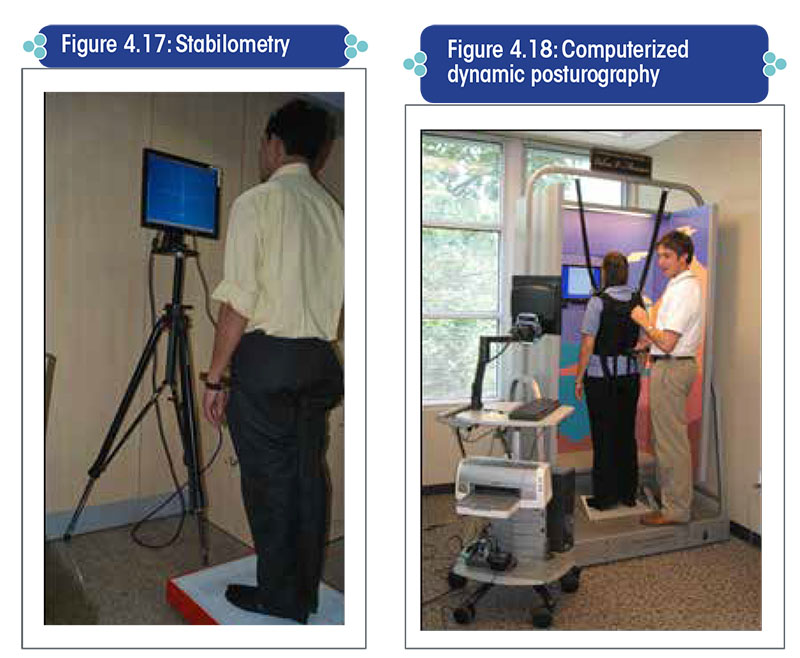
With the help of these tests, it is possible to determine whether postural control in a patient is visual-dependent or proprioceptivedependent, and accordingly tailor vestibular physiotherapy.
Key take-home messages
- Vertigo or imbalance is merely a manifestation/symptom of an underlying disorder that needs to be accurately diagnosed and treated.
- A very thorough history-taking and detailed clinical examination can lead to an accurate diagnosis of the underlying condition in more than 80% of the cases.
- In vestibulometry, a test battery approach is mandatory.
- Modern vestibulometry can diagnose the site and nature of a vestibular lesion with utmost precision and accuracy, provided it is carried out by the right person.
- Vestibulometric tests are only as good as the person performing the test and the clinician interpreting the results.
- Only tests carried out, or at least supervised, by a trained clinician with sufficient knowledge and insight in neurotology should be accepted. Tests that are not performed under the supervision of a clinician who is adequately trained in neurotology should be summarily rejected.